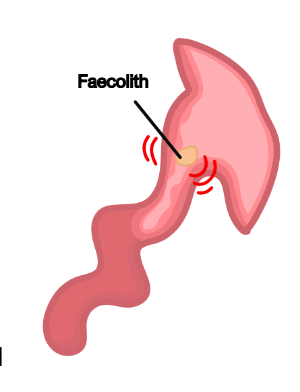
Acute Appendicitis
This refers to inflammation of the appendix. It is the most common cause of abdominal surgery in patients, which can occur at any age.
It occurs due to obstruction of the lumen commonly due to lymph hyperplasia (seen in children) or a feacolith (seen in adults).
Gut organisms then invade the appendix wall leading to oedema, ischaemia, and necrosis.
The inflammation irritates visceral fibres initially but then causes localised peritoneal inflammation in the right iliac fossa (RIF).
Symptoms
Migrating Periumbilical pain – right iliac fossa
Mild fever (37.5-38ºC) and anorexia
Infrequent Vomiting
Constipation (but diarrhoea can also occur)
Signs
Rovsing sign (palpating LIF caused pain in)
Psoas sign (pain extending hip if retrocaecal appendix)
Cope sign (pain on hip flexion if appendix closer to obturator internus)
Key tests
Blood tests show raised inflammatory markers (WCC and CRP)
If diagnostic doubt then do ultrasound, or CT scan if diagnosis still unclear
Management
Laparoscopic appendectomy, IV antibiotics
Large Bowel Obstruction
This is an obstruction of the large intestine, which shares similar features with small bowel obstruction.
Maximum diameter of large bowel is 6cm for colon and 9cm for the caecum (Small bowel = 3cm)
Causes
Colorectal cancer (most common)
Diverticular disease
Volvulus, adhesions and hernias
Symptoms
Constipation
Pain (more constant) and lower in abdomen
Distention (more than small bowel)
Vomiting (occurs later than small bowel)
Complications
If the ileocecal valve is competent, obstructed bowel will distend
This leads to a closed loop obstruction, causing vascular compromise
Caecum has the thinnest wall and is most likely point of perforation, leading to sepsis
Key tests
Imaging includes abdominal X-ray and CT scan
Management
Drip and suck if incompetent valve
If there is a closed loop obstruction, will likely require surgical management
Volvulus
This is a condition which is caused when the colon twists on its mesentery, cutting off the blood supply to the bowel.
This leads to obstruction of the bowel lumen and so can mimic bowel obstruction.
It usually occurs in two locations of the large bowel.
Sigmoid Volvulus
This is when the sigmoid colon rotates, compressing the vascular structures in the mesentery.
It is more common than caecal volvulus and occurs in elderly patients.
It is associated with chronic constipation, Parkinson’s disease and schizophrenia
Symptoms
Symptoms of large bowel obstruction
Key tests
Abdominal x-ray shows coffee bean sign, CT scanning is also used
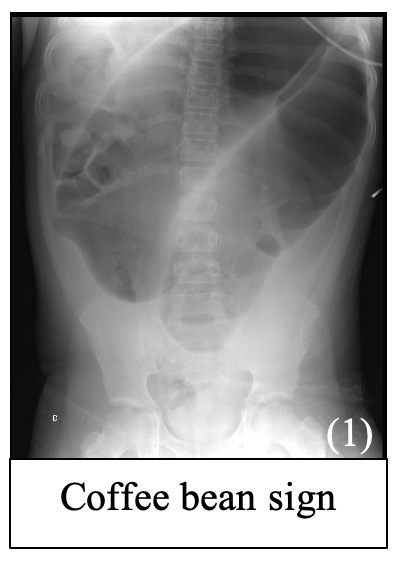
Management
Rigid sigmoidoscopy and rectal tube for decompression.
Patients should then be taken for elective surgical repair to prevent recurrence
Caecal Volvulus
This is rarer than sigmoid volvulus as the caecum lies in the retroperitoneal space.
But in some patients, the bowel becomes attached to the peritoneum during development allowing it to twist.
It is seen in people of all ages and associated with pregnancy.
Symptoms
Symptoms of small bowel obstruction (earlier vomiting, less distension)
Key tests
Abdominal x-ray shows embryo sign
Management
Usually right hemicolectomy
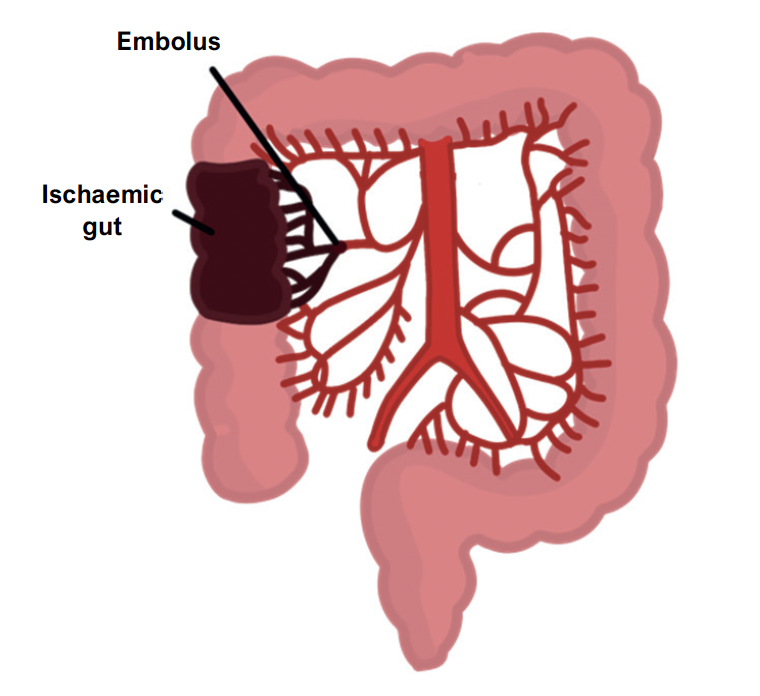
Ischaemic Gut
This is a generic term which describes a reduced blood supply to the bowel. It can be divided into 3 main types of bowel ischemia which share similar risk factors and symptoms.
Risk factors
Atrial fibrillation
Malignancy
Cardiovascular risk factors (smoking, BP, diabetes)
Symptoms
Abdominal pain
Rectal bleeding with diarrhoea
Septic signs – fever, elevated WCC with a lactic acidosis
Key tests
Blood tests show raised inflammatory markers and lactate
CT scan is the imaging of choice
In addition to these common features, the 3 types have some distinct aetiologies and features:
Acute Mesenteric Ischaemia
This describes an acute episode causing lack of blood supply to the bowel.
It is usually due to an embolism (due to atrial fibrillation) which blocks the superior mesenteric artery.
Symptoms
Classic triad of acute abdominal pain, no abdomen signs and rapid hypovolemia (shock)
Key is that the pain is sudden and not in keeping with the physical examination findings.
Management
Thrombolysis and anticoagulation
Surgery to remove dead bowel – can lead to septic peritonitis and septic shock
Chronic Mesenteric Ischaemia
This occurs due to atherosclerosis of the arteries supplying the bowel
It is more of a chronic condition seen in people with cardiovascular risk factors
Symptoms
Colicky abdominal pain that is intermittent and seen after meals
Leads to weight loss over time
Abdominal bruit can be heard
Management
Control vascular risk factors and stent insertion to vascularise gut
Ischaemic colitis
This is an acute reversible decrease in blood flow to the large intestine.
It usually affects splenic flexure which is at the border between the blood supply of the superior and inferior mesenteric artery.
It is also seen in young patients following cocaine abuse.
Symptoms
Acute lower left side abdominal pain and bloody diarrhoea
Management
Supportive management as it is transient – if no recovery then surgery
Bowel Perforation
This refers to a hole in the wall of part of the gut tube. This is very dangerous as it allows gut contents to enter the peritoneal cavity, which can quickly lead to infection.
This can rapidly deteriorate into septic shock and so has a very high mortality rate.
It can occur due to a variety of causes including trauma, iatrogenic (e.g., colonoscopy), bowel obstruction, ischaemia and a perforated peptic ulcer.
Causes
Trauma
Iatrogenic (e.g. colonoscopy)
Bowel obstruction
Ischaemia and infection
Symptoms
Acute onset pain over the abdomen worsened by movement
Nausea, vomiting and haematemesis
Sepsis – fevers, chills, hypotension
Abdomen is tense with guarding and rebound tenderness
After time, the abdomen will become distended and silent without bowel sounds
Key tests
CT is the imaging modality of choice
Erect chest X-ray will show free gas under the diaphragm
Management
Surgery to close the perforation, with IV fluids and antibiotics
Diverticulitis
This refers to inflammation of the diverticula, usually when one becomes infected.
Symptoms
Left iliac fossa pain, with nausea and vomiting
Change in bowel habit (can be constipation or diarrhoea)
Fever (peritonitis) and tachycardia
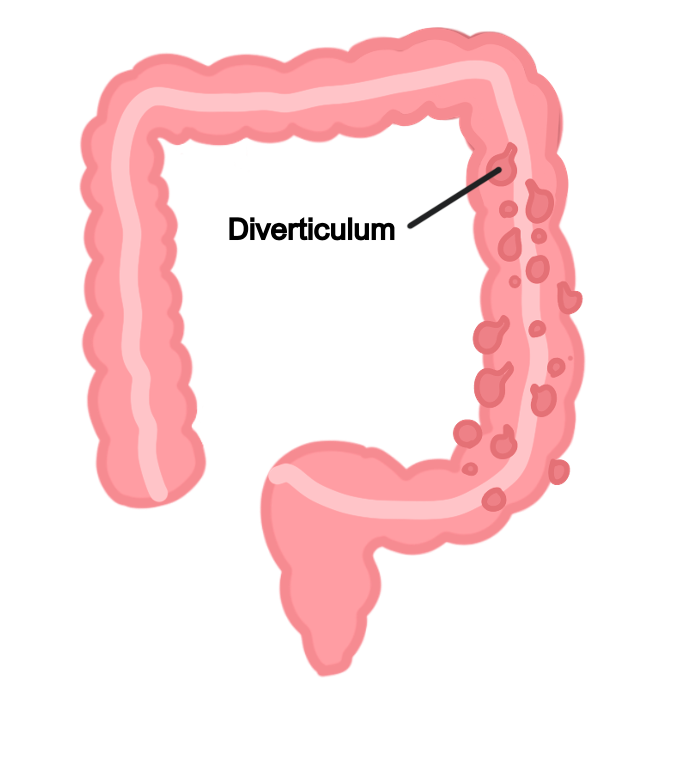
Key tests
Blood tests show raised inflammatory markers (WCC and CRP)
CT abdomen is the imaging of choice to confirm diverticulitis
Management
If mild, manage with oral antibiotics, fluids, and analgesia
If severe or symptoms last > 72 hours, consider hospital admission for IV antibiotics

