Coeliac disease
This is a condition characterised by T cell-mediated damage of the small bowel villi due to gluten exposure, which leads to malabsorption.
Gluten is found in wheat and grains and causes reduced mucosal absorption in the distal duodenum +/- proximal jejunum.
It is associated with HLA-DQ2 and HLA-DQ8, and onset has a bimodal prevalence pattern, presenting in childhood and again between 50–60 years.
If untreated, it can lead to T cell lymphoma of the small intestine.
Symptoms
Diarrhoea, bloating, abdominal pain
Steatorrhea, weight loss
Fatigue and failure to thrive
Hyposplenism
Anaemia secondary to iron, folate and vitamin B12 deficiency
Osteoporosis, osteomalacia
Associated conditions
Dermatitis herpetiformis, due to IgA deposition in dermis
Autoimmune thyroid disease
Type 1 diabetes
Irritable bowel syndrome
Lactose intolerance
Key tests
1st line is to check tissue transglutaminase (TTG) IgA and endomyseal antibody (IgA)
Patients should be on a gluten-containing diet for at least 6 weeks before the test
You should look at TTG levels in relation to overall IgA levels, as if the patient is deficient in IgA, then this can lead to a false negative result
If IgA deficient, repeat test for TTG with the IgG isoform and check HLA-DQ2 status
If the above is positive, definitive test is a duodenal biopsy. This shows villous atrophy, hyperplasia of the crypts and infiltration with lymphocytes.

Management
Dietary adjustment with gluten free diet
Pneumococcal vaccination every 5 years, as patients display hyposplenism
Whipple disease
This is a rare disease causing GI malabsorption, which occurs due to the bacteria Tropheryma Whippelli
These bacteria infect macrophages which compress lacteals resulting in fat malabsorption
Symptoms
Starts with arthralgia (pain of peripheral joints)
GI symptoms – Abdominal pain, weight loss, steatorrhea
Systemic symptoms – fever, sweats, cough
Skin symptoms – Photosensitivity and hyperpigmentation
Can involve CNS (dementia, seizures) and the heart (pericarditis)
Key tests
Jejunum biopsy – shows macrophages containing Periodic acid-Schiff (PAS) granules
Management
Antibiotics (e.g. Ceftriaxone followed by co-trimoxazole)
Abetalipoproteinemia
This is an autosomal recessive disorder due to a genetic mutation occurs in a transporter which leads to deficiency of apolipoprotein B-48 and B-100.
These apolipoproteins are needed for the synthesis of chylomicrons and VLDLs.
These are required to absorb fats. Therefore, this condition interferes with the normal absorption of fat and fat-soluble vitamins.
Symptoms
Fat malabsorption – steatorrhea (pale stools), failure to thrive, weight loss
Vitamin E (fat soluble) deficiency – gives cerebellar ataxia and peripheral neuropathy
Key tests
Blood test shows hypocholesterolaemia
Blood film shows acanthocytosis (spiked RBCs)
Management
Vitamin E supplements and high fat diet
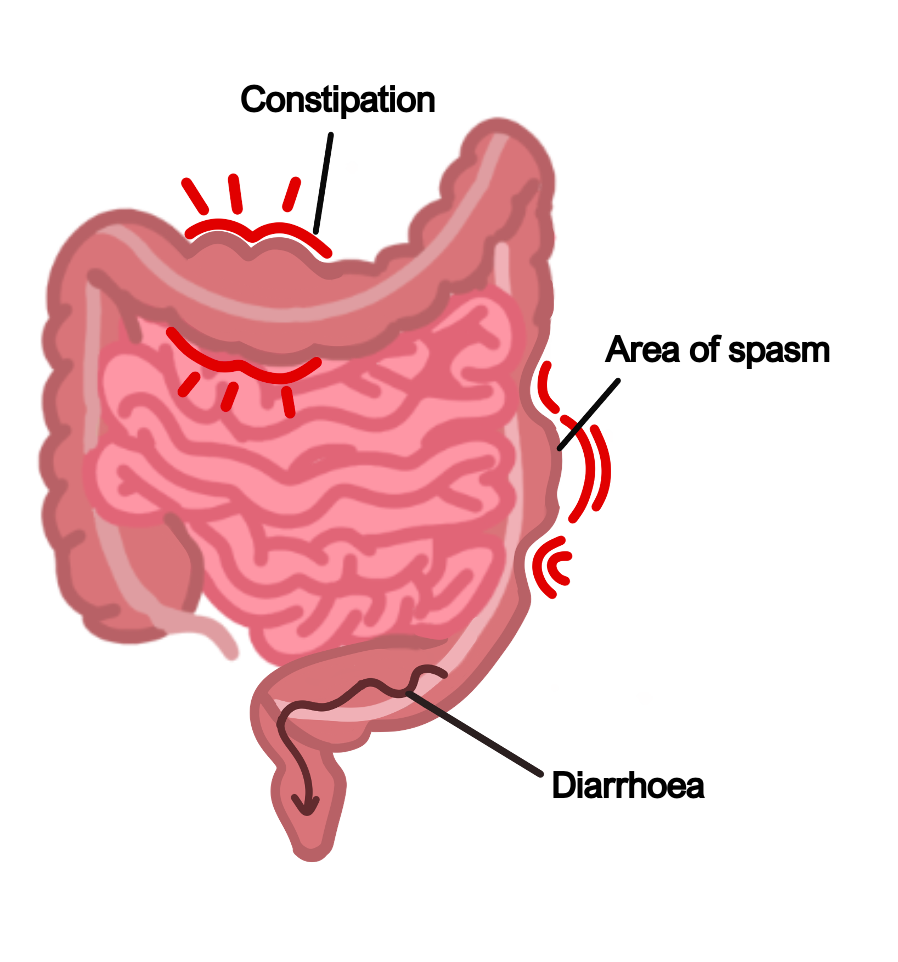
Irritable Bowel Syndrome
This is a multi-factorial condition associated with abdominal symptoms.
Patients may have chronic symptoms but blood tests and imaging will be normal.
Symptoms should be present for about 6 months to receive a diagnosis.
Symptoms
Abdominal pain, which is often relieved by defecation
Bloating – this leads to abdominal distention, usually gets worse after eating and can be triggered by particular foods
Change in bowel habit – either diarrhoea or constipation depending on the subtype
Management
1st line involves treating the most predominant symptom, e.g., pain with antispasmodic medication, constipation with laxatives or diarrhoea with loperamide
Other options include low dose amitriptyline or SSRIs
If no response to medication, can offer CBT or psychological therapy
Dietary advice includes avoiding trigger foods and having low FODMAP diet. These are carbohydrates which are poorly absorbed in the small intestine
Small Bowel Obstruction
This is an obstruction in the small intestine, preventing the passage of food/liquid through gut tube.
Causes
Adhesions – these are bands of fibrous tissue that form between organs and tissues, often due to previous abdominal surgery
Volvulus – this is the twisting of bowel with its mesentery, usually occurring in the sigmoid bowel (elderly) and caecal region (young adult)
Intussusception – this is when one part of the bowel slides into the next segment (like a collapsible telescope), which is more common in small children
Tumours – these can cause compression intramurally or from extrinsic compression
Strictures – these occur secondary to conditions like Crohn’s disease
Hernias – most are asymptomatic, but a few can result in bowel obstruction

Symptoms
Abdominal pain and distension
Unpredictable early vomiting
Constipation
“Tinkling bowel sounds”
Key tests
Abdominal X-ray and erect CXR are quick
CT scan is the best to establish the cause of obstruction and check for bowel perforation
Management
“Drip and suck” – keep the patient nil by mouth.
Insert nasogastric tube to drain the stomach contents and give IV fluids to rehydrate and correct electrolytes
Anti-emetics (not prokinetic metoclopramide)
If it is unresolving, secondary to strictures/tumours or there is evidence of bowel ischaemia/perforation, then surgery may be required
Carcinoid Tumours
This refers to a proliferation of enterochromaffin cells (neural crest origin), which usually occurs in the small bowel.
The tumour cells contain neurosecretory granules and often secrete 5-HT.
Serotonin is released into portal circulation and excreted in the urine as 5-HIAA.
These primary tumour sites can cause complications such as bowel obstruction, appendicitis and intussusception.
The main problem occurs when the tumour metastasises to the liver.
This allows 5-HT to enter the systemic circulation. This leads to carcinoid syndrome, which is often triggered by alcohol and emotional stress stimulating 5-HT release.
Symptoms
Flushing of the face, diarrhoea and bronchospasm
Hypotension
Right sided heart valve fibrosis – tricuspid regurgitation, pulmonary stenosis
Paraneoplastic syndromes due to hormone release e.g., ACTH, insulin, TSH
Key tests
Raised urinary 5-HIAA, raised blood chromogranin A (a neuroendocrine marker)
CT abdomen and pelvis to visualise the tumour and liver metastases
Management
Octreotide counters the peripheral effects of carcinoid syndrome
Surgical management involves resection of the tumour

