Oesophageal web
This is the protrusion of oesophageal mucosa, usually in the upper oesophagus.
It is a risk factor for the development of oesophageal squamous cell carcinoma.
It is associated with Plummer-Vinson syndrome, a triad of dysphagia, iron deficiency anaemia and oesophageal web.
Symptoms
Dysphagia (to solids more than liquids)
Can increase risk of aspiration and nasopharyngeal reflux
Management
Endoscopic dilation of the oesophagus
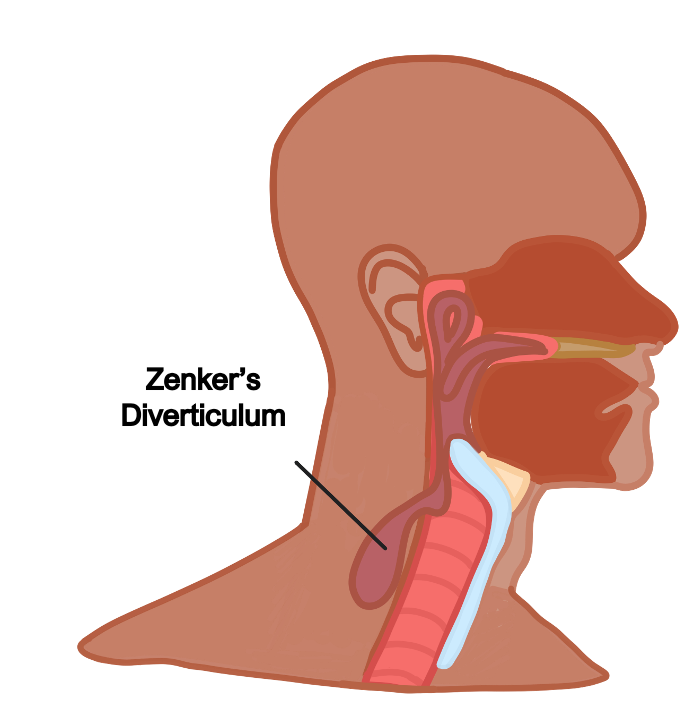
Pharyngeal pouch (Zenker diverticulum)
This is a pouch at the back of the throat, thought to be due to over-tightening of the cricopharyngeus muscle, causing the pharyngeal mucosa above it to pouch out.
It arises at the junction of the pharynx and oesophagus.
Symptoms
Dysphagia, neck swelling
Regurgitation of food, halitosis (bad breath)
Can present as multiple recurrent aspiration pneumonias
Key tests
Barium swallow and endoscopy
Management
Surgical correction
Mallory-Weiss syndrome
This is a longitudinal laceration of the mucosa at the gastroesophageal junction
It is usually caused by severe vomiting and so associated with conditions like alcoholism or bulimia
Symptoms
Gives normal vomiting followed by a small amount of blood with pain
There might be a history of the associated condition e.g. cycles of vomiting and binge eating
Management
In this case, treatment is supportive and persistent bleeding is uncommon.
However, if persistent, take to surgery for embolization of artery or open repair
Boerhaave Syndrome
This is a syndrome which is caused by persistent vomiting
It gives a rupture of the oesophagus which causes severe thoracic pain and can lead to air entering the mediastinum
Symptoms
Triad of Vomiting, thoracic pain, Crepitations (subcutaneous emphysema)
Management
Endoscopic or open surgery to repair oesophagus
Globus Hystericus
This is a persistent feeling of a lump in the back of throat making swallowing difficult.
It is associated with history of anxiety and stress, and there is usually no systemic upset to the patient
Symptoms
Intermittent dysphagia which is relieved by swallowing. No anaemia, vomiting or red flag symptoms
Management
Address anxiety, if pain or red flag symptoms investigate further with endoscopy
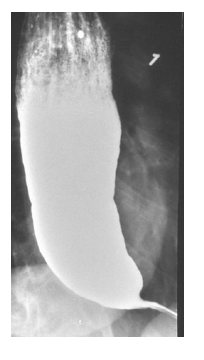
Achalasia
This is an inability to relax the lower oesophageal sphincter, due to damage to the neurones in the myenteric (Auerbach’s) plexus, usually seen in middle age.
Causes
Idiopathic
Malignancy
Infection, e.g., Chagas disease due to Trypanosoma cruzi
Symptoms
Dysphagia to both liquids and solids from the start
Heartburn and regurgitation of food (giving aspiration pneumonias)
Key tests
Barium swallow shows bird-beak sign, a dilated tapering oesophagus
Manometry can also be used to assess the motor function of the upper oesophageal sphincter (UES), oesophageal body and lower oesophageal sphincter.
A catheter is passed from the nose into the stomach.
It is then slowly withdrawn, allowing it to detect pressure changes.
In achalasia, it shows increased lower oesophageal sphincter tone.
Management
Calcium channel blockers/nitrates to relax sphincter
Botulinum toxin can be applied intra-sphincter to relax the smooth muscle
Endoscopic balloon dilation
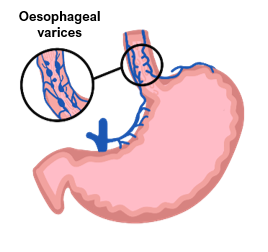
Oesophageal varices
These are dilated submucosal veins which occur in the lower part of the oesophagus.
They occur secondary to portal hypertension in liver cirrhosis.
High portal pressure causes the left gastric vein to back up into the oesophageal veins, causing dilation of these veins.
On their own they are asymptomatic.
However, they have a high risk of rupture.
This causes painless haematemesis with large volumes of fresh blood
If left untreated, it can be fatal.
Acute GI bleeding gives a disproportionate rise in blood urea compared to creatinine.
Management
Acute bleed
ABCDE approach with fluid resuscitation
Terlipressin (ADH analogue) and prophylactic antibiotics are also given
Definitive first-line treatment is endoscopic band ligation to stop the bleeding
If bleeding continues, use balloon tamponade with Sengstaken-Blackemore tube
If persistent bleeding, consider transjugular intrahepatic portosystemic shunt (TIPS)
Chronic management
Beta-blockers to reduce portal hypertension, e.g., carvedilol/propranolol
Endoscopy for surveillance and band ligation
Oesophageal carcinoma
A malignant proliferation of oesophageal cells subdivided into adenocarcinoma and squamous cell carcinoma:
Adenocarcinoma
This refers to a malignant proliferation of glandular cells, arising near the gastroesophageal junction.
It can be preceded by a condition called Barrett’s oesophagus, which refer to metaplasia of mucosa from stratified squamous to columnar epithelium.
High acidic stress in GORD can worsen Barrett’s oesophagus.
Squamous cell carcinoma
This refers to a malignant proliferation of squamous cells, usually arising in the middle third of oesophagus.
Risk factors include alcohol intake, smoking, achalasia and oesophageal web.

Symptoms
Progressive dysphagia
Weight loss and anorexia
Vomiting
Melaena, haematemesis
Retrosternal central chest pain
Cough and hoarseness of voice due to compression of trachea and recurrent laryngeal nerve
Key tests
Endoscopy with biopsy is investigation of choice
Endoscopic ultrasound provides local staging. CT is used to look for metastases
Management
Oesophagectomy with adjuvant chemo/radiotherapy is the definitive management which removes the tumour and creates an oesophagus-gastro anastomosis.
If patients are not fit for surgery, patients can be offered palliative chemotherapy, stenting of the oesophagus as well as options for artificial feeding, e.g., PEG feeding

