Acute Liver Failure
This term is used to describe an acute decrease in hepatocyte dysfunction.
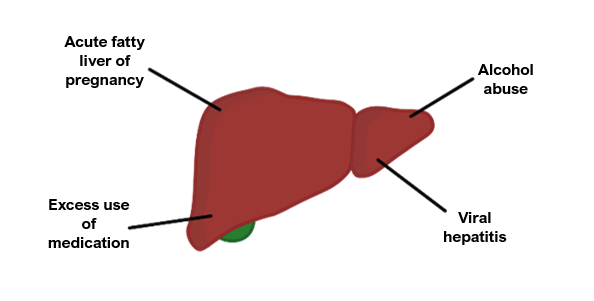
Causes
Drugs, e.g., paracetamol overdose, excess alcohol consumption, medicine reaction
Infections, e.g., hepatitis A/B
Trauma
Symptoms
Jaundice due to hyperbilirubinaemia
Coagulopathy due to decreased hepatocyte synthetic function
Oedema
Hepatic encephalopathy
Key tests
Liver function tests are not as indicative of the level of hepatic impairment
It is more useful to measure albumin levels and prothrombin time (this provides a better assessment of the synthetic function of the liver)
Management
Correct underlying cause, e.g., if paracetamol, the antidote is N-acetylcysteine
Medical management involves addressing symptoms, e.g., correcting clotting with vitamin K, lactulose for hepatic encephalopathy, terlipressin and albumin
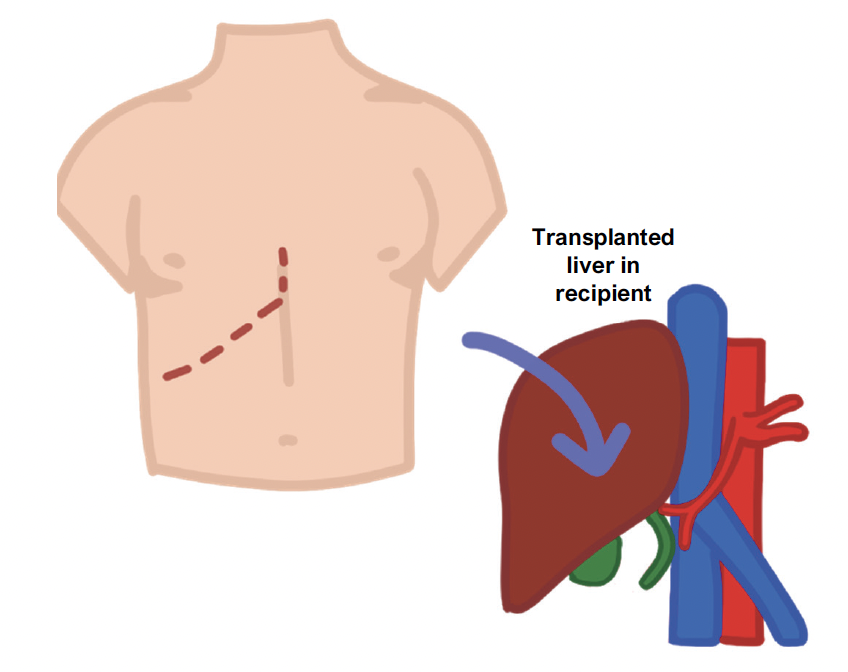
If severe or irreversible damage, liver transplant may need to be considered
Chronic Liver Failure
This is end-stage liver damage characterised by chronic degeneration of the hepatocytes.
Over time, increased inflammation causes fibrosis of the liver and progresses to liver cirrhosis.
Apart from hepatitis B and C, the most common causes of chronic liver disease are alcohol excess and non-alcoholic fatty liver disease.
Key tests
Blood tests – raised LFTs, low albumin, and low levels of clotting factors
Ultrasound liver – this shows a shrunken liver and can reveal increased flow in the portal vein (suggestive of portal hypertension)
Transient elastography uses ultrasound vibrations to measure liver stiffness
The definitive test is a liver biopsy, but this is generally not required
Management
Prevent further liver damage e.g., stop drinking, manage hyperglycaemia
Definitive treatment is liver transplantation
Treat complications accordingly e.g., lactulose for hepatic encephalopathy
Regular OGD to check for varices and ultrasound to check for progression to HCC
Alcohol-related liver disease (ALD)
This is the most common cause of chronic liver failure in which alcohol causes hepatocyte degeneration.
Alcohol initially causes fat accumulation in the hepatocytes, which is reversible.
This then leads to chronic inflammation, as the hepatocytes fill with Mallory bodies.
Alcohol can also cause an acute alcoholic hepatitis on the background of chronic liver damage, which is typically seen after a period of increased alcohol consumption.
Non-alcoholic fatty liver disease (NAFLD)
This is now the most common cause of liver disease in the developed world.
Its aetiology is thought to be associated with increased insulin resistance.
There is a build-up of fat in hepatocytes (steatosis) which leads to inflammation called steatohepatitis. Over time, it slowly progresses to liver cirrhosis.
It is associated with metabolic factors e.g., type 2 diabetes and hyperlipidemia.
A key part of the management involves weight loss and good blood sugar control.
Risk factors
Obesity – defined as BMI over 30. (Stage 1 = 30-35, stage 2 = 35-40, Stage 3 = >40)
Type 2 diabetes mellitus
Hyperlipidaemia
Management
Weight loss
Control diabetes
Complications of Liver Failure
Ascites
This is the collection of fluid in the abdomen due to increased portal pressure.
The causes are split according to the serum: ascites albumin gradient (SAAG)
If > 11 g/L, indicative of liver disease (as it suggests it is due to increased hydrostatic pressure secondary to portal hypertension)
If < 11 g/L, this suggest the cause is not liver related, e.g., malignancy, TB, trauma
Management
Fluid restriction
Diuretics such as spironolactone
Drainage if very large
Spontaneous Bacterial Peritonitis
This is an infection of the ascitic fluid, despite the absence of a clear infection source.
It is thought to occur secondary to E. coli bacterial translocation from the bowel, usually as a complication of ascites secondary to liver cirrhosis.
This leads to a triad of ascites, abdominal pain and fever.
It is diagnosed by an ascitic tap which can be sent for cytology and culture.
If left untreated, patients can become septic and it has a high mortality rate.
Symptoms
Gives a triad of Ascites, abdominal pain and fever
Key tests
Paracentesis (ascitic tap) and check for raised neutrophils
Management
Prophylactic antibiotics (e.g., norfloxacin) are given to patients who have a fluid protein less than 15 g/L or a previous episode of SBP
Treatment involves antibiotics (e.g., cefotaxime)
Hepatic Encephalopathy
The liver is unable to remove ammonia from the blood, due to decreased function.
This allows ammonia to enter the systemic circulation and reach the brain.
Ammonia is neurotoxic and can result in central nervous system dysfunction.
This ranges from mild confusion to asterixis and decreased consciousness.
Symptoms
Gives altered GCS, and asterixis (liver flap) and constructional apraxia (can’t draw a star)
Stage 1 (irritability)
Stage 2 (confusion)
Stage 3 (Incoherent)
Stage 4 (coma)
Management
1st line is lactulose (a laxative which flushes out ammonia producing gut bacteria)
Other options include rifaximin, an antibiotic which kills ammonia producing bacteria

