This refers to chronic, relapsing inflammation of the bowel, which is thought to be associated with an abnormal immune response to gut flora.
It classically presents in the younger population with two key symptoms: bloody diarrhoea and abdominal pain.
It is subdivided into two disorders which share similar symptoms.
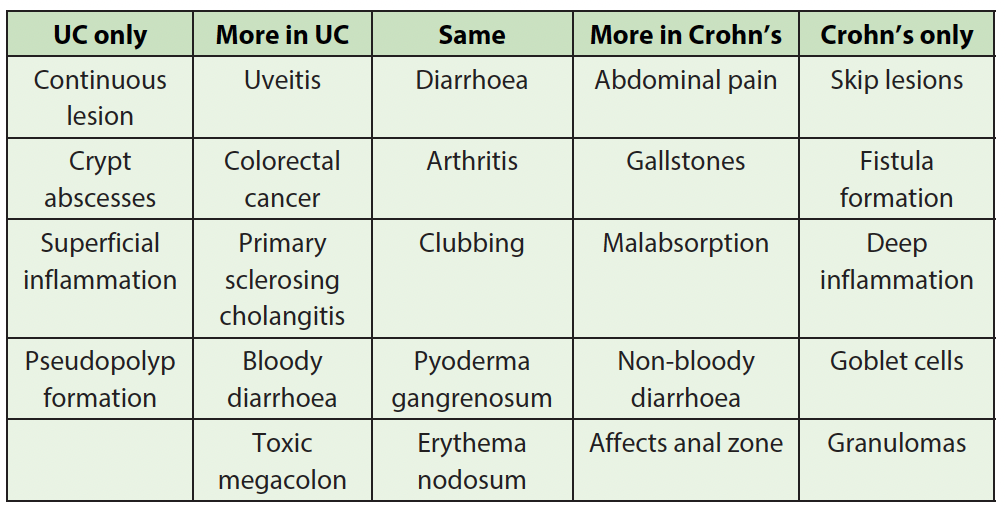
Ulcerative colitis (UC)
This disease is associated with recurrent inflammation of the colon which involves part or all the colon and rectum. The involvement is continuous, rather than in patches and never proximal to the ileocecal valve.
Inflammation leads to bleeding mucosa, pseudopolyp formation and ulcers which extend into the lamina propria.
It can lead to toxic megacolon and colon cancer and is also associated with primary sclerosing cholangitis.
Crohns disease
This is a disease which causes recurrent inflammation anywhere along the GI tract.
It is especially seen in the terminal ileum, resulting in malabsorption of vitamin B12.
It causes inflammation which traverses the whole thickness of wall and is not continuous (skip lesions).
Lymphoid aggregates form, giving granuloma formation with goblet cells.
It is also associated with stricture formation which can lead to bowel obstruction.
It can lead to malabsorption, colon cancer, fistula formation and osteoporosis.
Smoking increases the risk of developing Crohn’s.
Colonoscopy shows a “cobble-stone” appearance of mucosa and rose-thorn ulcers.
General symptoms
Increased bowel frequency
Rectal bleeding (more in UC)
Mucus like rectal discharge
Abdominal pain
Tenesmus (urge to defecate)
Fever, malaise, weight loss
Anal disease (more in Crohn’s)
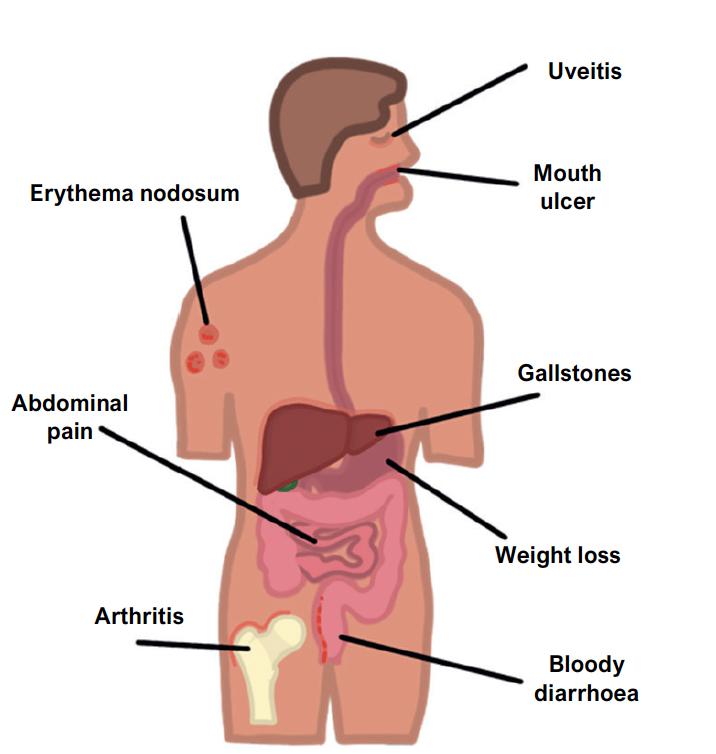
Extra-GI Symptoms
Whilst there are the general symptoms, certain symptoms are more common in Crohn’s disease compared to ulcerative colitis.
Key tests
Blood tests – raised inflammatory markers, e.g., CRP and ESR
Stool test and culture – this is required to exclude an infective cause
Faecal calprotectin – this is a marker for gut inflammation which is raised
There are also a host of imaging techniques which can be used:
Flexible sigmoidoscopy – used in the acute setting to assess lower GI inflammation
Abdominal X-ray – used in the acute setting to check for toxic megacolon
Colonoscopy – a more definitive investigation providing a view of the large bowel
CT scan/MRI small bowel – this is used to assess small bowel inflammation
Capsule endoscopy – in situations when the MRI is not clear, this involves swallowing a camera which takes photos of the gut tube to show intramural inflammation
Acute management
In moderate UC flares, can use topical or oral aminosalicylates before steroids
For Crohn’s and severe UC flares, IV steroids (hydrocortisone) are usually required
This can then be switched to oral steroids on a weaning regimen
If not settling despite steroids, may require biologics, e.g., infliximab rescue therapy
If toxic megacolon, strictures or persistent inflammation, consider surgery
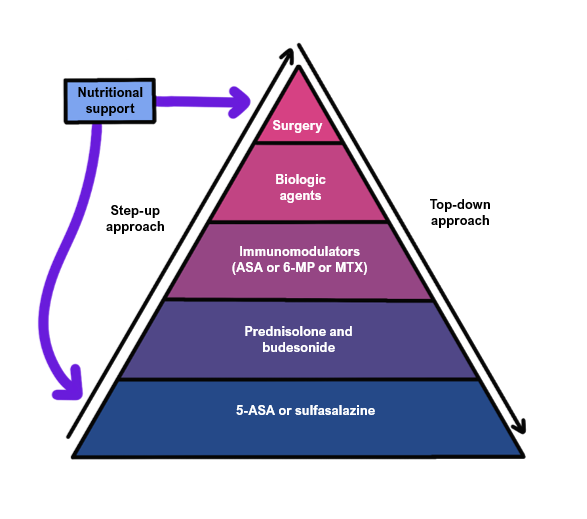
Chronic management
Ulcerative colitis
If mild, topical mesalazine anti-inflammatories
If persistent, increase to immunosuppressive drugs, e.g., azathioprine
If uncontrolled despite immunomodulators, then biological therapy
For recurrent flare, consider surgery, total colectomy is curative
Crohn’s
If mild, first-line is immunosuppressants (e.g., azathioprine, mercaptopurine)
If persistent/severe, consider biological therapy (e.g., infliximab, adalimumab, vedolizumab, ustekinimab)
For repeat flares, may require surgery to resect the inflamed patch of bowel

