Regulation of Osmolality
The body behaves as if its priorities are to maintain ECF osmolality first and then ECF volume.
– Osmolality = the concentration of all solutes in a given weight of water
– Low osmolality means the plasma is more dilute than cells –> this will cause water to move into cells giving “water intoxication” causing brain to swell in the skull.
– The major determinant of ECF osmolality is NaCl. However, changing NaCl does not affect the osmolality since water follows sodium
– Instead ADH adjusts water excretion independently in order to maintain osmolality
The kidney can produce urine that is between 0.1 and 4x the osmolality of plasma.
– It achieves this by pumping ions across cells that are impermeable to water, thus building up an osmotic gradient and using counter-current multiplication
– This occurs in the nephron, which is divided into particular parts which have different permeabilities to water:
i) Proximal Convoluted Tubule:
This is water soluble, so water follows NaCl reabsorption transcellularly and paracellularly.
ii) Descending loop of Henle:
This is water permeable, so water is reabsorbed into interstitium along with NaCl
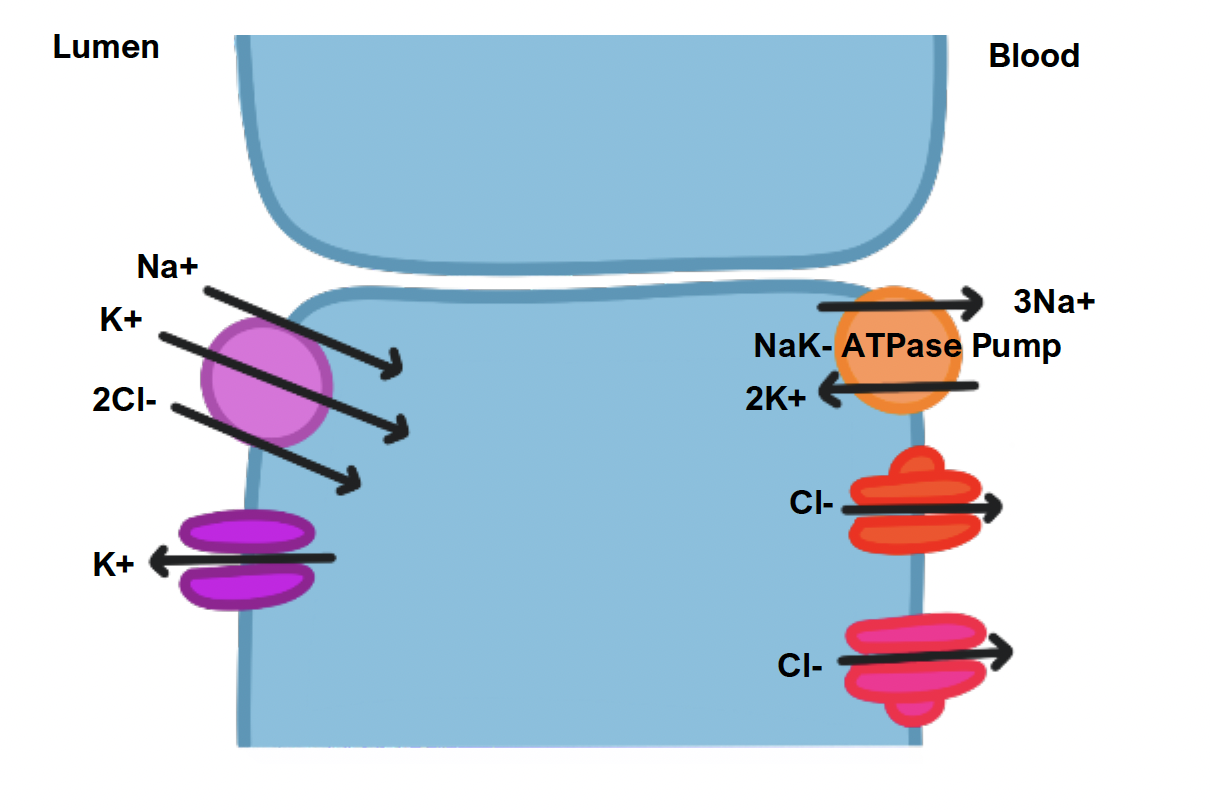
iii) Ascending loop of Henle:
This is the first place in the nephron which separates ions from and water
– Reabsorption of NaCl ions occurs via the NKCC2 transporter.
– However, these cells have low water permeability, so water remains in the tubule making it hypo-osmotic
– Meanwhile the medullary interstitium becomes concentrated.
iv) Collecting duct:
This is usually impermeable to water.
– But it can become more permeable via actions of ADH, allowing water to be reabsorbed by osmosis into the concentrated medullary interstitium.
Urine Production
Due to the specialised structures in the nephron, this allows the kidney to produce both dilute and concentrated urine according to the body’s needs
Making Dilute vs Concentrated Urine
Regulation of Water Volume and Blood Pressure
Unlike osmolality, the extracellular fluid is determined by the Na+ content
– The control is by moving solute not H2O, since movement of NaCl is always isotonic (i.e. water follows NaCl)
A fall in water volume will decrease arterial blood pressure, which is detected by the baroreceptors. This causes a series of changes which attempt to restore blood volume back to normal:
Renal sympathetic nerves:
A reduced blood volume decreases inhibition of sympathetic outflow.
– Stimulates Na+ reabsorption in PCT, by increasing Na+/H+ exchange via NHE3 exchanger.
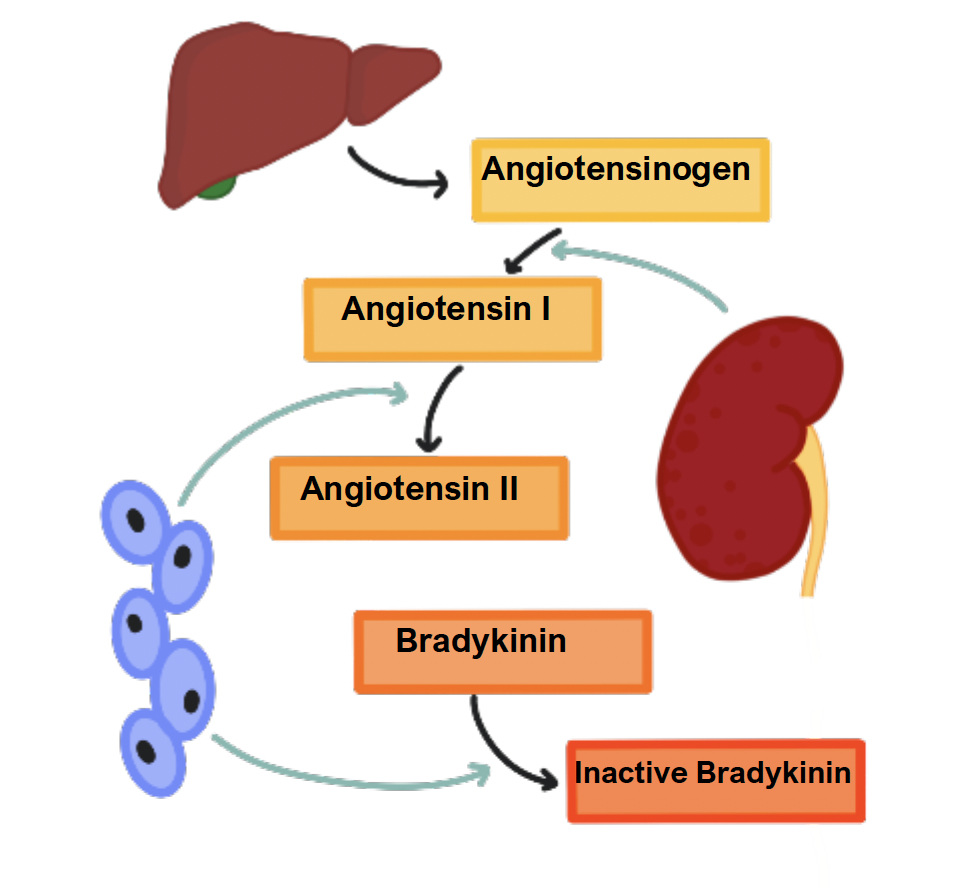
– Stimulates renin secretion, which produces angiotensin II and aldosterone.
Angiotensin II:
This is made from angiotensin I by ACE in the pulmonary capillaries
– Stimulates Na+ reabsorption in PCT, by increasing Na/H+ exchange via NHE3 exchanger.
– Simulates thirst and sodium appetite
– Constricts efferent arteriole to decrease renal blood flow
– Stimulates aldosterone synthesis.
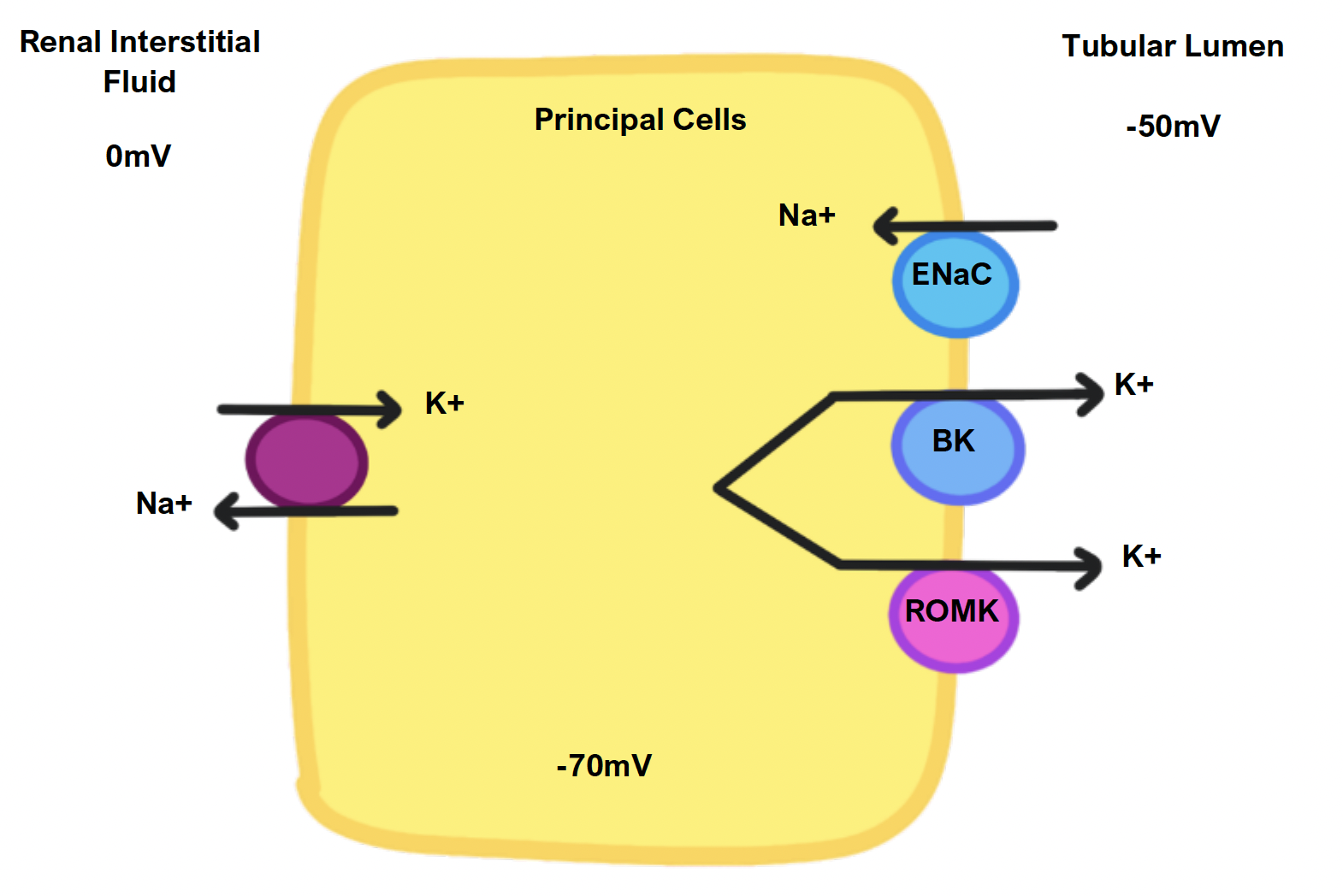
Aldosterone:
This is secreted by the adrenal cortex (outer zona glomerulosa)
– Acts on the principal cells by increasing density of ENaC and SK channels to increase sodium reabsorption into the cells
– Stimulates the H+/K+ ATPase in DCT cells, exchanging H+ secretion for K+.
There are other hormones which have antagonistic actions to angiotensin II and aldosterone:
Atrial natriuretic peptide (ANP):
This is secreted by atrial myocytes in response to increased stretch
– It acts to inhibit ADH secretion, increasing water loss
– Inhibits renin secretion, leading to a fall in Angiotensin II and aldosterone levels
– Reduces expression of ENaC and NHE3 exchanger.
Bradykinin:
This is a small peptide released from various cells which is a natriuretic and vasodilator.
– If the GFR is high, kallikrein is released –> this makes bradykinin which inhibits Na+ reabsorption.
– Broken down by ACE – hence drugs which inhibit ACE cause a bradykinin build up, causing a dry cough.

