Pulmonary Embolus
This is an embolus in the pulmonary circulation, which can impair gas transfer.
The most common source is from a deep vein thrombosis (DVT) in the leg.
Small emboli are usually clinically silent as the lung has a dual blood supply.
Large emboli can give rise to pulmonary infarction causing a myriad of symptoms
Risk factors
Immobility – especially abdominal or hip/knee surgery, bed rest, long haul flights
Thrombophilia – these include blood disorders, e.g., antiphospholipid syndrome, factor V Leiden (the most common inherited thrombophilia) and malignancy
Oestrogen – from the contraceptive pill, hormone replacement therapy, pregnancy
Symptoms
Pleuritic chest pain, shortness of breath and haemoptysis
Tachycardia, tachypnoea, oxygen desaturation
Pleural rub (which disappears when you hold your breath)
Pea-body sign, a clinical sign that involves calf pain upon dorsiflexion of the foot
Key tests
Pulse oximeter may show low SpO2
ABG shows hypoxia, low PaO2 (suggestive of show type I respiratory failure)
CXR – this is usually normal and performed to rule out other pathologies
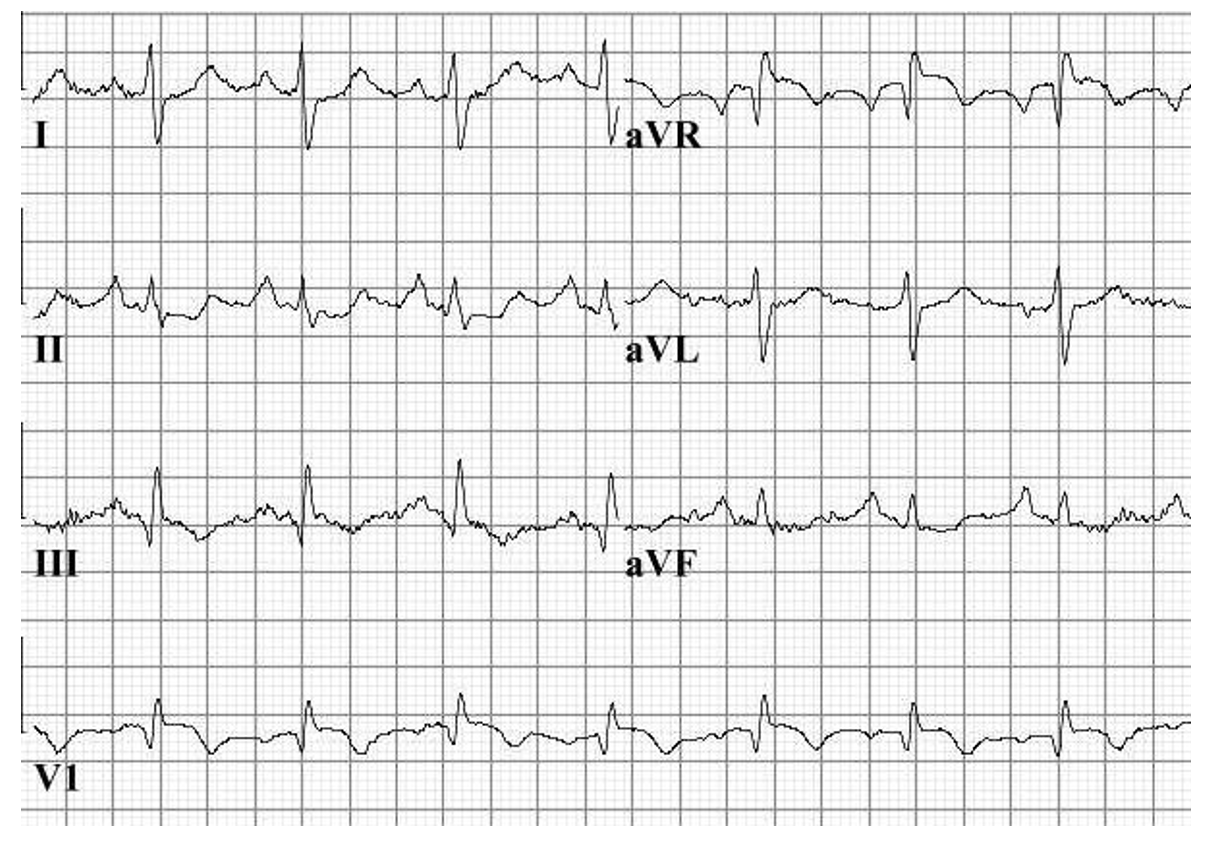
ECG – pathognomonic pattern is S1-Q3-T3. Deep S waves in lead I, pathological Q waves and inverted T waves in lead III
CTPA – this is gold standard and shows vascular filling defect in lung.
V/Q lung scan – shows mismatch between ventilation and perfusion. It is used when CTPA is unsuitable, e.g., due to poor kidney function or in pregnancy/young females
Diagnosis
The diagnostic pathway involves calculating the two-level Well’s score.
If score is 4 or more, it is suggested to go for immediate CTPA
If score is less than 4, request a D-dimer. If this is raised, then get CTPA
If CTPA is delayed, give the treatment dose of anticoagulation until scan is performed
Management
If hemodynamically unstable, patients require thrombolysis (e.g., alteplase)
If haemodynamically stable, therapeutic anticoagulation for 3–6 months
Pulmonary hypertension
This is a condition which is caused by a resting mean pulmonary artery pressure >25mmHg.
The main problem is that raised pulmonary pressure caused increased stress on the right side of the heart and can lead to right sided heart failure, a complication known as cor pulmonale
Primary hypertension occurs due to atherosclerosis of pulmonary trunk, smooth muscle hypertrophy and fibrosis, leading to the development of plexiform lesions.
Endothelin-1 is a potent pulmonary vasoconstrictor produced in increased amounts in pulmonary hypertension. It also induces the proliferation of pulmonary vascular smooth muscle.
Causes
Primary
This is typically seen in young adult females, aged 30-50 years
Due to an idiopathic cause, but there are some autosomal dominant forms due to inactivation mutations of BMPR2 leading to increased proliferation of vascular smooth muscle
Secondary
Due to hypoxemia (e.g. COPD)/ increased circulating volume (heart disease) or PE
Symptoms
Leads to progressive exertional shortness of breath
Chest pain
Syncope
Eventual Cor pulmonale – cardiac complication of pulmonary hypertension that involves right ventricular failure and hence gives jugular venous distension, oedema and hepatomegaly
Management
Acute vasodilator testing is used to decide on the appropriate management strategy:
If positive response to vasodilator testing, Give oral Ca2+ channel blockers
If negative response options include PDE 5 inhibitor (Sildenafil), endothelin antagonist (Bosentan) or prostacyclin analogues (Iloprost)

