Varicose Veins
This is a condition where the superficial veins become tortuous and enlarged.
Usually occurs due to valve insufficiency of the leg vein valves, resulting in venous hypertension and dilation
Risk factors
Obesity
Family history
Pregnancy
Oral contraceptive pill
Symptoms
Most are asymptomatic and only give cosmetic deformity (e.g., twisted superficial dilated veins)
Can occur with aching heavy legs with cramps and itching.
However, can lead to oedema and eventual ulcer formation with associated symptoms
Management
Only should be referred if pain, ulceration or a severe impact on quality of life (not cosmetic)
Non-surgical management – avoid prolonged standing, lose weight, compression stocking
Surgical management includes radiofrequency ablation: catheter inserted into vein heated to 120ºC burns endothelium closing vein and endovenous laser ablation: a similar method but uses a laser instead
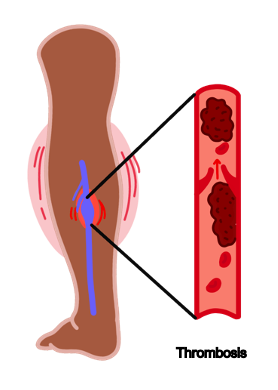
Deep Vein Thrombosis (DVT)
This is a clot which occurs usually in the femoral, popliteal or iliac veins in the leg.
It occurs due to blood stasis which brings pro-coagulants in contact with each other.
It is the most common cause of pulmonary embolism.
Symptoms
Tender calves, usually after period of immobilisation
Heavy legs and erythema
Leg swelling and oedema
Diagnosis
Calculate two-level DVT Wells score, which awards points for risk factors
These include active cancer, previous DVT, entire leg swollen, localised tenderness over calf, paralysis or immobilisation of legs (+ other factors)
If 2 points or more, do a proximal leg vein ultrasound scan within 4 hours
If < 2 points, advised to do a D-dimer test.
If this is raised, perform a proximal leg vein ultrasound within 4 hours
If the scan cannot be done within 4 hours, give the therapeutic anticoagulation dose, whilst awaiting the ultrasound scan to confirm the diagnosis
Management
If DVT confirmed, anticoagulation is given, usually with DOAC (e.g., apixaban)
If poor renal function/contraindications, then LMWH/warfarin can be given
Anticoagulation is continued for at least 3 months if provoked (e.g., surgery, immobilisation) or up to 6 months for an unprovoked DVT
Two of the most important risk factors for DVT are malignancy and thrombophilia.
In patients with unprovoked DVT, you should investigate for underlying causes.
Take a detailed history for weight loss/red flag symptoms and consider further investigations to look for underlying cancer/thrombophilia.
Post-Thrombotic Syndrome
Peripheral Arterial Disease (PAD)
This condition refers to reduced blood flow to the peripheral limbs, usually the legs.
It represents a spectrum of symptoms from asymptomatic to critical.
It usually occurs over time due to atherosclerosis leading to increasing ischaemia.
However, occasionally there is an acute obstruction either from limb ischaemia or distal embolisation of a clot formed more proximally, for example in atrial fibrillation.
Risk factors
Smoking
Diabetes
Hypertension
Hyperlipidaemia
Atrial fibrillation
Symptoms
Intermittent claudication (aching or burning in the leg muscles following walking)
Pain in the legs, often worse at night when the patient’s legs are elevated
If severe, leads to ulceration and gangrene formation
If critical, 6Ps (pallor, pulseless, painful, paralysis, paraesthesia, perishingly cold)
Key tests
Ankle brachial pressure index (ABPI) compares the blood pressure in the ankle against the arm. In PAD, the BP is reduced in the lower limb due to atherosclerosis.
However, it is possible to get a false positive. Conditions like diabetes lead to calcification of the arteries of the lower limb, which will increase the blood pressure.
Lower limb doppler ultrasound (shows flow within leg arteries)
CT/MR angiography is used to visualise the extent of blockage in the arteries
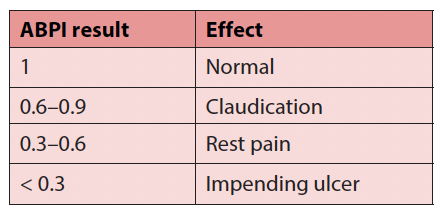
Problems with ABPI
Management
Conservative – supervised exercise programme and smoking cessation
Medical – statin (e.g., atorvastatin 80 mg), antiplatelet therapy, diabetic control
Surgical approaches include stenting or bypass surgery
In critical limb ischaemia, amputation may be required

