Angina
This is the term which is used to describe symptomatic chest pain which occurs due to myocardial ischaemia.
In the heart, the coronary circulation fills during diastole. Due to atherosclerosis, over time, the coronary arteries become occluded impeding blood flow to the muscle.
It means areas of myocardium become ischaemic, especially in times of greater oxygen demand, which leads to chest pain.
To counteract this, the body increases sympathetic stimulation which aims to increase cardiac output. But this worsens the issue as it increases O2 demand further.
Hence, when treating angina, the main goals are increasing coronary filling by vasodilation, increasing diastolic time and reducing myocardial oxygen demand.
There are 2 main types of angina
Stable angina
This is a chronic condition which occurs when > 70% of the vessel is occluded.
It has three main defining criteria.
Typical angina has all 3 features, whereas atypical angina has two of these features.
1) Constricting discomfort in the front of the chest/neck/shoulders/arms
2) Pain which is precipitated/exacerbated by physical exertion
3) Relieved by rest or GTN spray (within 5 minutes)
Unstable angina
This is chest pain that occurs at rest and generally requires inpatient treatment. It is managed as acute coronary syndrome until the troponin comes back as negative.
It can be due to rupture of a plaque which leads to incomplete occlusion of coronary artery, or just critical coronary artery stenosis.
It is relieved by GTN and associated with ST-segment depression.
However, there is high risk of progression to myocardial infarction (treated as ACS).
Key tests
For stable angina, 1st line is CT coronary angiography (CTCA)
2nd line is non-invasive functional imaging to look for reversible myocardial ischaemia
In unstable angina, generally invasive angiography is performed, although performing a CTCA is reasonable
Management
The management for stable angina involves three types of medication:
1) Prognostic medications to reduce risk of MI – aspirin and a statin
2) Initial symptom relief – glyceryl trinitrate spray
3) Longer term – 1st line is B-blocker or Ca2+ channel blocker (verapamil or diltiazem)
If still symptomatic, give dual therapy with beta-blocker and dihydropyridine
If dual therapy not tolerated, add nicorandil or ivabradine or long-acting nitrate
Prinzmetal Angina
Myocardial Infarction
This is a term that describes the irreversible death of cardiac myocytes, which occurs due to ischaemia.
It is due to the rupture of a plaque which leads thrombosis and arterial occlusion.
It can be divided into an ST-elevated myocardial infarction (STEMI) and non-ST elevated (NSTEMI).
Risk factors include age, hypertension, diabetes, sex (male) and smoking.
Symptoms
Acute crushing chest pain that comes on at rest (elderly/diabetics may have no pain)
Pain radiating to the jaw, neck and either or both upper limbs
Sweaty and clammy
Nausea, vomiting and epigastric pain
Key tests
Blood Troponin
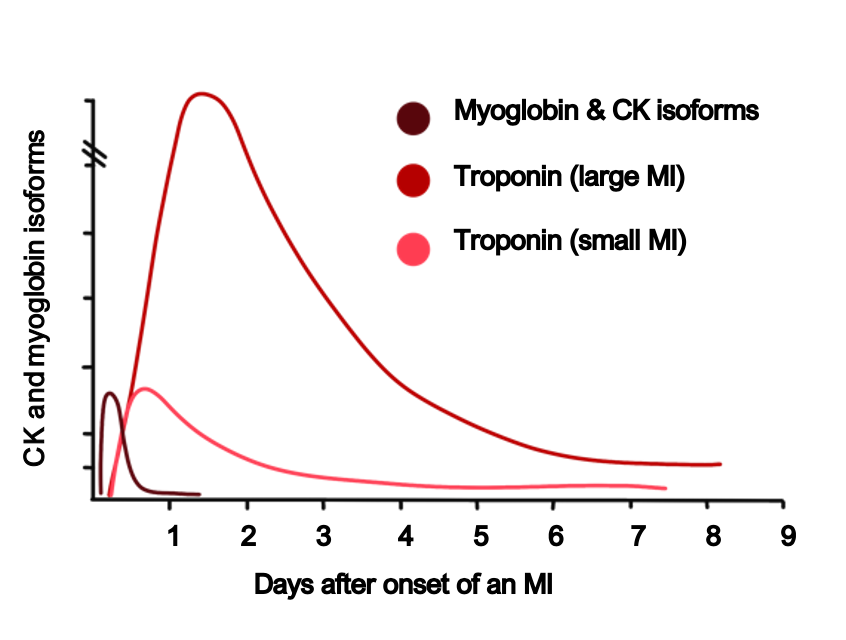
Levels of troponin I indicate damage to myocardial cells.
Two samples taken 3h apart and indicate possible infarction.
Levels rise 2-4 hours and peak at 24 hours
ECG
This is helping in identifying ischaemic changes
STEMI = >1mm ST elevation in at least 2 consecutive limb leads
Or >2mm ST elevation in at least 2 consecutive precordial leads
Or new onset left-bundle branch block.
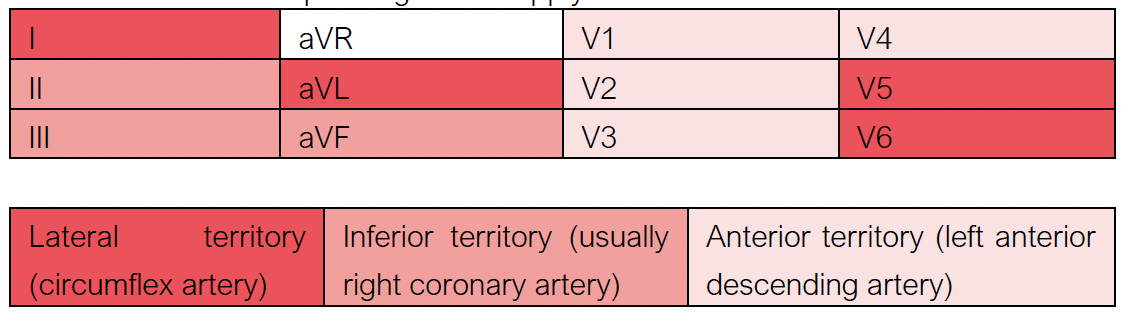
By seeing which leads the ST elevation occurs in, we can determine which artery has been occluded:
Lead V1-V4 = anterior territory –> LAD artery
Leads I, V5, V6 = lateral territory –> Circumflex artery
Leads II, III, aVF = inferior territory –> Right coronary artery
ECG areas and corresponding blood supply:
Acute Management
If patient has raised troponin, then there are some common steps regardless of whether it is a STEMI or NSTEMI:
Morphine – given for pain relief (with an anti-emetic, e.g., metoclopramide)
Oxygen – given if SpO2 is below 94%
Nitrates – GTN spray given to vasodilate veins and reduce preload on the heart
Aspirin – loading dose of 300 mg
P2Y12 inhibitor – ticagrelor, clopidogrel or prasugrel
There are then some specific pathways according to whether it is a STEMI or an NSTEMI
STEMI
Dual antiplatelet therapy (aspirin and ticagrelor, but some trusts give clopidogrel)
1st line is primary percutaneous coronary intervention (PCI) within 12 hours of symptom onset
Fibrinolysis is given if PCI cannot be given within 120 minutes of the time when fibrinolysis could be given. After fibrinolysis, do ECG 90 minutes later to see if there is > 50% resolution in ST elevation
If very severe, may require open heart surgery or emergency coronary bypass
NSTEMI
Treatment is with dual anti-platelets and fondaparinux (unless immediate angiography required).
The timing of angiography depends on clinical symptoms
In high-risk patients (haemodynamic instability, cardiogenic shock, widespread ST depression) it should be performed within 2 hours
If lower risk, angiography is performed later. This latter decision can incorporate the GRACE score to decide – if > 140 should be within 24 hours.
Chronic Management
Patients are given cardio-protective medications to reduce risk in future:
Aspirin
Second antiplatelet – clopidogrel, prasugrel or ticagrelor
B-blocker – slows heart rate and decreases risk of arrhythmia
ACE inhibitor – decreases left ventricular dilation reducing preload
Statin

