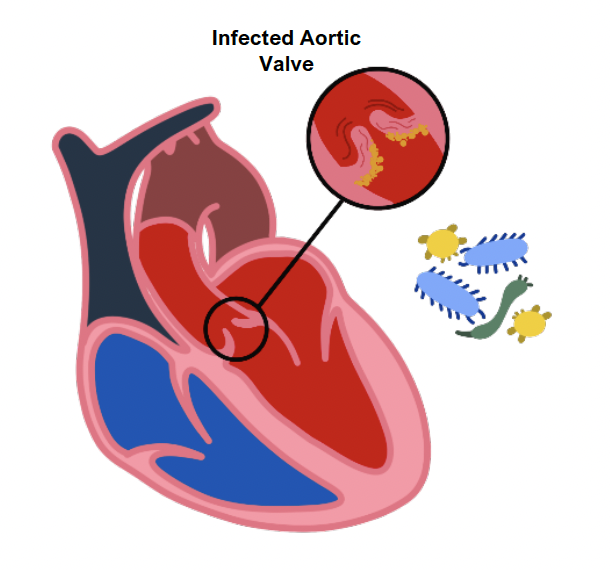
This refers to inflammation of the endocardium that lines the surface of heart valves.
It can lead to vegetations on the valve surface that can destroy the valve.
In addition, it can lead to septic emboli formation leading to other complications.
Causes
Staphylococcus aureus
This is the most common cause of IE which is usually seen in IV drug abusers
It is a high virulence organism that destroys valves, most commonly the tricuspid valve
Risk factors for this bacterium include skin breaches (dermatitis, IV lines), kidney failure and diabetes
Viridans Streptococci
This is a group of low-virulence bacteria that affects previously damaged valves.
It is associated with poor dentition with sequelae of dental procedures
It causes small vegetations that do not completely destroy the valve and so causes a subacute endocarditis
The damaged endocardium develops small thrombotic vegetations of platelets and bacteria
Staphylococcus epidermidis
This is associated with endocarditis of prosthetic valves
Streptococcus bovis
This is associated with endocarditis in patients with colorectal carcinoma
HACEK organisms
These are Gram negative bacteria which give negative blood cultures
HACEK Organisms
Fungi
Candida and Aspergillus, seen in IV drug users and immunocompromised patients
Non – bacterial thrombotic endocarditis
This is due to sterile vegetations that arise in association with a hypercoagulable state or an underlying adenocarcinoma
Vegetations usually occur on the mitral valve and lead to mitral regurgitation
Libman-Sacks endocarditis
This is when you get vegetations associated with SLE.
Vegetations occur on both sides of the mitral valve and lead to mitral regurgitation.
Symptoms
Septic symptoms – fever, anaemia, clubbing, weight loss
Cardiac symptoms – heart murmur (due to valve disease), heart failure, chest pain
Immune complex deposition – Roth spots (retinal haemorrhage with pale centers), splinter haemorrhages and Osler nodes (tender lesions on fingers and toes)
Septic emboli – these can cause abscesses in organs, e.g., in skin they are called Janeway lesions (on palms), ischaemic strokes
Diagnosis
The is done using the modified Duke criteria, which use major and minor criteria:
Major Criteria
2 Positive blood cultures – 3 cultures are taken from different sites when the patient is febrile, looking for typical microorganisms which cause infective endocarditis
Involvement of the endocardium, which is shown by an echocardiogram. A transthoracic echocardiogram cannot rule out IE – perform TOE if high suspicion
Minor Criteria
Predisposition (e.g., valve prolapse)
IV drug use
Fever > 38 degrees celcius
Microbiologic evidence (e.g., blood cultures not meeting major criterion)
Immunologic phenomena, e.g., Osler nodes/Roth spots
Vascular signs e.g., splinter haemorrhages, Janeway lesions
Management
Antibiotic therapy according to cultures and sensitivity
Initial empirical therapy may involve amoxicillin and low dose gentamicin
Some severe cases may require valve replacement surgery, e.g., if there is acute heart failure, severe valve incompetence or recurrent embolic events

