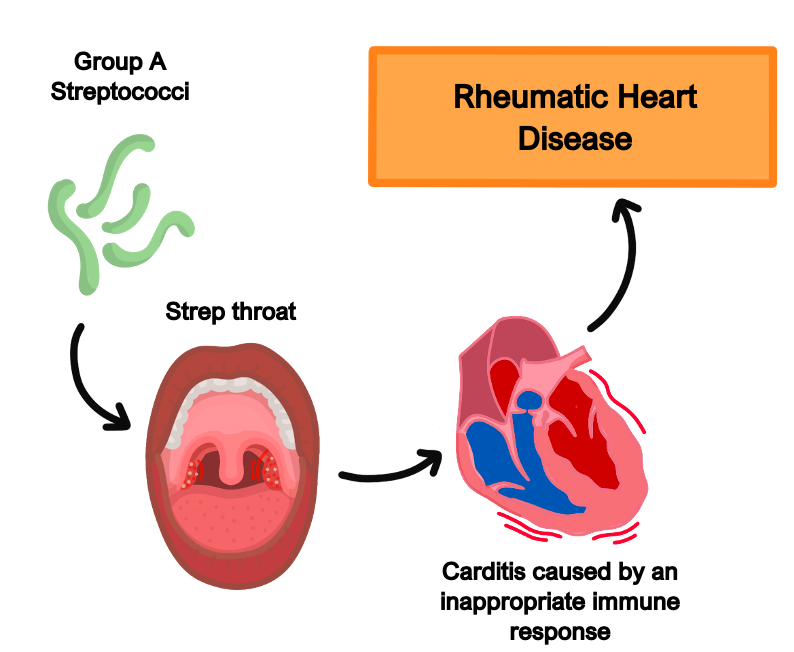
Rheumatic fever
This is a complication after being infected with group A β-haemolytic streptococcus.
Antibodies directed against the streptococcus pyogenes M-antigen cross react with myosin and smooth muscle.
This leads to a systemic condition which occurs in acute attacks, taking about three months to recover. It can also cause chronic inflammation leading to permanent damage to heart valves.
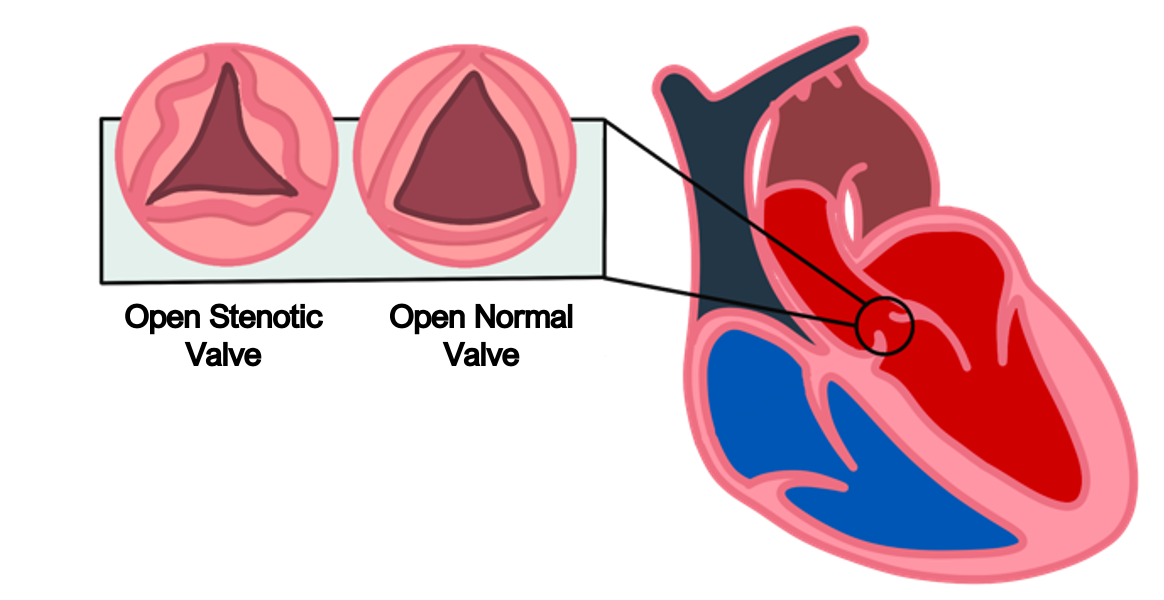
It typically causes stenosis of valves (usually mitral) with a “fish mouth” appearance.
Symptoms
History of previous streptococcal infection (e.g., pharyngitis)
Infective signs – fever and arthralgia
Cardiac symptoms (e.g., mitral stenosis) may occur after multiple attacks of RF
Key tests
Jones criteria is used, which requires evidence of recent infection plus 2 major, or 1 major and 2 minor criteria to be filled.
Evidence of prior group A B-haemolytic streptococcal infection
By throat culture or anti-streptolysin O (ASO) antibodies/anti-DNase B titres
Major criteria
Cardiac inflammation, including endocarditis (small vegetations along mitral valve) and myocarditis (Aschoff bodies, characterised by foci of chronic inflammation)
Migratory polyarthritis – joint inflammation that resolves and migrates to a new joint
Subcutaneous nodules on joints and spine
Erythema marginatum – a non-pruritic rash with red borders on trunk and limbs
Sydenham chorea – jerky, uncontrollable and purposeless muscle movements
Minor criteria
Fever
Prolonged PR interval on ECG
Raised inflammatory markers (ESR/CRP)
Management
Penicillin based antibiotics and anti-inflammatories
Important to treat the complications (e.g., mitral valve stenosis) as they occur
Individual Valve Conditions
These conditions affect specific valves and are usually divided into stenotis (narrowed) or regurgitation (incompetency of the valve) leading to backflow of blood.
Key tests
The key diagnostic for identifying valvular conditions is an echocardiogram
Management
The definitive management for valve conditions is a valve replacement.
If less severe or surgery not suitable, medical management is considered.
Tricuspid regurgitation
This refers to incompetency of the tricuspid valve which connects the right atrium and ventricle, which allows blood to flow back from the right ventricle to the right atrium.
This raises right atrial pressure and reduces venous return.
Therefore, it produces similar symptoms to right sided heart failure.
Causes
Right ventricle hypertrophy (after pulmonary hypertension) or right ventricle MI
Classically seen in infective endocarditis of IV drug users
Rheumatic fever, Ebstein’s anomaly, carcinoid syndrome
Symptoms
Gives signs of right heart failure (peripheral oedema, active pulsing in JVP)
Pulsatile hepatomegaly with left parasternal heave
Gives a pansystolic murmur head over the left sternal edge
Mitral Regurgitation
This refers incompetency of the mitral valve which allows blood from the left ventricle to enter the left atrium during systole.
Causes
Mitral valve prolapse
Myocardial infarction, causing ischaemia of the papillary muscles
Infections – rheumatic fever and infective endocarditis
Arrhythmias – long-standing fast AF can cause progressive atrial dilatation and reduce coaptation of the mitral valve

Symptoms
Most patients are asymptomatic until the MR becomes very severe
Can give signs of left-sided heart failure (dyspnoea, fatigue, oedema)
Pansystolic “blowing” murmur at the apex radiating to the axilla with a soft S1
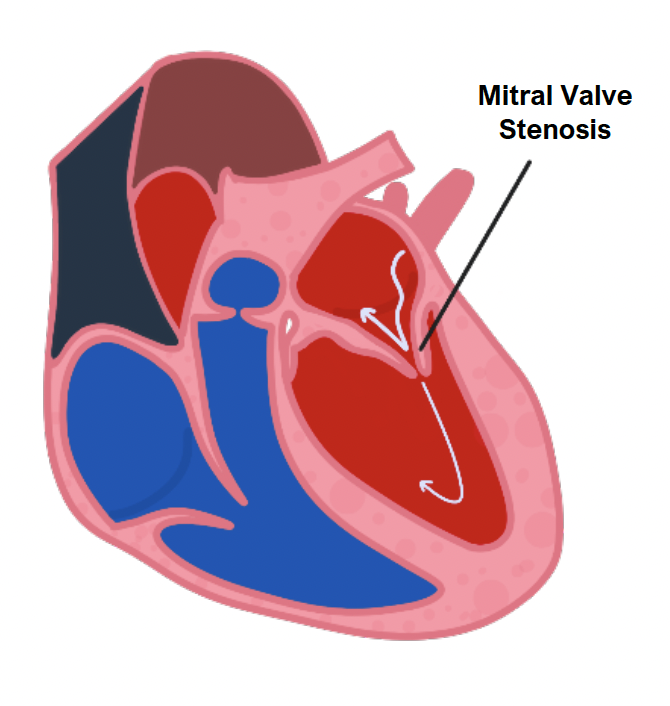
Mitral Stenosis
This is narrowing of the mitral valve orifice, usually due to chronic rheumatic fever.
This reduces blood flow from the left atrium into the ventricle and will cause enlargement of the left atrium.
This reduces the cardiac output from the left ventricle and so produces symptoms of left-sided heart failure.
Symptoms
Heart failure – dyspnoea, chest pain
Malar flush on cheeks due to decreased cardiac output
Fatigue, worse with activity
Atrial fibrillation and palpitations
Can lead to secondary pulmonary hypertension and right sided heart failure
Gives an opening snap followed by a mid-late diastolic murmur
Mitral Valve Prolapse
This refers to ballooning of the mitral valve into the left atrium during systole.
It is a type of myxomatous valve disease, which means the tissue of the mitral valve leaflets and chordae are abnormally stretchy, making the valve “floppy”.
Whilst it is mostly asymptomatic, it predisposes to complications such as valve regurgitation, arrythmias, emboli and infective endocarditis.
Causes
Connective tissue disorders (Marfan, Ehlers-Danlos syndrome)
Genetic conditions, e.g., polycystic kidney disease, Turner’s syndrome
Symptoms
Usually asymptomatic, but patients can get atypical chest pain or palpitations
Produces a mid-systolic click and late systolic murmur
Aortic stenosis
This is the narrowing of the aortic valve orifice, usually due to fibrosis and calcification from “wear and tear”.
It usually presents in late adulthood (> 60 years) and means that less blood is able to flow out from the ventricle into the aorta, which reduces cardiac output.
It is associated with a triad of chest pain, exertional dyspnoea and syncope.
Causes
Calcification of the valve due to age
Bicuspid aortic valve (seen more in younger patients)
Rheumatic fever, William’s syndrome
Symptoms
Can be asymptomatic until the narrowing gets severe
Gives chest pain, breathlessness and syncope with exercise
Narrow pulse pressure with slowly rising pulse
Leads to eventual left ventricular hypertrophy or failure
Systolic ejection murmur radiating to carotids and a soft S2
May hear additional 4th heart sound
Management
If symptomatic, will require valve replacement
If asymptomatic, measure valvular gradient – if > 40 mmHg (severe) with ventricular dysfunction may need surgery
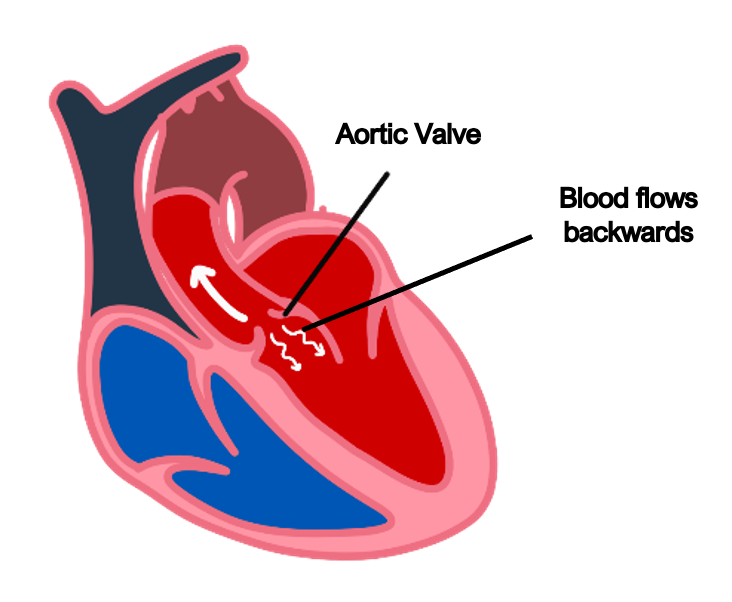
Aortic Regurgitation
This condition refers to aortic valve incompetency, which results in the backflow of blood from the aorta into the left ventricle during diastole.
This means that the left ventricle must compensate by pumping the blood harder to maintain a sufficient cardiac output.
This leads to left ventricular hypertrophy over time.
Left untreated, this will eventually lead to heart failure.
Causes
These are divided into valvular causes and aortic root causes
Valvular – rheumatic fever, IE, connective tissue disease, bicuspid aortic valve
Aortic root disease – aortic dissection, hypertension
Symptoms
Heart failure symptoms – breathlessness, orthopnoea, palpitations
A hyperdynamic circulation with wide pulse pressure (difference between systolic and diastolic). The diastolic is lower due to regurgitation, whilst systolic higher due to increased stroke volume.
Gives a water-hammer/collapsing pulse
Left ventricular dilation and eccentric hypertrophy
Early, blowing diastolic murmur heard in the tricuspid region
Rarer signs include pulsating nail bed (Quincke pulse) and head bobbing with each heartbeat (de Musset’s sign)
Management
Main goal is to reduce systolic hypertension with medication
Valve replacement if there is heart failure and dysfunction of the left ventricle

