This is a clinical syndrome consisting of symptoms (e.g., breathlessness, oedema, fatigue) that occurs due to abnormalities in cardiac structure or function, causing inadequate cardiac output or raised intracardiac pressures.
Usually, it is due to myocardial dysfunction, but can be due to other causes like valvular disease, pericardial disease or arrhythmias.
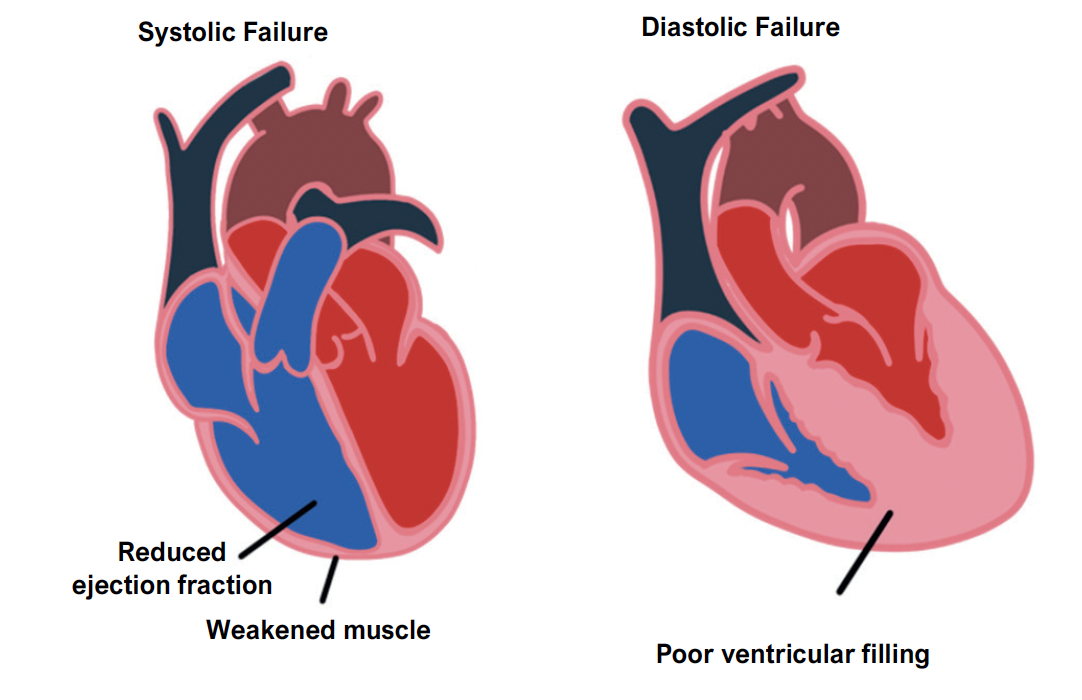
Systolic failure
This is an inability for the ventricle to contract properly, decreasing cardiac output.
In this case, the ejection fraction (EF) is < 40%.
It occurs due to conditions which weaken the heart muscle reducing contractility, e.g., ischaemic cardiomyopathy, dilated cardiomyopathy and myocarditis.
Diastolic failure
Refers to an inability of the ventricles to fill normally causing increased filling pressure.
The ejection fraction here is usually > 50%, but because the ventricles cannot fill, the cardiac output is low and filling pressures are raised.
Causes include disorders of heart muscle such as hypertrophy, extrinsic compression from pericardial disease and tamponade from pericardial fluid.
Traditionally, heart failure has been divided into left and right sided heart failure depending on the main ventricle affected.
These can occur separately, but if both are present it is known as congestive cardiac failure (CCF).
Right ventricular failure
This usually occurs after left-sided failure and pulmonary hypertension
It is also due to left–>right shunts, which increases the pulmonary blood flow.
This results in results in congestion of the peripheral venous circulation
Symptoms
Raised JVP, pitting ankle oedema and ascites
Hepatosplenomegaly with a smooth “nutmeg” liver which is pulsatile
Left Ventricular failure
This is usually due to MI, cardiomyopathies and ischemia
– Results in decreased forward perfusion and congestion of the pulmonary circulation
Symptoms
– Dyspnoea, paroxysmal nocturnal dyspnoea, orthopnoea (breathlessness lying down)
– Polyphonic expiratory wheeze with bibasal crackles due to pulmonary oedema
– Gives a 3rd heart sound
– Weight loss (however, the patient will also have weight gain due to the oedema)
– Pulsus alternans (alternation of force of arterial pulse: hard then soft)
Grading
Heart failure is graded using the New York classification of heart failure:
Grade 1 – asymptomatic with no dyspnoea from ordinary activity
Grade 2 – mild symptoms present, dyspnoea from ordinary activities but comfortable at rest
Grade 3 – moderate symptoms present, dyspnoea from less than ordinary activity but comfortable at rest
Grade 4 – Severe symptoms present with dyspnoea at rest
Key tests
Blood tests show raised natriuretic peptides (BNP and NT-proBNP). These are secreted when heart chambers become overloaded
Echocardiogram – used to assess the ventricular ejection fraction
ECG – this shows signs such as axis deviation and may show ischaemia
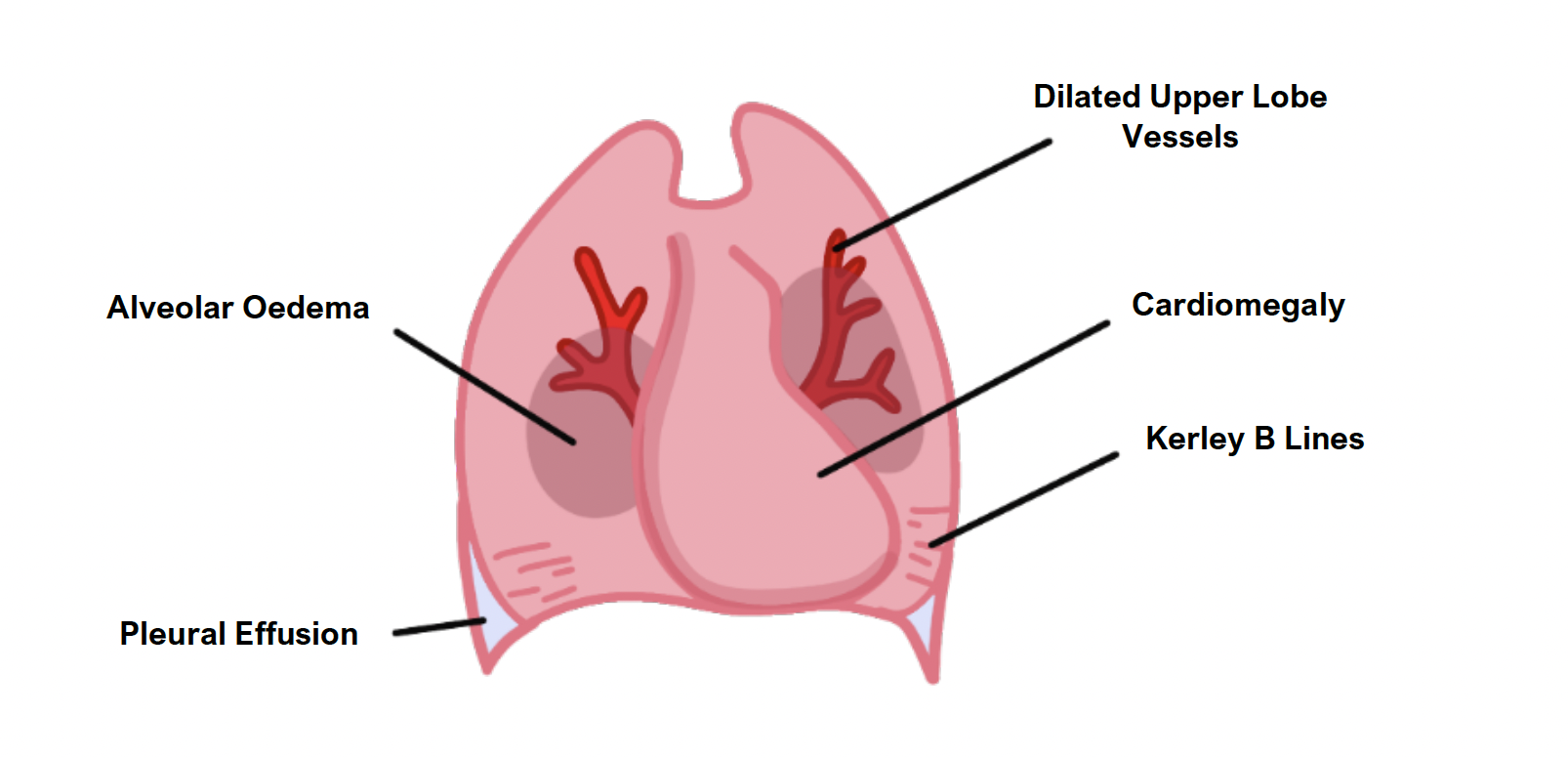
Chest X-ray – left ventricular failure shows signs of fluid overload such as pulmonary oedema, pleural effusions, Kerley B lines
Acute management
The aim is to drive the fluid out of the lungs reducing breathlessness
This is achieved through diuretics and then nitrates to reduce pre/afterload
Give oxygen to keep saturations > 94%
IV furosemide
If BNP is still raised, start IV nitrates
CPAP can be used to drive out fluid from lungs
You should avoid beta-blockers in acute heart failure as they are negatively ionotropic and can severely reduce (already-struggling) cardiac output
Chronic management
The aim of treatment is to oppose the body’s natural compensatory mechanisms which try to increase cardiac output, as this just makes the situation worse.
Patients with heart failure should also be offered the annual Influenza vaccine and a single pneumococcal vaccine.
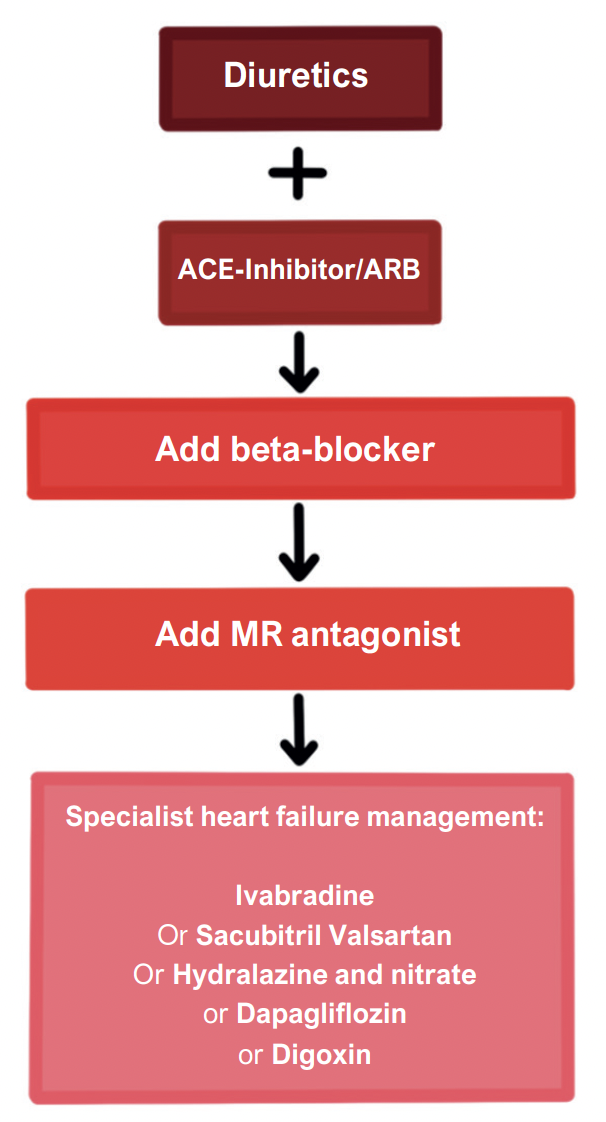
Diuretic e.g., furosemide
Used for symptomatic (fluid overload) relief but has no proven mortality benefit.
ACE inhibitor e.g., ramipril
1st line treatment which is given to patients with EF < 40%.
Beta-blocker e.g., bisoprolol
This is given in addition to ACE-i in patients with EF < 40% or those with LV systolic dysfunction after myocardial infarction.
Mineralocorticoid receptor antagonist e.g., spironolactone
This is recommended as a 3rd drug added on for patients persisting with symptoms or when LVEF < 35%.
Angiotensin receptor blocker (ARB) e.g., candesartan
This can be used when the ACE-i is not tolerated (due to dry cough) or as the 3rd drug when the MRA not tolerated with ACE-i and the B-blocker.

