Hypertension (HTN)
This refers to raised arterial blood pressure, usually defined as BP > 140/90 mmHg.
It is usually asymptomatic but can produce symptoms if the blood pressure becomes very high. Hypertension can be categorised according to the cause:
Primary
This is the most common type which occurs due to an unknown aetiology.
It is a chronic condition which often develop around middle age and is known as essential hypertension.
Risk factors include male sex, age, race, obesity, salt diet.
Secondary
This is HTN which occurs secondary to an identifiable aetiology.
It is important to remember that these causes are usually much rarer (5% of cases).
Key indicators include young age, BP > 180 mmHg unresponsive to medication and electrolyte imbalance.
Secondary Hypertension Causes
Diagnosis
If raised one off blood pressure > 140/90 mmHg, advised to do ambulatory or home blood pressure monitoring
Ambulatory blood pressure monitoring (ABPM) involves taking 2 BP measurements per hour during the day and gives an average value of 14 measurements
Home blood pressure monitoring (HBPM) involves recording BP twice daily, in the morning and evening for ideally 7 days and taking the average value
Staging
You can use the clinic and ABPM/HBPM to stage the hypertension

Management
If Stage 1, treat only if age < 80 years AND the patient has evidence of organ damage, diabetes or QRISK > 10%
If Stage 2, all patients should be started on antihypertensive medication
If Stage 3, urgent fundoscopy to check for papilledema/retinal haemorrhages and specialist referral

Hypertension managament depends both on age and ethnicity.
Step 1
If < 55 or diabetic, start with ACE-inhibitor (or ARB)
If > 55 or Afro-Caribbean, start with Ca2+ blocker
Step 2
If BP is still high, commence dual therapy.
If on ACE-i, add Ca2+ blocker or thiazide-like diuretic.
If on Ca2+ blocker, add ACE-i or thiazide-like diuretic
Step 3
If BP uncontrolled, triple therapy with ACE-i, Ca2+ blocker and thiazide-like diuretic
Step 4
If K < 4.5 mM, add MRA (e.g., spironolactone); if K > 4.5 mM, add alpha-blockers (e.g., doxazosin) or beta-blockers
If blood pressure is still not controlled, they require specialist advice as they will need additional medication or investigation.
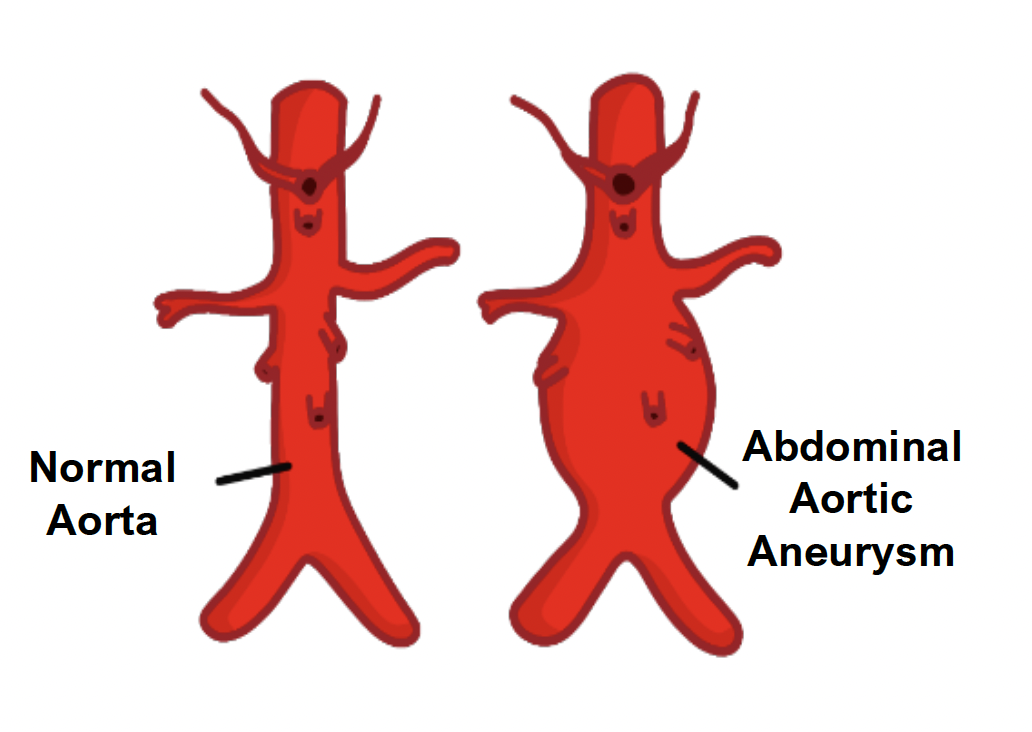
Aortic Aneurysms
An aortic aneurysm occurs when the aorta is dilated to > 50% of its original diameter.
A true aneurysm is an abnormal dilation of the vessel which involves all 3 layers of the arterial wall.
A false aneurysm involves blood collecting in the tunica adventitia which communicates with the lumen.
Causes
Cardiovascular risk factors – hypertension, smoking, diabetes, hyperlipidaemia
Connective tissue disorders – Ehlers Danlos syndrome, Marfan syndrome
Infections – tertiary syphilis (leads to arterial wall atrophy)
Abdominal Aortic Aneurysm
This is a dilation of the abdominal aorta > 3 cm.
It is usually asymptomatic even when the diameter increases to > 5.5 cm.
Symptoms
Central abdominal pain radiating to back, renal colicky pain and irritation of leg nerves
When ruptured, usually causes hypotension and bleeding in the flanks (this will most likely be fatal)
Management
There is a screening program which involves abdominal ultrasound at age 65
If asymptomatic or aortic diameter < 5.5 cm, monitor with ultrasound every 3 months
If symptomatic, diameter > 5.5 cm or expanding > 1 cm/year, endovascular repair or open surgery will likely be required
Thoracic Aortic Aneurysm
This occurs when the thoracic aorta is dilated to > 50% of its original diameter.
Symptoms
Acute chest pain which radiates to the back between the shoulder blades
Can cause dilation of the aortic valve root, causing aortic valve regurgitation
Management
Surgery or stenting (endovascular aneurysm repair, EVAR)
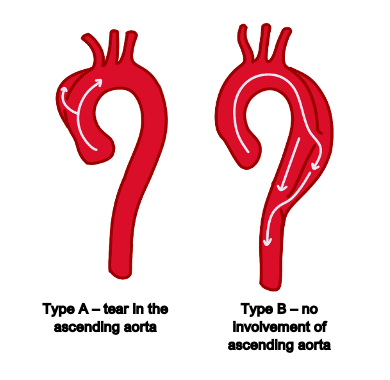
Aortic dissection
This is a tear in the tunica intima with blood flowing through a false lumen.
Type A dissections involve the ascending aortic arch at some point.
Type B describes dissections which have no involvement of the ascending aorta and are less common.
They share similar risk factors to the aortic aneurysms.
Symptoms
Sharp, tearing chest pain that radiates to the back between the scapulae
Hypertension
Complications
These can occur when the tear extends either backwards (towards heart) or distally
If a backward tear, it can lead to aortic regurgitation, an inferior MI due to right coronary involvement and pericardial tamponade (common cause of death)
If a forward tear, it can cause unequal arm pulses (radio-radial delay), a difference in BP between the arms and obstruction of the renal arteries giving kidney failure
Key Tests
CT angiography is the investigation of choice.
Management
Type A – surgical repair (BP should be controlled to between 100–120 mmHg)
Type B – can be managed conservatively, aim to reduce BP with IV labetalol

