These conditions are characterised by a restrictive pattern of spirometry.
They occur due to inflammation which leads to fibrosis (irreversible scarring) of the lungs, meaning they cannot expand fully, reducing the vital capacity.
Both the FVC and FEV1 are reduced in restrictive conditions. However, the FEV1/FVC ratio stays constant as both FEV1 and FVC decrease proportionally.

Different conditions cause fibrosis predominantly in the upper or lower zones.
| Upper Zone Fibrosis (BREASTS) | Lower Zone Fibrosis (BRAINS) |
| Berylliosis | Bronchiectasis |
| Radiation | Rheumatoid Arthritis |
| Extrinsic Allergic Alveolitis | Asbestosis |
| Ankylosing spondylitis | Idiopathic Pulmonary Fibrosis |
| Silicosis | Nitrofurantoin (+ amiodarone, bleomycin, methotrexate) |
| TB | Scleroderma |
| Sarcoidosis |
Interstitial Lung Diseases
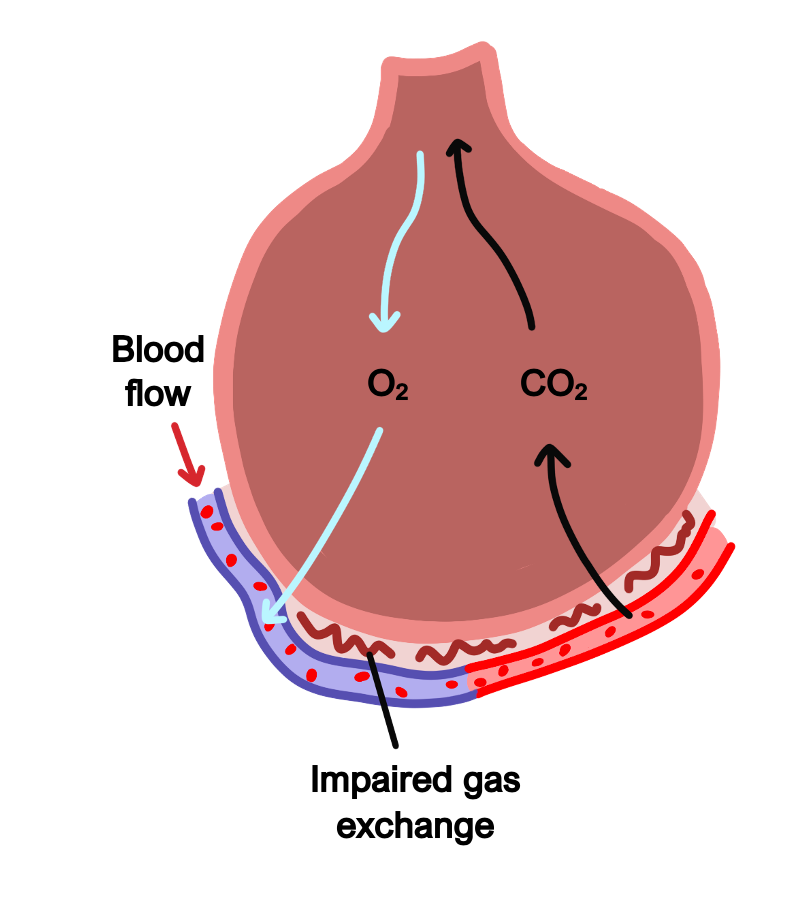
The term “interstitial lung disease” is an umbrella term that refers to conditions that cause fibrosis of the interstitial space (the space between the alveoli and capillaries surrounding the alveoli).
This fibrosis increases the diffusion distance for gases between the air in the alveoli to the blood in the capillaries, impairing gas transfer.
In addition, chronic inflammation decreases the elasticity and compliance of the lungs, reducing the total lung volume and vital capacity.
Symptoms
Dyspnoea on exertion
Non-productive cough
Cyanosis
Weight loss
Clubbing of the fingers
Pneumoconiosis
This refers to interstitial fibrosis caused by an immune reaction to the inhalation of foreign particles. This is often linked to occupational exposure, so it is very important to ask about work history.
These conditions are managed by avoiding further exposure and symptomatic management.
Silicosis
This is caused by the inhalation of silica (mining, pottery and slate workers).
On imaging, fibrotic nodules are visible in the upper zones of the lung and hilar lymph nodes show “eggshell” calcifications.
Silicosis is a risk factor for developing TB
Berylliosis
This disease is caused by exposure to beryllium (metal workers).
It leads to non-caseating granulomas and causes upper lobe fibrosis.
Asbestosis
This occurs due to the inhalation of asbestos fibres (commonly used in certain types of archaic insulation in buildings).
Asbestos most commonly causes pleural plaques which are benign.
However, exposure can also lead to lower lobe fibrosis, lung carcinoma and mesothelioma (cancer of the pleural lining). Mesothelioma occurs 20–40 years post exposure and patients may be eligible for compensation from their employers.
Coal Workers Pneumoconiosis (CWP)
This is a disease due to the repetitive inhalation of carbon dust.
This can lead to simple pneumoconiosis which is usually asymptomatic.
However, chronic exposure leads to progressive massive fibrosis (PMF).
Patients develop exertional dyspnoea and cough with black sputum.
Sarcoidosis
This is a disease characterised by granuloma formation in organs.
It typically involves the hilar lymph nodes causing respiratory symptoms.
Sarcoidosis can also cause lung fibrosis, leading to a restrictive pattern of disease.
There is no known cause, but it typically affects Afro-Caribbeans and young females.
Symptoms
Lung – progressive dyspnoea and dry cough, with inspiratory crackles
Skin – lupus pernio, cutaneous nodules
Hypercalcaemia (thirst, bony pain, confusion) due to uncontrolled production of activated vitamin D by granuloma macrophages

Key tests
Blood tests show elevated serum ACE, high Ca2+ and raised ESR
CXR/CT chest shows bilateral hilar lymphadenopathy and progressive fibrosis
Biopsy (e.g., from bronchoscopy) is diagnostic and shows noncaseating granuloma
Lung function tests show a restrictive pattern of disease
Management
Many people recover spontaneously and do not need treatment
If severe disease or symptomatic, may require immunosuppression, e.g., steroids
Idiopathic pulmonary fibrosis/Usual Interstitial Pneumonia (UIP)
This is the most common interstitial lung disease.
IPF is a diagnosis of exclusion whereby no underlying cause can be found.
It is seen more in the elderly and is about twice as more common in men.
Alveolar epithelial injury leads to TGF-β release to induce fibrosis.
The disease has a poor prognosis and only about a 50% five year survival rate.

Symptoms
Non-productive cough
Shortness of breath worsened by exertion
Fine inspiratory crackles
Clubbing
Key tests
Blood tests – may find ANA antibodies (30%) and rheumatoid factor (10%)
Restrictive spirometry pattern of disease
High resolution CT is the investigation of choice showing honeycombing fibrosis
Management
Pulmonary rehabilitation
Drugs which down-regulate fibrotic growth factors, e.g., pirfenidone, nintedanib
Definitive treatment is lung transplantation
Extrinsic allergic alveolitis (EAA)/Hypersensitive Pneumonitis
This is a disease which occurs after the repetitive inhalation of allergens (e.g., spores).
It is initially a type III hypersensitivity reaction with delayed type hypersensitivity (type IV) more in the chronic phase.
Acute inflammatory changes are seen in the alveoli, followed by granuloma formation in the chronic phase and fibrosis of the upper zones.
Causes
Pigeon fancier’s lung – due to avian proteins from the feathers or bird droppings
Farmer’s lung – due to inhalation of fungal spores
Malt worker’s lung – due to inhalation of Aspergillus clavatus
Symptoms
Acute – fever, chills, malaise, cough, chest tightness, dyspnoea, and rash
Chronic – insidious onset of cough, progressive dyspnoea, fatigue, and weight loss
Key tests
Lung function tests show a restrictive pattern of disease
CXR/HRCT shows radiological signs of fibrosis
Bronchoalveolar lavage can show a lymphocytosis
Management
In the acute setting, avoid the allergen and give oxygen if needed
Patients may require long-term steroids to prevent the hypersensitivity reaction


