The breathing system relies on creating a pressure gradient between the inside and external environment, which needs an intimate relationship between the lungs and chest wall.
– Lungs are lined by visceral and parietal pleura, which are separated by a thin layer of fluid.
The volume of thoracic cavity is determined by the outward recoil of chest wall + inward elastic recoil of lungs
– These opposing forces are balanced by small negative pleural pressure.

Breathing relies on increasing thoracic cage volume which then decreases intrapleural pressure
i) At the end of expiration, alveolar pressure (PA) = 0 and pleural pressure = -5. Therefore, transpulmonary pressure is +5 which keeps lungs inflated.
ii) In breathing, the diaphragm contracts decreasing the intrapleural pressure
iii) Alveoli expand causing a decrease in alveolar pressure below atmospheric pressure
iv) This resultant pressure gradient pulls in air from mouth
v) At end of inspiration, alveolar pressure = atmospheric pressure –> NO NET FLOW
vi) In expiration, muscles relax and PPl less negative and alveoli deflate –> Pa>PB forcing air out.
The mechanism of breathing is essential to understand how different conditions affect expiratory rates.
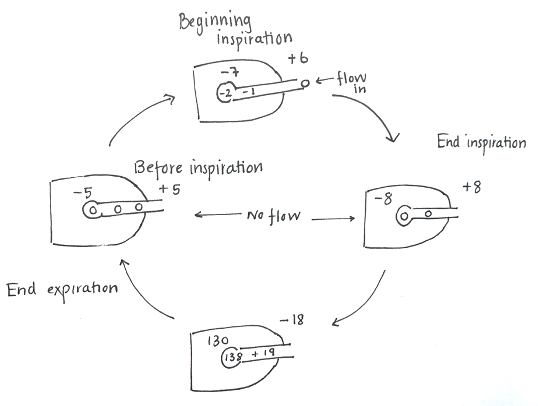
At the start of forced expiration, pleural pressure rises > atmospheric pressure.
– This raises alveolar pressure > pleural pressure (due to elastic recoil of lungs).
– Therefore, transpulmonary pressure is +8
As flow out is initiated, there is a progressive fall in pressure along the airway due to airway resistance, so transpulmonary pressure drops.
– At some point due to resistance the transpulmonary pressure reaches zero.
– This is called the equal pressure point.
– After this, transpulmonary pressure is negative resulting in airway collapse.
Hence conditions which increase airway resistance have lower equal pressure points, making it harder to force out the air. These are known as obstructive conditions.
Maximum flow rate is determined by the elastic recoil of the lungs (greatest at large lung volumes) and resistance to air.
Therefore, respiratory conditions which cause increased airway resistance and have less compliance are able to force out less air, and so have slower expiratory rates.
Alveolar ventilation
The purpose of breathing is to deliver oxygen to the tissues while removing carbon dioxide from the blood.
– One of the most important variables in determining gas exchange is alveolar ventilation = volume of fresh air actually reaching the lungs in one minute.
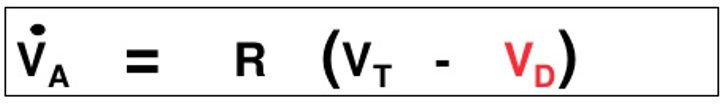
Alveolar Ventilation = Breathing Rate (Tidal Volume – Dead space)
Alveolar ventilation can be calculated from the volume of CO2 expired per unit time and the fraction [CO2]
This is because inspired air has no CO2 – therefore all expired CO2 must have come from the alveoli.
Alveolar ventilation = volume expired CO2 per minute/partial pressure CO2
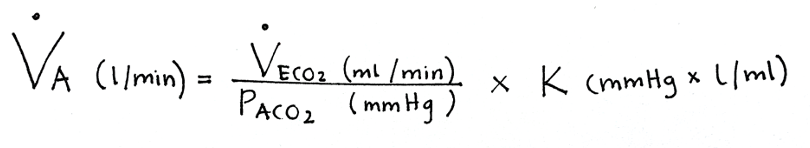
This equation shows that alveolar ventilation is inversely proportional to P(CO2).
– As P(CO2) is in equilibrium with the carbon dioxide in arterial blood, this shows that alveolar ventilation inversely proportional to arterial CO2.
– In exercise, to maintain a constant P(CO2), alveolar ventilation must rise to keep oxygen high and CO2 low.
P(oxygen) is also related to alveolar ventilation, but unlike P(CO2) it is not directly proportional. But the general rules are:
– Hyperventilation –> Carbon dioxide falls, oxygen increases
– Hypoventilation –> Carbon dioxide increases, oxygen decreases
| Atmospheric Air (mmHg) | Alveoli (mmHg) | |
| PO2 | 158 | 100 |
| PCO2 | 0.3 | 40 |
| PN2 | 596 | 573 |
| PH2O | 5.7 | 47 |
It is important that alveolar ventilation is matched to blood flow, which is monitored by the VA/Q ratio. This ratio tells us about the relationship between amount of air (VA) vs blood flow (Q):
– If the ratio is low (<0.8), there is not enough air compared to blood:
–> This is seen in obstructive respiratory conditions e.g. COPD featuring chronic bronchitis and asthma
– If the ratio is high (>1), there is not enough blood flow to lungs compared to air
–> This is seen in Pulmonary embolism
Control of breathing
Breathing is controlled by the brainstem (pons and medulla) using an intrinsic circuit. This relies on negative feedback mechanisms to control the rate of breathing.
– The variable which is under the closest control is arterial P(CO2) (set point 40mmHg).
This is monitored by central and peripheral chemoreceptors:
Central:
– Chemosensitive areas in the brain detect changes in pH.
– CO2 crosses the BBB and dissociates into H+ ions. High CO2 thus lowers the pH
– This fall in pH is detected by the chemoreceptors and leads to an increase in breathing rate.
N.B. If the CSF pH is displaced for a long period, there is a compensatory increase in HCO3 to buffer the acid.
– Hence one with chronic lung disease may have a compensated normal CSF pH despite raised arterial P(CO2)
– In these people, they rely on detecting P(O2) to control their breathing as they have a reduced central chemoreceptor drive.
Peripheral:
– Chemoreceptors are in carotid and aortic bodies these cells detect oxygen, CO2 and pH.
– Only these cells can use hypoxia as a stimulus to increase breathing rates
Using these systems, it is possible to live in extreme climates (altitude) where partial pressure of oxygen is low:
– Hyperventilation – lowers P(CO2) and increases P(O2)
– Increase in [RBC] concentration to increase [haemoglobin] and oxygen carrying capacity
– Increased 2,3-DPG – moves the oxygen dissociation curve right to help unloading oxygen at tissues.

