Acute Respiratory Distress Syndrome (ARDS)
This refers to widespread inflammation at the alveolar-capillary interface, increasing the permeability of the alveolar capillaries.
Fluid moves out of the permeable capillaries, resulting in non-cardiogenic pulmonary oedema that impairs ventilation.
ARDS can progress to organ failure and carries a high morbidity and mortality risk.

Causes
Direct – this is due to direct lung injury (such as smoke inhalation)
Indirect – due to conditions which cause inflammation (such as sepsis, shock and acute pancreatitis)
Symptoms
Acute onset tachypnoea, dyspnoea
Bilateral inspiratory crackles
Low oxygen saturations and cyanosis with respiratory distress
Key tests
ABG shows hypoxia which maybe resistant to oxygen therapy
CXR/CT – shows bilateral infiltrates
Echocardiogram – needed to rule out cardiac failure
Diagnosis
There are 4 key criteria for diagnosing ARDS:
Acute onset (within 1 week of a known risk factor)
Bilateral infiltrates (e.g., pulmonary oedema) not explained by other lung pathology
Respiratory failure not due to heart failure
Decreased PaO2/FiO2 ratio (< 40 kPa): indicates poor oxygenation
Management
This requires cardiorespiratory support whilst you correct the underlying cause
Respiratory support – low tidal volume mechanical ventilation
Cardiac support – maintain cardiac output with inotropes and vasodilators
Pneumothorax
This refers to an accumulation of air in the pleural space. It can be classified as:
Primary
This occurs in a patient without a known respiratory disease, usually due to rupture of a subpleural air bulla (typically affects young, thin men).
Secondary
This occurs in a patient with a chronic respiratory disease. The aetiology depends on the underlying disease (e.g., in cystic fibrosis, endobronchial obstruction by mucus leads to increased pressure in the alveoli, leading to alveoli rupture).
Tension
This occurs due to a penetrating chest wall injury and is an emergency. The injury acts like a one-way valve, which allows air to enter but not escape the pleural space.
As more air enters the pleural cavity, this can lead to compression of the SVC/IVC, leading to haemodynamic compromise and death.
Signified by deviation of the trachea and mediastinum away from the affected side.

Risk factors
Lung disease (asthma, COPD)
Trauma, i.e., can be iatrogenic e.g., mechanical ventilation, central line insertion
Connective tissue diseases (Marfan)
Catamenial pneumothorax, due to endometriosis in menstruating women
Symptoms
Dyspnoea
Tachycardia, tachypnoea
Pleuritic chest pain
Signs
Reduced lung expansion
Reduced breath sounds and hyperresonant percussion on affected side
Key tests
CXR shows lung markings do not reach chest wall
Management
For Tension
If you suspect a tension pneumothorax, you should treat before getting a CXR
Insert a 14 G cannula into the 2nd intercostal space mid-clavicular line and subsequently insert a chest drain

For Spontaneous
Management used to depend on the size of the pneumothorax, which guided whether to monitor the patient, needle aspirate or insert a chest drain
The latest guidance by the British Thoracic Society focuses more on whether the patient is symptomatic and whether they can be managed conservatively
Asymptomatic – conservative management (review regularly as outpatient)
Symptomatic and high-risk characteristics (e.g., hypoxia, underlying lung disease, if age > 50 years old with significant smoking history) – needle aspiration or chest drain
Symptomatic without high-risk characteristics – management is guided based on patient preference (e.g., procedure avoidance if they wish for this)
Anaphylaxis
This refers to a life-threatening hypersensitivity reaction.
It arises within seconds-minutes of exposure to the allergen, due to excessive mast cell degranulation releasing vast amounts of histamine.
Common allergens include food (nuts, dairy, shellfish); medications (including penicillin) and blood transfusions.
Symptoms
Respiratory – bronchospasm with dyspnoea and wheezing
Cardiovascular – distributive shock, i.e., hypotension with tachycardia
Skin – angioedema and urticarial rash with pruritus
ENT – tongue swelling and laryngeal oedema (can obstruct the airway)

Management
The most important immediate treatment is intramuscular adrenaline.
Hydrocortisone and Chlorphenamine are used after the IM adrenaline is given.
Patients should be observed for 6–12 hours from symptom onset, as a biphasic reaction can occur in about a fifth of patients.
To determine whether it is true anaphylaxis, serum tryptase levels are taken between 4–12 hours after onset of anaphylaxis (should be raised).
Patients require monitoring in a high dependency area due to risks of cardiovascular collapse and further deterioration.

Carbon Monoxide Poisoning
This is an acute condition which occurs due to the inhalation of carbon monoxide.
It commonly occurs in house fires and in poorly maintained housing.
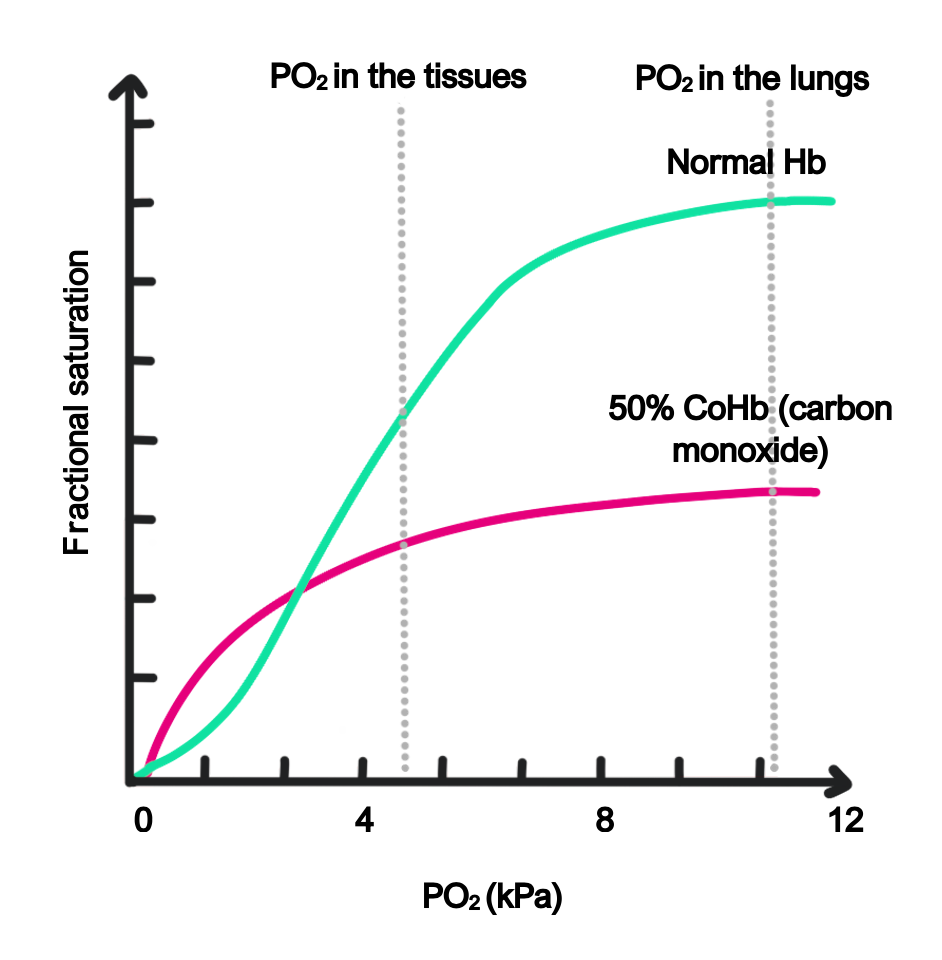
CO has greater affinity for haemoglobin than O2, reducing haemoglobin’s ability to deliver O2 to the respiring tissues.
Carbon monoxide binds haemoglobin to form carboxyhaemoglobin (COHb):
In non-smokers, the ratio of carboxyhemoglobin to haemoglobin can be up to 5%
In smokers, levels of COHb are usually < 10%
In symptomatic CO poisoning, COHb is usually between 10–30%
In severe toxicity, COHb is > 30%
Symptoms
Headache
Nausea, vertigo and confusion
Can cause arrhythmias, fever, reduced consciousness and death
“Pink” skin and mucosae
Management
100% oxygen (target SpO2 is 100%)
Consider hyperbaric oxygen, especially if there is loss of consciousness, neurological signs or the patient is pregnant
Pleural effusion
This is defined as fluid in the pleural space which surrounds the lungs, divided into transudate and exudate:
Transudate
This is fluid in the pleural space which has < 25 g/L protein.
It is caused by increased hydrostatic pressure in the pleural capillaries (increased fluid in the capillaries) or decreased oncotic pressure (reduced albumin/protein).
This forces water out of the capillaries into the pleural space.
Causes
Heart failure (most common cause)
Hyperalbuminemia (e.g., secondary to nephrotic syndrome liver failure)
Hypothyroidism
Meigs syndrome – triad of ovarian fibroma and ascites with pleural effusion
Exudate
This refers to fluid which has > 35 g/L protein. It occurs due to increased leakiness of pleural capillaries, which allows protein into the pleural space.
Causes
Infection, e.g., pneumonia (most common cause), TB, abscess
Connective tissue diseases, e.g., SLE, rheumatoid
Malignancy
Symptoms
Effusions can be asymptomatic if small
Shortness of breath, dry cough and pleuritic chest pain
On examination, reduced chest expansion, breath sounds and stony dull percussion
Key tests
CXR – this shows blunting of the costophrenic angles
Ultrasound – shows presence of pleural fluid
Pleural tap – the diagnostic test which involves aspiration using a fine needle. This is sent to the lab for biochemistry analysis (e.g., checking for malignant cells) and microscopy, culture and sensitivity (MC&S).
Management
If symptomatic or evidence of empyema, a chest drain maybe required.
Treat the underlying cause, e.g., antibiotics for pneumonia
Patients with recurrent pleural effusions may need pleurodesis, which is a procedure that binds the 2 visceral and parietal pleurae together, stopping fluid from reaccumulating in the space between them.

