Epididymo-orchitis
This is inflammation of the epididymis (and the testes)
Causes
Bacteria, e.g., chlamydia, gonorrhea, E. coli
Viruses, e.g., mumps (in teenage males)
Drugs e.g., amiodarone
Symptoms
Acute onset tender swelling (confined to epididymis)
Dysuria, sweats, fever
Management
Treat the underlying cause, e.g., antibiotics if due to an STI
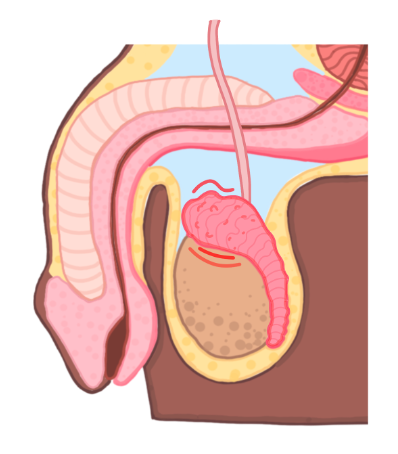
Testicular torsion
This refers to twisting of the spermatic cord, usually in adolescents
It can cut off the blood supply to the testes resulting in ischaemia
Symptoms
Acute onset testicular pain
Absence of the cremasteric reflex
Abdominal pain, nausea and vomiting
Prehn’s sign seen (where raising the testicle does not reduce pain)

Key tests
Can be diagnosed clinically if the history and exmination is comvincing
Ultrasound can be used if diagnosis unclear
Management
This is a surgical emergency – aim to treat within 6 hours
Orchidectomy (removal of testes) is required if the testicle is non-viable
Hydrocele
This is a fluid collection within the tunica vaginalis covering the testis and scrotum.
It occurs in infants due to incomplete closure of the processus vaginalis.
It can also occur in adults as the presenting feature of testicular cancer.
Symptoms
Non-painful, soft scrotal swelling limited to the scrotum (can get “above it”)
It can be transilluminated, unlike solid tumour
Hydrocele will appear a soft red whereas a tumour is opaque to the light

Key tests
In adults, can use ultrasound to exclude tumour
Management
Usually requires surgical fixation to close the processus vaginalis
Varicocele
This refer to dilation of a spermatic vein due to blocked venous drainage.
It usually occurs on the left, as the gonadal vein drains into the renal vein before the IVC, in comparison to the right side.
It is sometimes seen if a patient has a left-sided renal cell carcinoma.
Symptoms
Scrotal swelling which gives a dull ache, but can be asymptomatic
Key tests
Doppler ultrasound
Management
Does not require treatment unless it is symptomatic
Embolisation if painful (this diverts blood away from an enlarged vein in your scrotum using a coil to block the vein)
Cryptorchidism
This is a failure of one or both testicles to descend into the scrotum.
As a result, the higher temperature within the abdomen suppresses sperm production.
This leads to atrophy and significantly increases the risk of testicular cancer.

Symptoms
Absent testes in the scrotum (can be bilateral)
Predisposes to infertility later in life
Management
Orchidopexy, a procedure which moves the undescended testicle into the scrotum and permanently fix it there, usually performed before the age of 18 months
Testicular Cancer
This is most common cancer in young males which arises from germ cells or sex cords.
Most tumours are malignant germ cell tumours
Risk Factors
Undescended testis
Infertility
Having a relative with testicular cancer
Symptoms
Present as a solid non-tender mass which cannot be transilluminated
Can give rise to a secondary hydrocele causing pain
Can present with established metastases in the lungs or abdominal masses
Key tests
1st line is Ultrasound
Check tumour markers AFP, LDH, β-hCG – these are elevated in germ cell tumours
Tumours are usually not biopsied due to risk of disseminating the tumour cells
CXR and PET-CT scan can be used for staging of the cancer
Management
Radical orchidectomy (complete removal of the testes) and chemo/radiotherapy

Germ Cell Tumour
This is the most common type of testicular cancer occurring in ages 15–40.
The germ cell tumours are usually divided into two main types:
Seminoma
This is a malignant tumour of big cells which look like spermatogonia.
They have a clear cytoplasm and central nuclei.
These are very responsive to radiotherapy and metastasise late.
Therefore, they are relatively easier to treat and have a good prognosis
Non-seminoma
This includes a variety of tumours, which metastasize early
Subtypes of Non-Seminomas
Sex-Cord Tumour
This is a (usually benign) proliferation of sex-cord cells and is split into 2 types:
Subtypes of Sex-cord tumours
Lymphoma
This is a proliferation of white blood cells, usually large B-cells
It is the most common testicular mass in men above the age of 60 years

