This is a group of disorders which can affect various parts of the nephron, leading to specific symptoms.
The symptoms reflect either an inability to reabsorb or excess reabsorption of solutes in the various segments.
Fanconi syndrome
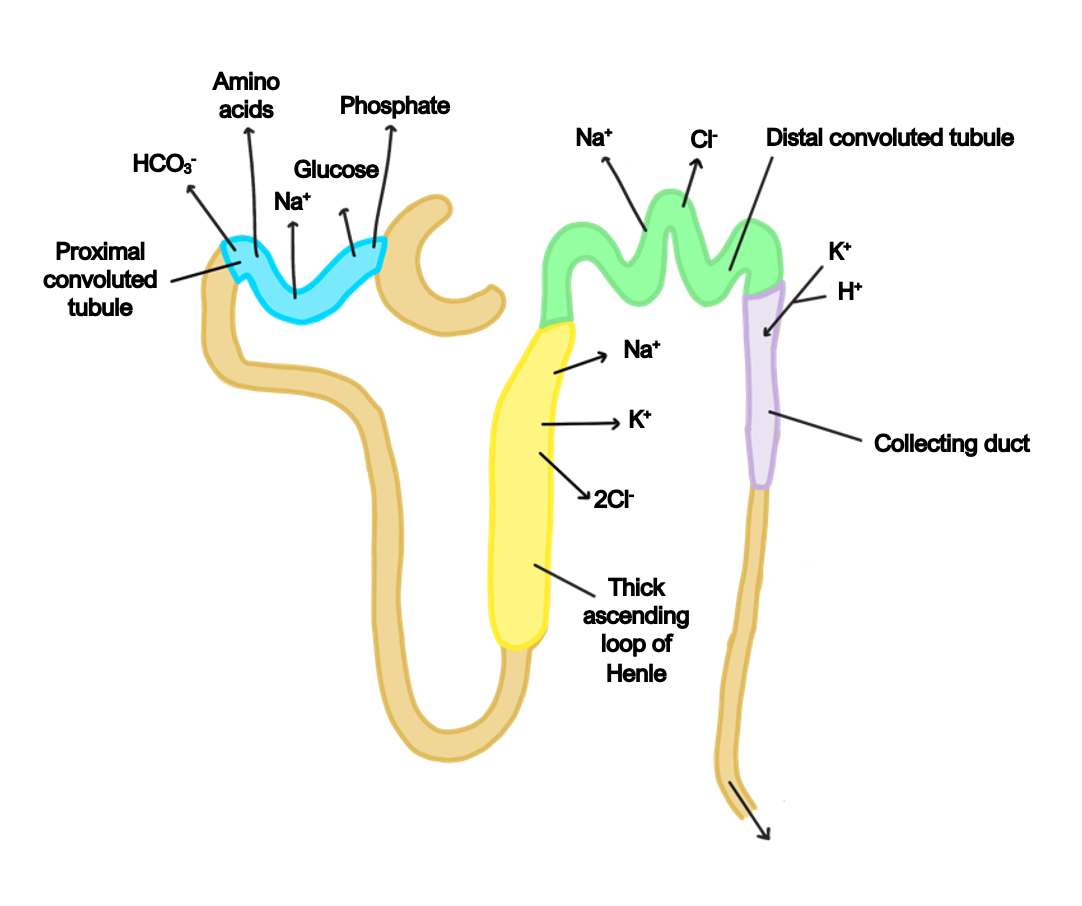
This is a disorder causing impairment of PCT function, preventing solute reabsorption.
It can be either inherited or acquired.
Symptoms
Glycosuria, aminoaciduria, uricosuria and phosphaturia
Phosphate loss can cause bone demineralisation resulting in osteomalacia
Management
Phosphate replacement is important
Bartter syndrome
This is an inherited condition which results in an impairment of salt reabsorption in the thick ascending loop of Henle, which usually affects children.
Sodium concentration increases further in the DCT, increasing the gradient for exchange with K+ and H+.
Symptoms
Hypokalaemia, hypochloraemia and metabolic alkalosis
The severe loss of electrolytes can affect growth in children
Management
Electrolyte replacement
NSAIDs and potassium sparing diuretics are used
Gitelman syndrome
This is an impairment of the NaCl cotransporter in the DCT.
It is milder than Bartter syndrome and usually presents in adults.
Symptoms
Mimic thiazide diuretic effects – hypokalemia, metabolic alkalosis, gout
Management
Electrolyte supplementation
Renal Tubular Acidosis (RTA)
This is a condition involving accumulation of acid in the body, due to a failure of the kidneys to acidify the urine.
The term RTA is only used for patients with poor urinary acidification but otherwise well-functioning kidneys.
It can be due to a primary tubule pathology (type 1 and 2) or secondary to low aldosterone or excessive use of potassium-sparing diuretics.
The problem is the metabolic acidosis which can demineralise bone.
Type 1
This is due to a failure of H+ excretion from the distal parts of the nephron, due to dysfunction of H+/K+ antiporter.
It can be primary (genetics) or secondary to autoimmune conditions and toxins.
It leads to hypokalaemia, hypocalcaemia and hyperchloraemia
High Ca2+ in urine increases the risk of urinary stones and nephrocalcinosis.
Symptoms
Gives hypokalemia, hypocalcaemia and hyperchloremia
High acid demineralizes bone (osteomalacia)
High Ca2+ in urine gives urinary stone + nephrocalcinosis (Kidney Ca2+ deposition)
Urine is not acidified
Management
HCO3- replacement to buffer acid and treat underlying disease
Type 2
This is due to an impairment of HCO3– reabsorption in the PCT, leading to urinary HCO3– loss, which contributes to a metabolic acidosis.
The loss of bicarbonate ions means that Na+ ions are held back as a cation, which increases the gradient for K+ loss.
The distal intercalated cells still work, so the acidosis is less severe than type 1.
It can be secondary to the ingestion of heavy metals and certain drugs.
Causes
Heavy metals
Drugs
Usually accompanied with Fanconi syndrome
Symptoms
Acidosis demineralizes bone and gives hypokalemia
Management
HCO3- and K+ replacement
Type 3
This is a combination of type 1 and 2 RTA which occurs in children
Type 4
This is a secondary RTA which is due to hypoaldosteronism
Causes
Aldosterone deficiency or resistance (due to drugs e.g. K+ sparing diuretic)
Symptoms
Gives hyperkalaemia, hypotension and metabolic acidosis
Acute Tubular Necrosis (ATN)
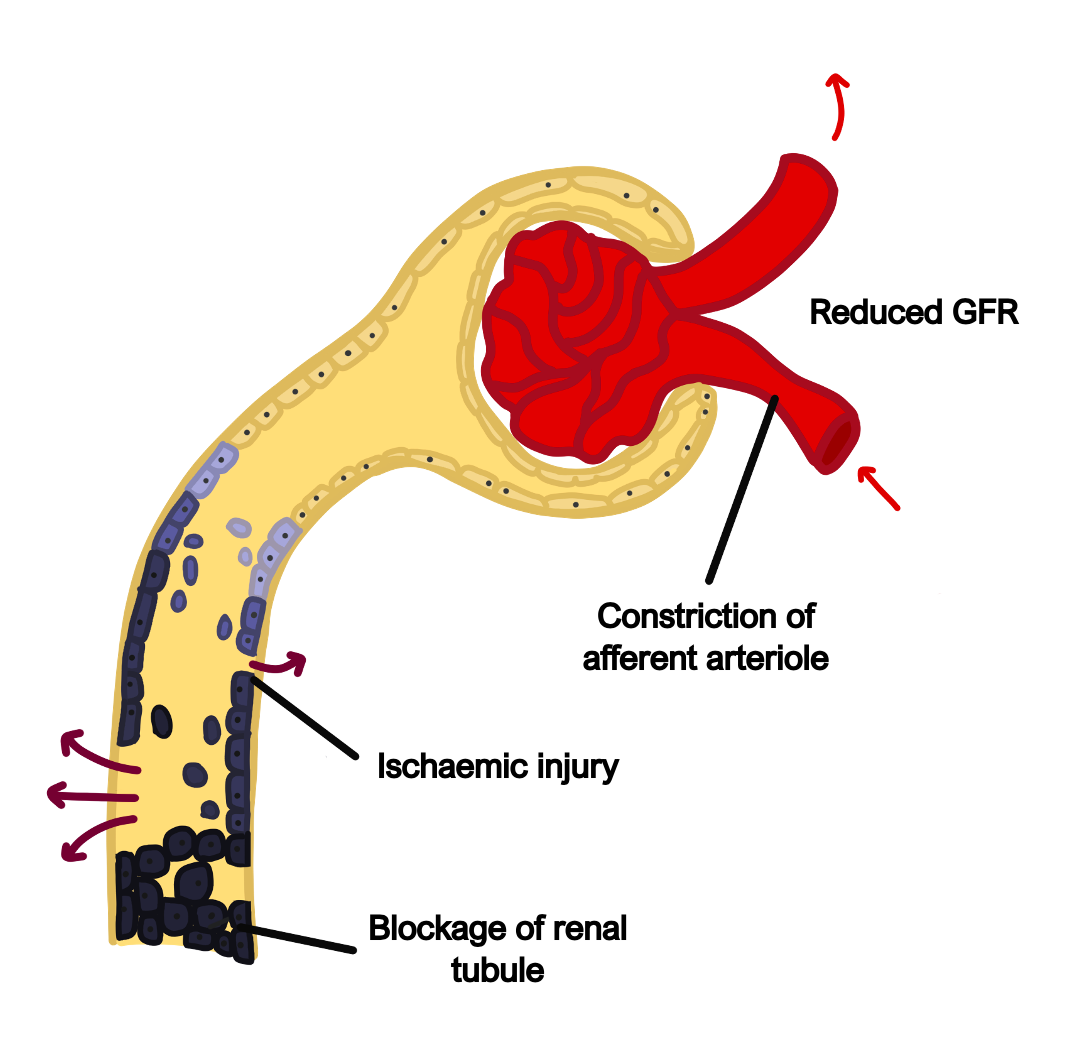
This is a condition resulting in necrosis of the tubule lining cells.
The necrotic cells fall off and can then obstruct the tubules decreasing the GFR
Causes
Poor renal blood flow (hypovolaemic/septic shock)
Drugs – NSAIDs, aminoglycoside antibiotics, iodine
Heavy metal poisoning – lead
Endogenous agents – urate (breakdown of tumour cells), so allopurinol used before chemotherapy to reduce urate-induced ATN
Symptoms
Oliguria phase often then followed by polyuria phase
AKI – poor urine output with raised urea and creatinine
Hyperkalaemia and metabolic acidosis
Key tests
Urine microscopy – presence of muddy brown, granular casts in urine
Blood tests – raised Cr and Urea
Kidney biopsy if diagnosis is unclear
Management
Hydration and cessation of nephrotoxic substance
Recovery is seen within a few weeks as the PCT cells are constantly replaced
Acute interstitial nephritis (ATIN)
This is a hypersensitivity reaction which causes inflammation of the nephron and the surrounding interstitial space
Causes
Drugs (NSAIDs, penicillin, diuretics, allopurinol)
Infection by Staphylococci
Underlying connective tissue diseases
Symptoms
Inflammatory signs – rash, low grade fever, joint pain
Renal dysfunction – oliguria (low urine), azotemia, hypertension
Key tests
Bloods may show an eosinophilia which demonstrates that it is an allergic mediated inflammatory reaction
Urine microscopy – shows white cell casts seen in the urine
Kidney biopsy – shows interstitial oedema and inflammatory cell infiltration
Management
Stop the causative agent.
Can also give steroids to dampen the immune system
Chronic interstitial nephritis (CTIN)
This is a chronic condition of the interstitium and tubules.
Chronic inflammatory episodes eventually lead to fibrosis of the tubules, leading to a deterioration in kidney function.
If left untreated, these patients will eventually suffer from chronic kidney disease.
Causes
Most commonly due to drugs or infection
Management
Stop causative agent and treat the progressive CKD

