Acute prostatitis
This is acute inflammation of the prostate, which usually occurs in infection
Causes
Young adults – Chlamydia trachomatis, Neisseria gonorrhoeae
Older Adults – E. coli
Symptoms
Dysuria, urinary frequency, and suprapubic pain
Can cause urinary retention leading to pain and haematospermia
Systemic symptoms, e.g., fevers
Key tests
DRE gives tender prostate and secretions reveal bacteria
Management
Antibiotics e.g. levofloxacin (Quinolone) or Trimethoprim
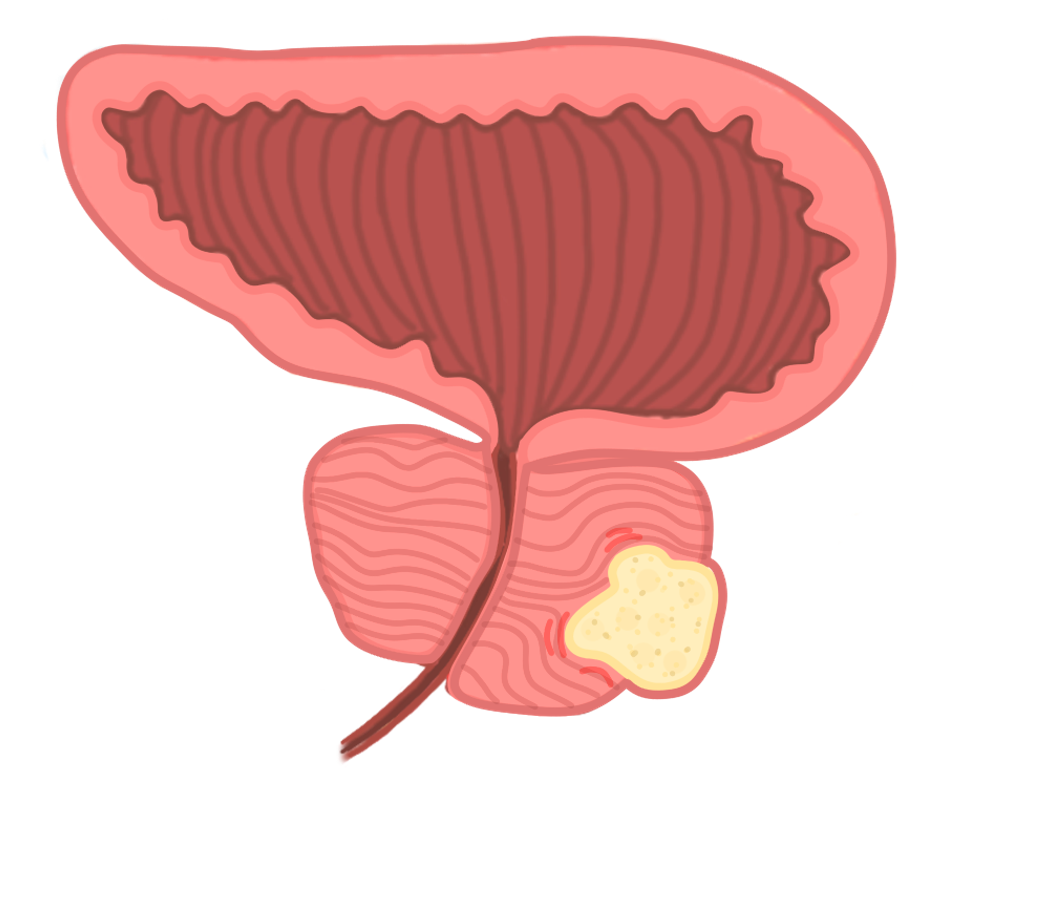
Benign prostatic hyperplasia (BPH)
This refers to hyperplasia of the prostate which occurs with age and is common.
It does not increase the risk of cancer, as it is the central zone of the prostate which enlarges, rather than the peripheral layer in prostate cancer.
It is linked to testosterone release, which is converted to DHT by 5-alpha-reductase.
Symptoms
Voiding – weak flow, hesitancy, postterminal dribbling
Storage – increased urgency, urinary frequency, incontinence
Microscopic haematuria
Impaired bladder emptying causes increased risk of diverticula and UTI

Management
Conservative – avoid caffeine and alcohol, bladder training to control urgency
a1 antagonists (e.g., tamsulosin) relaxes smooth muscle to allow urination
5 alpha-reductase inhibitors (finasteride) blocks conversion of testosterone to DHT
Transurethral resection of the prostate (TURP) is a surgical option
Prostate Cancer
This is a malignant proliferation of the prostate gland cells that arise from the posterior zone of the prostate. It is the most common cancer in men.
It does not cause the urinary symptoms very early on unlike BPH.
It often spreads to the lumbar spine and pelvis, resulting in bony metastases.
It is associated with in an increase in alkaline phosphatase (ALP) and prostate serum antigen (PSA).
Risk factors
Age (80% in men > 80)
Family history
Race (high in Afro-Caribbean)
Diet high in unsaturated fat
Symptoms
Lower urinary tract symptoms (nocturia, hesitancy, poor stream, dribbling)
Microscopic haematuria
Weight loss
Bone pain due to metastases
Key tests
Digital rectal examination – hard, irregular prostate (non-tender)
Prostate serum antigen – a serum PSA > 10 ng/mL increases the risk of cancer
1st line imaging is MRI – can be followed by transrectal US and biopsy to confirm
Grading
This is done using the Gleason grading system, based on architecture – higher score is worse
A score (1-5) is given for two separate areas on biopsy, based on how abnormal the cells appear.
Management
The definitive treatment is surgery (radical prostatectomy)
Medical therapy includes flutamide (androgen receptor antagonist) and continuous GnRH analogs (e.g., leuprolide) to inhibit release of pituitary gonadotrophs
Other treatment options include brachytherapy, a type of internal radiotherapy.

