This refers to a group of signs and symptoms secondary to glomerular disease.
It reflects inflammatory damage to the glomerulus which increases the permeability to proteins and blood causing proteinuria and haematuria.
Left untreated, it can progress to end-stage renal failure.
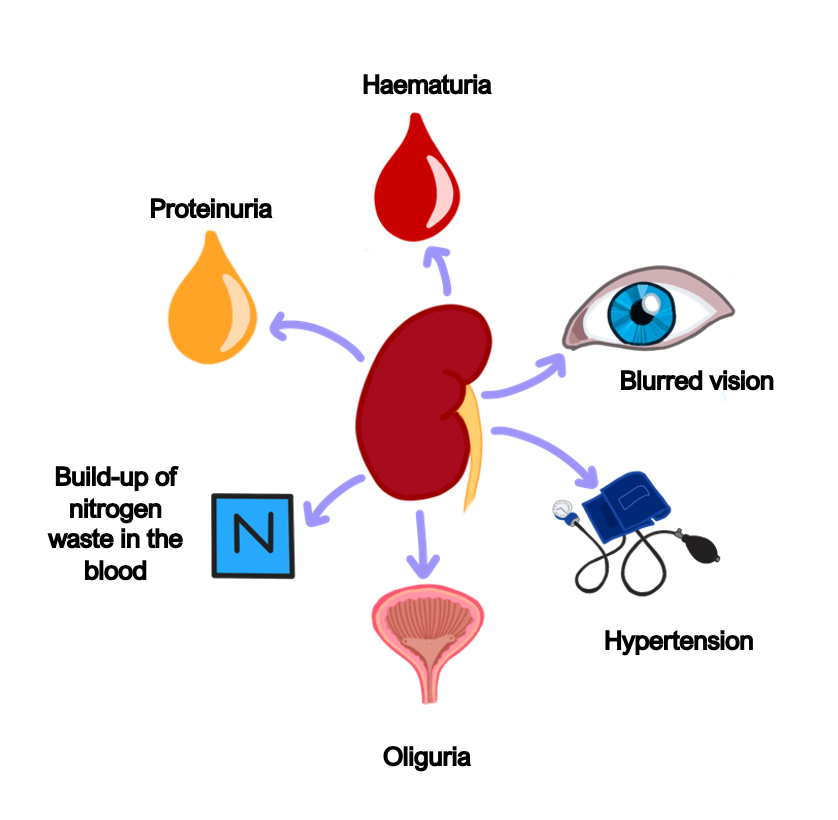
Symptoms
Haematuria
Less proteinuria (< 3.5 g/24 h)
Hypertension and blurred vision
Oliguria – low urine output
Azotemia – high urea/creatinine
Can progress onto renal failure
Key tests
Kidney biopsy
There are many specific conditions which give rise to nephritic syndrome, which have specific treatments:
IgA nephropathy
This is most common cause of nephritic syndrome, called Berger’s disease
It occurs due to IgA immune complexes being deposited in the mesangium of the glomerulus.
It is usually seen in young males and is associated with alcohol and coeliac disease.
Symptoms
The classic presentation is macroscopic haematuria, usually 1–2 days after URTI.
The condition carries a good prognosis and is unlikely to lead to CKD.
Biopsy findings
Shows IgA deposition in glomerulus
Management
Corticosteroids
Henoch-Schonlein purpura (HSP)
This is similar to IgA nephropathy, but in addition, there is also IgA deposition in other parts of the body such as the skin and joints (IgA vasculitis)
It leads to symptoms of IgA nephropathy, as well as arthritis and a typical purpuric rash on the extensor surfaces.
It is usually a self-limiting illness, but steroids can also be given.
Symptoms
IgA Nephropathy
Arthritis
Rash on extensor surfaces
Management
Steroids
Analgesia for joint pain (it is usually self-limiting)

Post-Streptococcal Glomerulonephritis
This is a complication which arises 1–2 weeks after infection with group A beta-haemolytic streptococcal bacterial infection.
Antibodies produced against the bacteria lead to immune complex formation which then end up getting deposited in the glomerulus, causing inflammation.
It usually self-resolves in children, but some adults can get a rapidly progressing glomerulonephritis, causing haematuria as well as other signs of nephritic syndrome
Symptoms
Haematuria
Other signs of full nephritic syndrome (hypertension + proteinuria/oedema)
Key tests
Blood tests – check for anti-streptolysin antibodies or DNase antibodies
Biopsy – endothelial neutrophil proliferation giving granular “starry sky” appearance
Management
Antibiotics to clear bacteria
Supportive treatment for renal dysfunction
Anti-GBM disease
This is a disease which used to be called Goodpasture’s disease, which occurs due to autoantibodies against type IV collagen.
This causes damage to the exchange surfaces which rely on the basement membranes, notably the lungs and kidney.
It leads to a rapidly progressive nephritic syndrome, as well as lung symptoms, including shortness of breath and pulmonary haemorrhage leading to haemoptysis.
Key tests
Blood tests – shows the present of anti-GBM antibodies
Kidney biopsy – shows linear IgG deposits in membrane on renal biopsy. These lead to crescent formation, which is the histopathologic hallmark of anti-GBM disease
Management
Plasmapheresis can be used remove antibodies form blood
Immunosuppression is the mainstay of treatment
Alport syndrome
This is a genetic X-linked dominant condition the protein chain of type IV collagen
This causes the glomerular basement membrane to be excessively thin, meaning it can easily tear.
Symptoms
Presents in childhood with microscopic haematuria, progressing to renal failure
Bilateral sensorineural hearing loss
Retinitis pigmentosa and blindness
Key tests
Renal biopsy show splitting of lamina densa
Management
Definitive management is a kidney transplant.
But some transplant patients can develop anti-GBM antibodies which can cause graft dysfunction.

