Parkinson’s disease
This is a disease where the dopaminergic neurons in the substantia nigra are progressively lost, resulting in the development of symptoms.
Parkinsonism can be drug-induced (gives rapid-onset bilateral motor symptoms)
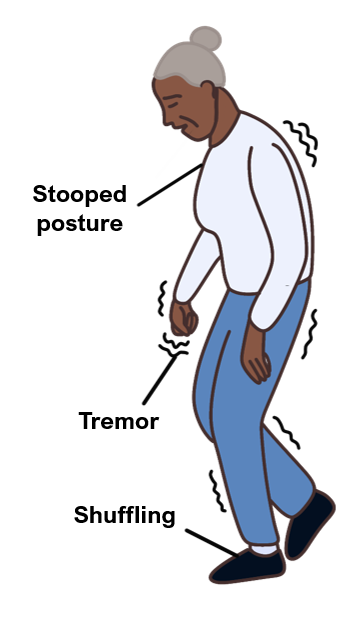
Symptoms
Tremor, described as a pill-rolling motion of thumb over fingers, which is usually worse at rest and typically improves with movement
Bradykinesia – slow initiation of voluntary movements
Hypertonia – increased muscle tone, which gives cogwheel rigidity in the extremities
Postural instability and shuffling/festinant gait (pitched forward gait)
Expressionless face (“mask-like”)
Psychiatric – depression (most common symptom), dementia and psychosis
Micrographia, anosmia
Autonomic dysfunction (postural hypotension and constipation)
Key tests
It is a clinical diagnosis. SPECT (DaT scan) shows reduced dopaminergic activity in basal ganglia
Management
1st line is levodopa (often combined with dopa decarboxylase inhibitor, e.g., carbidopa, dopamine agonist (such as rotigotine) or MAO-inhibitor (such as selegiline)
2nd line is dual therapy or COMT inhibitor (entacapone)
Parkinson Plus Syndromes
Multiple Sclerosis
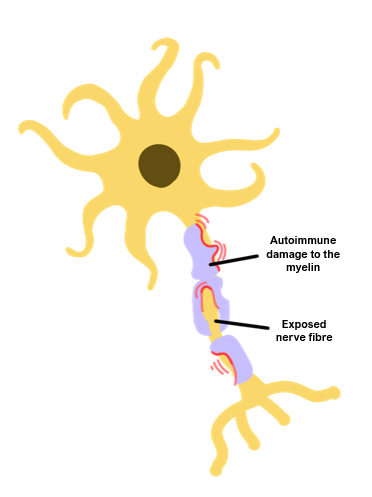
This is an autoimmune disorder against the CNS oligodendrocytes which produce myelin, which eventually leads to axonal loss.
It is the commonest cause of chronic neurological disability in young adults.
All sub-types, except for primary progressive, have a female preponderance.
Risk factors
Family history
Low vitamin D
Smoking
HLA-DR2 serotype
Living away from the equator
Infectious mononucleosis
Female gender
Types
Symptoms
Presents with relapsing neurological deficits with periods of remission
Vision – optic neuritis, saccadic movements, desaturation of red-green colour vision
Sensory – asymmetrical pins and needles, trigeminal neuralgia
Motor – UMN symptoms, e.g., spasticity, muscle weakness
Cerebellar – ataxia, tremor
Cognitive – “brain fog”, memory impairment, executive dysfunction
Autonomic dysfunction – incontinence, sexual dysfunction, and fatigue
To be diagnosed, there must be “dissemination in time and space”.
This means that there must be more than one episode affecting more than one part of the nervous system.
Key tests
MRI – this is used to exclude other causes; contrast enhancement shows active disease, whereas lesions that don’t enhance are older lesions, known as plaques.
Lumbar puncture – shows IgG (oligoclonal bands) and myelin basic protein in CSF
CSF oligoclonal bands shows CNS inflammation and, if they’re not present in a concurrent serum sample, then it supports diagnosis of MS.
Management
Address symptoms accordingly – e.g., baclofen can be used for spasticity
Acute flare – high-dose steroids for 3–5 days (shorten length of relapse)
Chronic – disease modifying therapies reduce relapse frequency, e.g., β-interferon, fingolimod, and monoclonal antibodies, e.g., natalizumab (mAb against α4-integrin)
Huntington disease
This is an autosomal dominant disorder caused by trinucleotide repeats (CAG) in the huntingtin gene, leading to the formation of abnormal huntingtin protein.
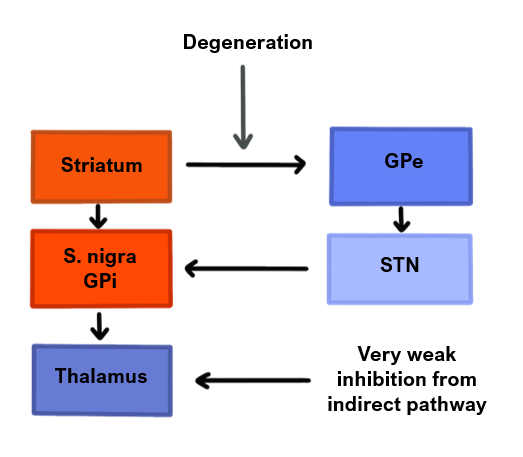
The disease affects the caudate nucleus of basal ganglia initially, and then causes progressive loss of neurons in other brain regions.
It results in weak inhibition from the indirect pathway of the basal ganglia, allowing unnecessary movements.
This leads to excessive uncontrolled movements, which is characteristic of the disease (although not specific) usually starting around age 35–45.
Symptoms
Irritability and incoordination
Chorea (uncontrolled, hyperkinetic movements)
Behavioural problems, depression and progression to dementia
Management
Supportive management, including tetrabenazine, benzodiazepines and antipsychotics as there is no cure available
Spongiform encephalopathy
This is a group of rare degenerative diseases, caused by abnormal prion proteins in the brain, leading to misfolded normal proteins and subsequent brain damage (including formation of holes in the brain, thus causing its “spongiform” appearance).
Creutzfeldt-Jakob disease (CJD)
The most common spongiform encephalopathy, which usually occurs sporadically.
Variant CJD
This is a form seen in younger patients (average age is 25 years). It can very rarely be transmitted through dietary intake and gives anxiety and withdrawal early.
Symptoms
Rapidly progressive dementia
Myoclonus (spasmodic, jerky contraction of groups of muscles)
Can have ataxia (cerebellum involvement) and eye signs (diplopia, field defects
Key tests
Lumbar puncture – CSF shows presence of 14-3-3 protein; RT-QuIC assay can be used to break prion aggregates, which then can replicate sufficiently to be measured
EEG shows biphasic sharp waves
MRI shows hyperintensity in basal ganglia and thalamus
Definitive diagnosis is only available at post-mortem
Management
No treatment available and the condition usually has a poor prognosis

