Chlamydia
This is a condition which is caused by the bacteria Chlamydia trachomatis.
It is the commonest sexually transmitted disease in the UK.
It is spread through all types of sex and can be passed to the baby during childbir
Symptoms
Often the infection is asymptomatic
In females, can cause vaginal bleeding, discharge and deep dyspareunia
In males, can cause urethritis (dysuria and discharge)
Eye disease – can cause blindness
Joints – often a cause of reactive arthritis
Risk factor for pelvic inflammatory disease (PID) in women, leading to infertility
Key tests
Investigation of choice is nuclear acid amplification tests (NAAT)
In women – 1st line is vulvovaginal swab (not urine or cervical swab)
In men – 1st line is urine test
Management
Antibiotics – oral doxycycline (for 7 days) or oral azithromycin (1 to 2 days)
If pregnant – azithromycin, erythromycin or amoxicillin
Gonorrhoea
This is due to the bacteria Neisseria gonorrhoeae, a Gram-negative diplococcus.
It gives similar symptoms to chlamydia, with additional complications.
There is no vaccine available, and reinfection is common due to antigenic variation.
Symptoms
In females, can cause vaginal bleeding, discharge, and deep dyspareunia
In males, can cause urethritis (dysuria and discharge) and urethral strictures
Can also cause infections of the rectum and the pharynx
Complications
Disseminated gonococcal infection (due to the spread of bacteria in the bloodstream from the genitals). Initially gives tenosynovitis, migratory polyarthritis and dermatitis
Fitz-Hugh-Curtis syndrome – inflammation of the liver capsule and RUQ pain
Key tests
Nuclear acid amplification tests (NAAT) of vulvovaginal swab or urine (used in men)
Management
1st line is single dose intramuscular ceftriaxone
If the strain is known to be sensitive to oral ciprofloxacin, a single dose of ciprofloxacin can be given
Syphilis
This is a condition due to Treponema pallidum, a spirochete bacterium.
It is transmitted by sexual contact or during pregnancy from the mother to her baby.
The infection consists of three stages, that increases in severity.
Symptoms
Primary (2–6 weeks)
Chancre (painless ulcer) at site of sexual contact and local painless lymphadenopathy
Secondary (6–10 weeks)
Rashes, particularly affecting the trunk, palms and soles of feet
Erosions that occur in linear streaks in the mouth known as “snail track” ulcers
Systemic signs of infections (fatigue, lethargy, pyrexia)
Condylomata lata (non-tender lesions resembling verrucas on the genitalia)
Tertiary (3–15 years)
CNS involvement – dorsal column syndrome (loss of proprioception and vibration)
Argyll Robertson pupil – this is a pupil which can accommodate but not constrict
Aortic aneurysms
Gummas (granuloma lesions of skin))
Key tests
Direct test for syphilis is PCR or dark-field microscopy
Serological tests for syphilis include treponemal antibody tests – this test remains positive after treatment, so it cannot differentiate between current and past infection
Non-specific tests include venereal disease research laboratory (VDLR) – this has high sensitivity in secondary syphilis and levels decline after treatment
Management
1st line IM benzathine penicillin – 2nd line is doxycycline
Jarisch-Herxheimer reaction
Genital Herpes
This is an ulcerating condition which is caused by the herpes simplex virus.
It is usually caused by HSV-2 but can also be caused by HSV-1.
Onset of symptoms occurs around 4 days after exposure. This leads to a primary infection which can be severe and then further outbreaks, which are usually milder.

Symptoms
Males – multiple blisters that form ulcers on glans, shaft of penis, thighs or anus
Females – multiple blisters that form ulcers on vulva, buttocks, clitoris or anus
Fever and headache with general malaise
Key tests
Nucleic acid amplification testing of swab
Management
Antiviral therapy, e.g., oral acyclovir
If pregnant > 28 weeks’ gestation, consider elective caesarean section
Lymphogranuloma Venereum (LGV)
This is an invasion of the inguinal lymph system, causing granulomatous inflammation.
It is a complication of the STI Chlamydia trachomatis.
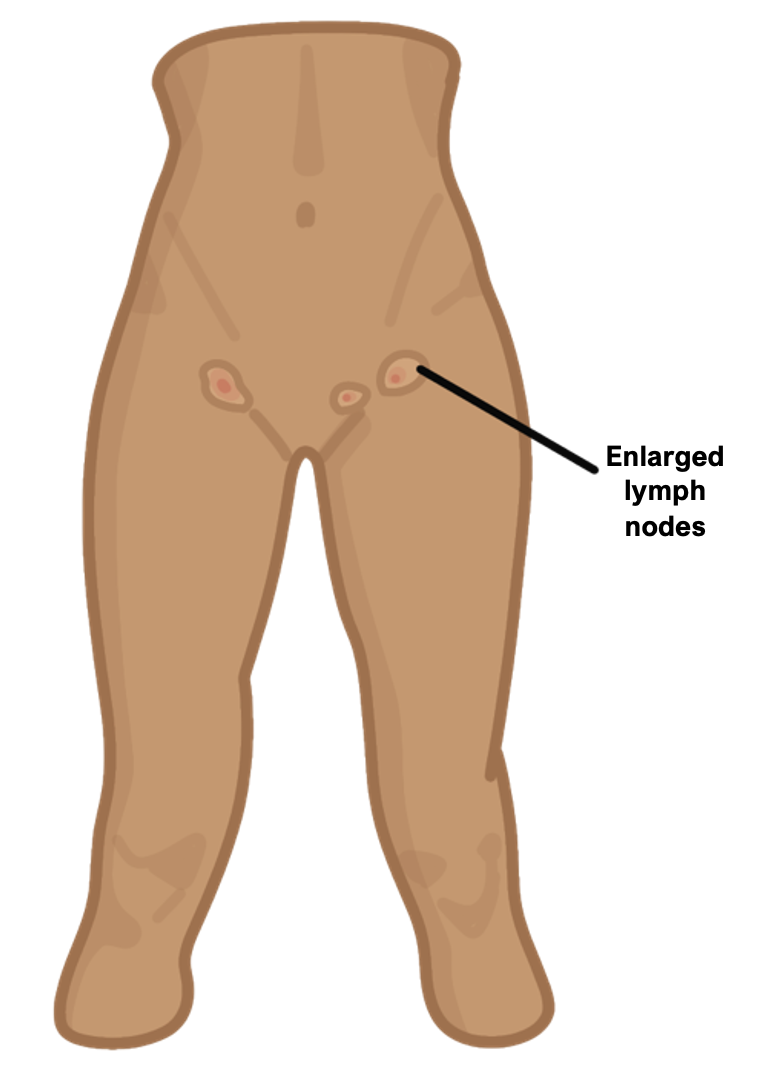
It leads to ulceration and a tender inguinal canal with swollen inguinal lymph nodes.
It heals with fibrosis but can involve perianal structures causing rectal strictures.
Symptoms
Primary stage
Painless genital ulcer at contact site 3–12 days after infection, healing in a few days
Secondary stage
Bilateral or unilateral swollen, painful inguinal lymph nodes 10–30 days later
If route was anal, can develop proctitis symptoms (anal pain, tenesmus, diarrhoea and abdominal cramps
Key tests
Serological testing
Management
Antibiotic treatment for chlamydia, e.g., doxycycline
Chancroid
This is an STD which is caused by the bacteria Haemophilus ducreyi.
It is rare in UK, but a very common cause of genital ulceration in the world.
It causes local symptoms and there are usually no systemic signs.

Symptoms
Painful ulcers with sharply defined irregular saucer-shaped borders
Painful unilateral inguinal lymphadenopathy
In females can cause dysuria and dyspareunia
Management
1st line is macrolide antibiotics (Azithromycin, erythromycin)
Conditions affecting women
Bacterial Vaginosis
This condition is due to an overgrowth of bacteria in the vaginal canal.
The vagina is normally dominated by Lactobacillus, but overgrowth of the anaerobic bacteria Gardnerella vaginalis creates a biofilm.
This allows other opportunistic bacteria to thrive. Colonisation of anaerobic bacteria means aerobic Lactobacilli stop making lactic acid, raising the pH of the discharge.
Symptoms
It is asymptomatic in about half of women and usually not painful
“Fishy” odour which smells bad and is white or grey in colour
Diagnosis
This is done using a vaginal swab. Looking for at least 3 features:
i) pH > 4.5
ii) Thin, white discharge
iii) Clue cells seen on microscopy
iv) Positive whiff test –> this is when adding potassium hydroxide gives a fishy odour
Management
1st line is oral metronidazole for 5-7 days
Trichomonas Vaginalis
This is a protozoan parasite which causes the STI trichomoniasis, spread via skin-to-skin contact.
Symptoms
Offensive smelling vaginal discharge which is yellow/green in colour
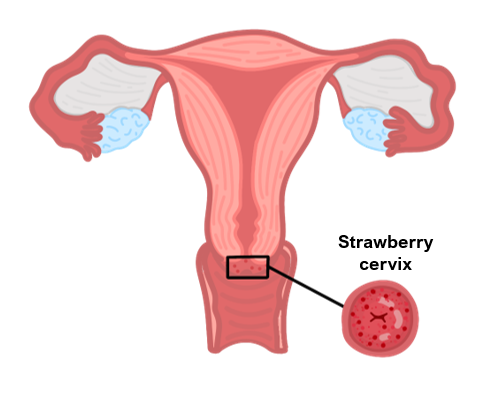
Vulvovaginitis (itching, burning, pain) with a strawberry cervix
It is usually asymptomatic in men, but can cause urethritis
Key tests
Vaginal smear and wet mount microscopy shows the trophozoites
pH of vaginal discharge > 4.5
Management
1st line is oral metronidazole for 5-7 days
Candidiasis
This is called vaginal thrush and it is usually self-diagnosed and managed.
It is due to growth of the yeast Candida which colonises the vagina causing irritation.
It is not entirely regarded as an STI as there is no infectious risk to the partner.
It is associated with increased age, immunosuppression, pregnancy and diabetes.
Risk factors
Age
Immunosuppression
Pregnancy
Diabetes

Symptoms
Itchy vagina with dyspareunia (painful intercourse)
“Cottage-cheese” discharge which does not smell offensive
Symptoms can worsen just before a woman’s period
Key tests
Usually diagnosed clinically, but if doubt take vaginal swab
Management
If moderate, intravaginal antifungal (e.g., clotrimazole 500 mg pessary)
If more severe, oral fluconazole 150 mg single dose can be give

