Introduction
Bacteria are prokaryotic (single-celled) microorganisms that are found in both human health and disease.
Bacteria range in size from approximately 0.5-5.0 micrometers in length and different in morphology. Typical shapes of bacteria include spheres (i.e. cocci) and rods (i.e. bacilli) .
The human body is colonised with trillions of bacteria in normal health. This collective is known as the human microbiota and is important for normal functioning. Bacteria are also the cause of many clinically relevant infections in humans.
Cell wall structure
The general structure of a bacterium includes the cell wall, cell membrane, capsule, flagella, fimbriae, nuclear material, cytoplasm and other intracellular components.
The cell wall forms the outer aspect of bacteria, which protects it against host immune defences and external osmotic pressures. The cell wall differs depending on whether the organisms is gram-positive or gram-negative. These are the two major groups of bacteria.
- Gram-positive organisms: have a thick peptidoglycan layer composed of polysaccharides and charged amino acids interlaced with other major polymers like teichoic acid. Underneath the peptidoglycan layers is the cell membrane
- Gram-negative organisms: have an outer cell membrane that contains lipopolysaccharides(LPS). Beneath the outer membrane is a smaller peptidoglycan layer compared to gram positive organisms and then the cell membrane. LPS is the key feature of gram negative organisms that contains lipid A. When broken down and released into the circulation, lipid A stimulates a profound inflammatory response that can lead to septic shock.
NOTE: Some bacteria do not have a cell wall (e.g. mycoplasma).
Gram stain
Gram staining is a technique used to identify microorganisms under a microscope.
Gram staining follows a number of steps:
- Application of primary stain: Crystal violet staining cells blue/purple
- Application of mordant: Gram’s iodine solution is added, forms a complex with crystal violet
- Decolourisation: Agent such as acetone added, thinner peptidoglycan layer of gram-negative bacteria cannot retain the crystal violet-iodine complex
- Application of counterstain: Such as safranin, stains decolourised cells red.
In gram-positive bacteria, the thick peptidoglycan layer results in retention of the violet crystal. In gram-negative bacteria, the thin peptidoglycan layer results in loss of the crystal allowing its cell wall to be counterstained red.
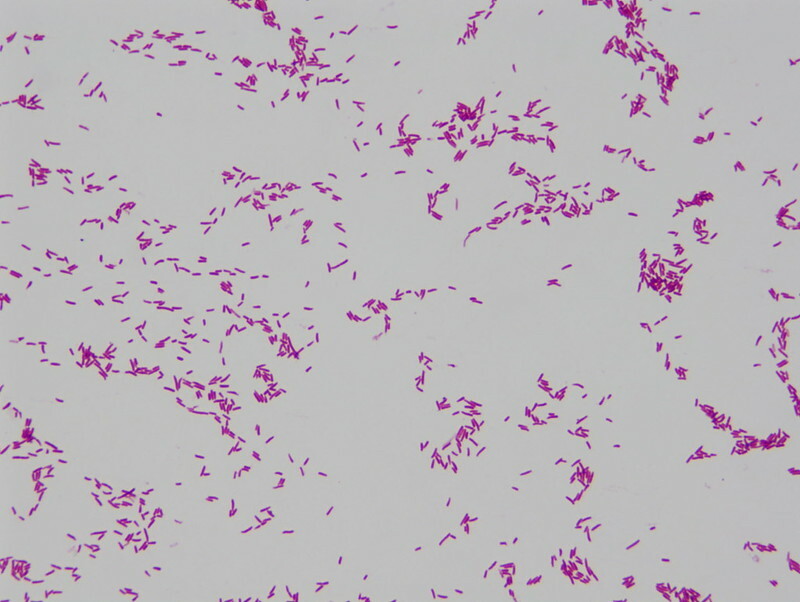
Gram-negative rods – a culture of E.coli
Image courtesy of Joe Rubin
Classification
Bacteria can be broadly divided into two main groups (gram-positive or gram-negative) based on gram staining of the bacterial cell well.
Gram-negative bacteria are further divided based on the morphology, which can be assessed under the microscope. The three major groups are cocci (spheres), bacilli (rods) and coccibacilli (intermediate shape).
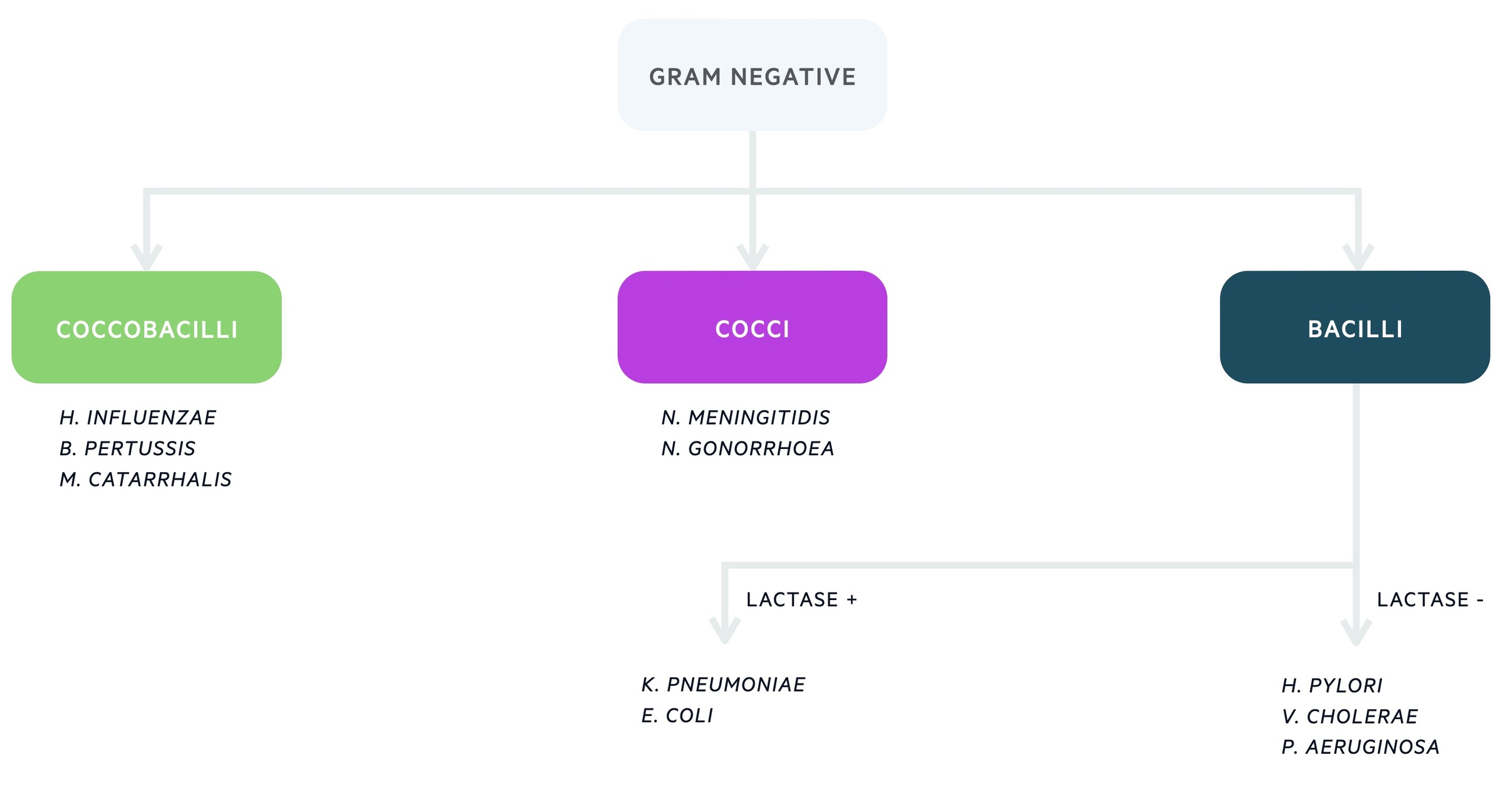
Further differentiation is then based on laboratory and molecular techniques that assess the different characteristics of gram negative bacteria.
NOTE: Coliform is a generic term that refers to fermentative rod-shaped gram-negative microorganisms (e.g. E. coli and K. Pneumoniae)
ESBLs
Some bacteria produce the enzyme beta-lactamase that breaks down beta-lactam antibiotics (i.e. penicillin, cephalosporins) making them resistant.
Bacteria that have beta-lactamases with an extended-spectrum to a wide-range of beta-lactam antibiotics are known as extended-spectrum beta-lactamases.
These are a significant medical problem because only limited antibiotics can be used to treat ESBL infections. Two common microorganisms with ESBL activity are E. coli and K. pneumoniae.
Escherichia
Escherichia are commonly associated with urinary and gastrointestinal infections and are a major cause of nosocomial infections (hospital-acquired).
Types
Most members of Escherichia are common commensals in the gut microflora. Some strains, notably Escherichia coli, are pathogenic to humans causing numerous infections. Different serotypes of Escherichia coli are shown below.
- Enterotoxigenic Escherichia coli (ETEC) – Gastroenteritis
- Enteropathogenic Escherichia coli (EPEC) – Gastroenteritis
- Uropathogenic Escherichia coli – UTIs
- Enterohemorrhagic Escherichia coli (EHEC) – Haemolytic uraemic syndrome
- Shiga toxin–producing Escherichia coli (STEC) – Shigella-like dysentery
Shape
Escherichia are rod-shaped (bacilli), facultative anaerobic microorganisms. They are referred to as coliforms.
Locations
Commonly found in the lower intestines.
Infections
E. Coli usually causes intra-abdominal and urinary infections.
- UTI
- Biliary infections
- Gastroenteritis
- Hospital-acquired pneumonia
E. Coli 0157 is a specific serotype of Escherichia that can cause haemolytic uraemic syndrome (HUS). HUS is a clinical syndrome that can occur following a diarrhoeal illness with the 0157 serotype. It presents with acute kidney injury, haemolytic anaemia and thrombocytopenia.
HUS is one of the microangiopathic haemolytic anaemias (non-immune mediated destruction of erythrocytes) that occurs due to damage and dysfunction of the endothelial lining of blood vessels.
Treatment
Numerous antibiotics can be used to treat E. coli. However, due to increasing resistance patterns and the emergence of ESBLs, many require the use of intravenous broad-spectrum antibiotics.
Klebsiella
Klebsiella are a major cause of nosocomial infections, particularly affecting the biliary system, urinary system and lower respiratory tract.
Types
There are three major Klebsiella species that cause infections in humans.
- Klebsiella pneumoniae
- Klebsiella oxytoca
- Klebsiella granulomatis
Shape
Klebsiella are rod-shaped (bacilli) microorganisms that contain a prominent polysaccharide capsule.
Locations
May be found colonising skin, the gastrointestinal tract and pharynx. In some parts of the gastrointestinal tract considered part of the normal flora.
Infections
Klebsiella commonly affect the respiratory tract, urinary and biliary systems.
- UTI
- Biliary infections
- Pneumonia
Hospital-acquired pneumonia secondary to Klebsiella pneumoniae usually cause a subacute presentation.
Treatment
Klebsiella are resistant to numerous antibiotics and treating them is becoming more difficult especially with ESBLs. Typical antibiotics choices include cephalosporins, aminoglycosides and quinolones.
Pseudomonas
Pseudomonas is an opportunistic pathogen, typically causing infections in patients with impaired immune systems.
Whilst rarely causing disease in healthy individuals, pseudomonas is a significant problem in patients with chronic lung disease (e.g. cystic fibrosis) or compromised immune systems.
Pseudomonas contains multiple host resistance genes and forms a thick biofilm that protects the microorganism from host defences and anti-microbials.
Types
The major human Pseudomonal pathogen is Pseudomonas aeruginosa.
Shape
Pseudomonas is a gram-negative rod-shaped (Bacilli) that predominantly uses aerobic respiration.
Infections
Pseudomonas can infect almost every site within the body, but it is most prominently a problem in wounds, urinary and respiratory tract.
- Wounds (e.g. Burns)
- UTIs
- Pneumonia
- Meningitis
- Osteomyelitis
Treatment
Pseudomonas has a high rate of antibiotic resistance making treatment difficult. Typical treatment regimes include beta-lactam based antibiotics with pseudomonal cover (e.g. Tazocin) and aminoglycosides.
Other
There are several other clinically relevant gram-negative microorganisms.
Neisseria
The two major Neisseria pathogens are Neisseria gonorrhoea and Neisseria meningitidis. These cause the infections gonorrhoea and meningitis, respectively. Both these microorganisms are gram-negative diplococci.
Haemophilus
The major human pathogen is Haemophilus influenza. It is an encapsulated gram-negative cocco-bacilli that causes pneumonia, especially in patients with chronic lung disease (i.e COPD).
Salmonella
Salmonella can cause serious gastrointestinal infections. Salmonella typhi is the cause of typhoid and Salmonella enterica is the cause of paratyphoid. Salmonella typhi can be vaccinated against, usually as a combination vaccine with hepatitis A.
Campylobacter
Campylobacter is one of the most common causes of food poisoning within the UK, often from contamination of raw chicken. In rare cases, autoimmune reactions can occur following infections with campylobacter jejuni such as Guillain-Barré syndrome (immune-mediated demyelinating polyneuropathy of peripheral nervous system).

