Lyme disease
This is a condition which is caused by the bacteria Borrelia burgdorferi.
Transmission occurs via the Ixodes tick bite, so it is important to ask a detailed travel history to places where these ticks live e.g., forests, parks (e.g., Richmond Park in London has a higher incidence).
It initially causes an expanding area of redness on the skin at the site of the tick bite.
The bacteria can become systemic and spread to the heart, joints and CNS where they can persist for years.
It is thought that the bacteria induce an autoimmune disease secondary to molecular mimicry, which leads to the development of symptoms.
Symptoms
Initially fever, arthralgia, malaise
Starts with erythema migrans (rash at bite site, appears as a ring of erythema with a central clearing)
The disease can lead to several complications
Complications
Cardiovascular – heart block, acute myocarditis
CNS – can develop after a long time: meningitis, Bell’s palsy and neuropathy
Polyarthritis – lasts even after the bacteria have been eradicated

Key tests
The disease can be diagnosed clinically if erythema migrans is present
1st line is ELISA for antibodies – if positive, do immunoblot test for Lyme disease
Management
Patients should start treatment before the ELISA results come through if there is high clinical suspicion of the disease
In early disease, doxycycline is recommended
In later disease, other antibiotics such as ceftriaxone can be used
Leptospirosis
This is an infection due to the bacteria Leptospira which cause a systemic infection.
Transmission is via contaminated rat urine infected through breaches in the skin/ mucous membranes.
As it is spread in rat urine, it is seen in sewage workers and farmers in particular.
The bacteria spread to various organs, especially the liver, damaging hepatocytes.
Upregulated inflammation can also lead to an interstitial nephritis giving an AKI.
The most severe form of the disease is known as Weil’s disease, and typically causes jaundice due to hepatocyte damage.
Risk factors
Sewage workers and farmers particularly
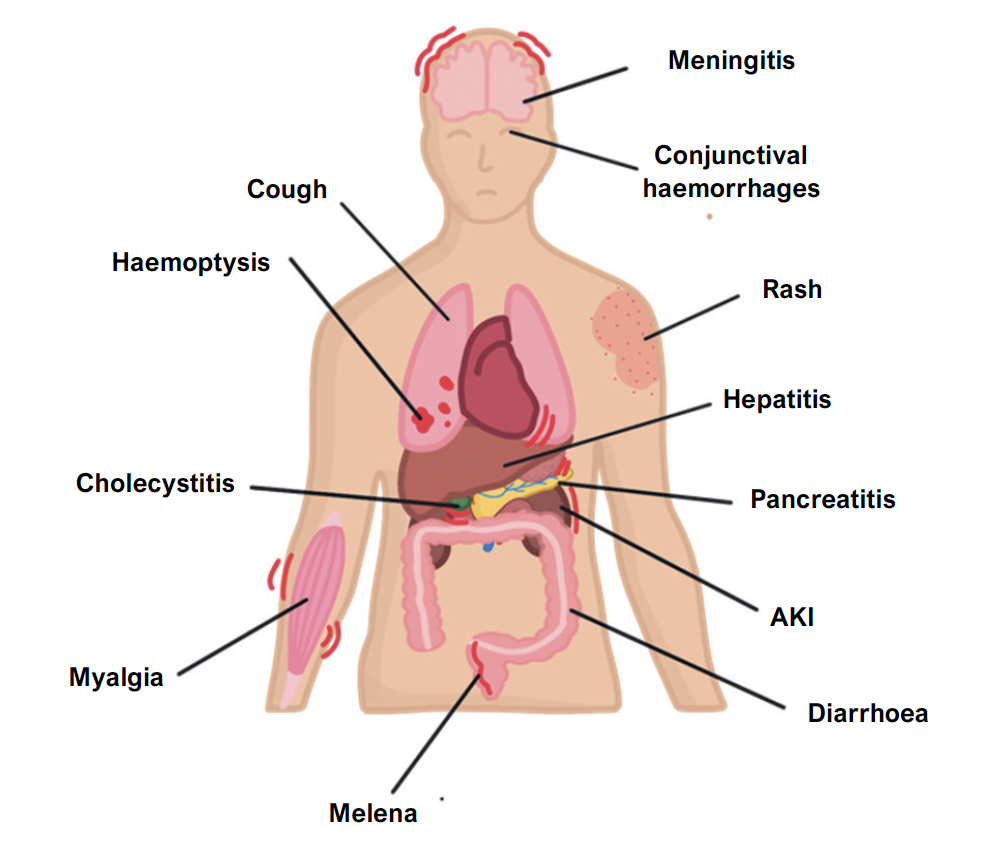
Symptoms
Fever and flu like symptoms
Jaundice and elevated LFTs, due to liver involvement
Kidney – AKI, low urine output
Bleeding from lungs, gut and mucous membranes (due to depletion of platelets)
Subconjunctival haemorrhages
Key tests
Serological testing for IgM to bacteria is diagnostic
Bloods show raised inflammatory markers
Management
Antibiotics to clear bacteria, e.g., doxycycline/benzylpenicillin
Toxic shock syndrome
This is a condition which is due to an inflammatory reaction to bacterial toxins.
It is caused by S. Aureus or S. pyogenes usually which produce the TSS toxin – 1.
This acts as a superantigen meaning it can stimulate T cells directly and does not need initial processing by an antigen-presenting cell.
T cells are activated giving a cytokine storm and unregulated inflammation.
Risk factors
Tampon use
Skin lesions in young children
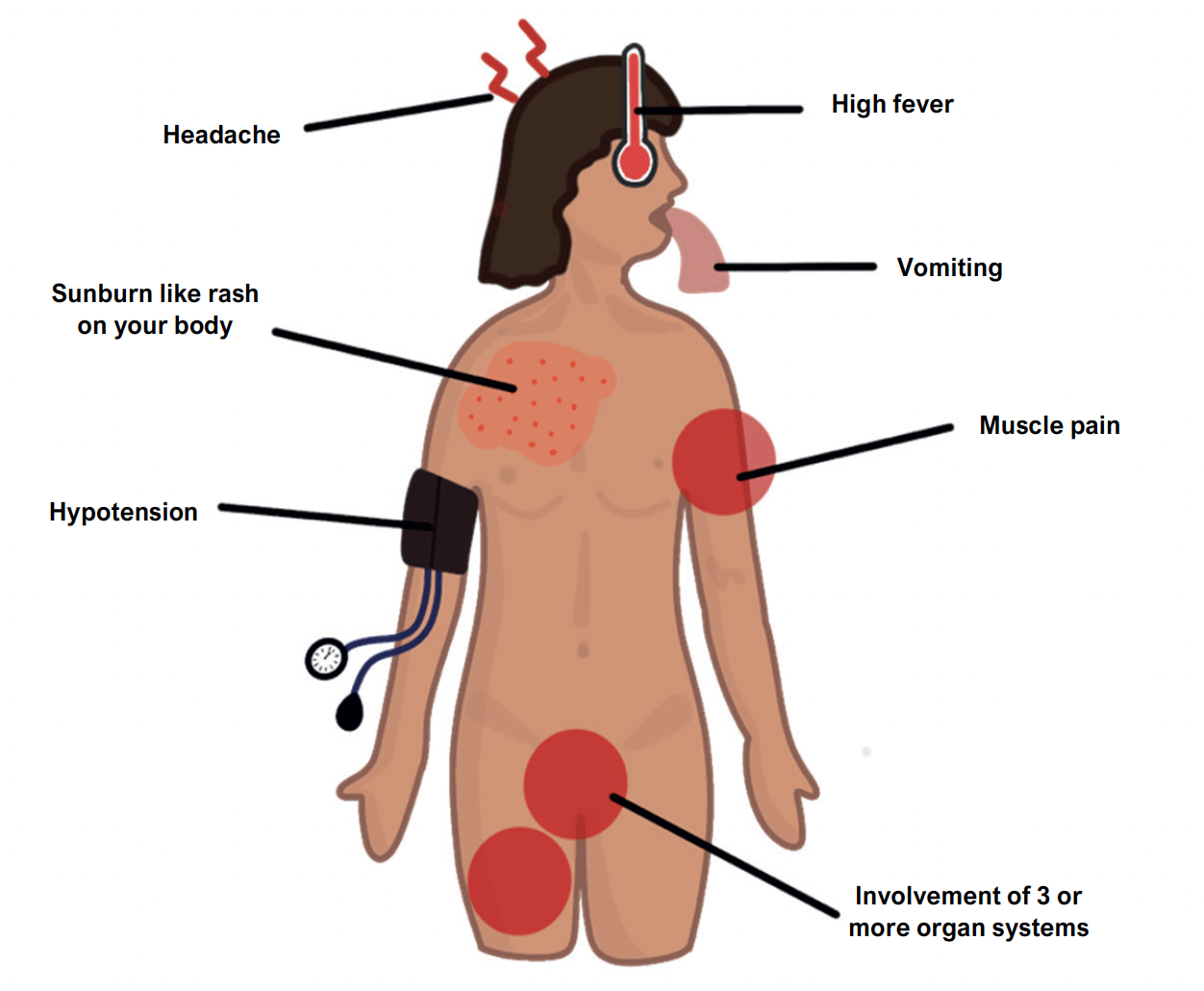
Symptoms
Fever – temperature > 38.9ÅãC
Hypotension – systolic BP < 90 mmHg leading to confusion and lethargy
Headache, watery diarrhoea, non-purulent conjunctivitis
Diffuse red rash, typically like a ‘sunburn’
Desquamation of the rash occurs after 10 days (affecting soles, palms, and lips)
Involvement of 3 or more organ systems e.g., GI (vomiting/diarrhoea at start of disease), kidney (raised creatinine, indicating AKI), liver (abnormal liver function tests)
Management
Will usually require admission to ITU and IV antibiotics
Important to urgently remove/drain source of infection (e.g., remove tampon)

