Overview
Non-alcoholic fatty liver disease (NAFLD) essentially refers to the presence of excess fat in the liver in the absence of excess alcohol consumption.
Non-alcoholic fatty liver disease (NAFLD) is a rising problem worldwide. It is defined as excess fat with the liver, which is known as hepatic steatosis (i.e. fatty liver). A small amount of fat in the liver is normal, but when this is present in > 5% of hepatocytes we term it NAFLD. NALFD is strongly linked to obesity and the metabolic syndrome.
NAFLD is a condition that actually encompasses a spectrum of pathological conditions including:
- Non-alcoholic fatty liver (NAFL): sometimes referred to as simple steatosis
- Non-alcoholic steatohepatitis (NASH): describes the presence of liver inflammation and injury
- Liver fibrosis: refers to liver scarring
- Cirrhosis: an advanced form of liver fibrosis that is irreversible and associated with major complications
Patients with NAFLD are at risk of progression to NASH. NASH is a state liver inflammation and injury that is usually confirmed on liver biopsy. NASH increases the risk of progression to fibrosis, cirrhosis (i.e. advanced form of fibrosis), and hepatocellular carcinoma (HCC).
As the name suggests the diagnosis of NAFLD requires exclusion of a significant alcohol intake (≥ 30g/day men and ≥ 20g/day women), which would be suggestive of alcohol-related liver disease that can also cause a fatty liver. Approximately, 8 g of ethanal is equivalent to 1 unit of alcohol.
Epidemiology
NAFLD affects around 20% of the population in developed countries.
NAFLD is a growing problem due to the rise in obesity. NAFLD is now the most common cause of abnormal liver blood tests within the UK and estimated to affect > 50% of patients with type 2 diabetes mellitus. NAFLD is more common in older patients and those with obesity or metabolic syndrome. However, it can occur in children and lean (i.e. normal weight) individuals.
NAFLD is expected to become the leading indication for liver transplantation.
Aetiology & pathophysiology
The exact cause of NAFLD is not fully understood.
It is important to recognise that NAFLD is an extremely complex and heterogenous condition that has been linked to multiple aetiological factors. These all contribute to the pathophysiology of the condition and its progression to cirrhosis and other liver-related complications.
The development of NAFLD is strongly linked to obesity, insulin resistance and the metabolic syndrome. Factors such as a high calorie diet, excess (saturated) fats, high fructose intake and a Western diet all contribute to the development of weight gain, obesity and NAFLD.
Metabolic syndrome
The metabolic syndrome refers to a group of risk factors that are associated with an increased risk of cardiovascular disease and stroke. These risk factors have also been associated with the development NAFLD and include:
- Abdominal obesity: waist circumference > 94 cm men and > 80 cm women
- Hypertension: arterial blood pressure > 130/85 mmHg or treated for hypertension
- Impaired fasting glucose: fasting blood glucose > 5.6 mmol/L or treated for type 2 diabetes mellitus
- High triglycerides: serum level > 1.7 mmol/L
- Low HDL cholesterol: < 1.0 mg/dl mne and < 1.3 mmol/L women
Insulin resistance
Insulin resistance, which occurs when peripheral tissue (e.g. muscle, fat, liver) doesn’t respond as well to insulin, is one of the major drivers in NAFLD due to the secondary effects on lipid metabolism. It promotes increased breakdown of peripheral adipose tissue (i.e. lipolysis), increased synthesis of triglycerides and increased uptake of fatty acids. Collectively, this contributes to the accumulation of toxic lipids within the liver and development of hepatic steatosis.
Genetics
There is a genetic element to the NAFLD with various genetic mutations (i.e. variants) linked to development and progression of NAFLD (e.g. PNPLA3 and TM6SF2). These factors are particularly important in children and lean patients who develop NAFLD.
Natural progression
The accumulation of fat within the liver can promote inflammatory changes, liver injury and eventually scarring leading to fibrosis and in its most severe form cirrhosis. It is estimated that 20% of patients with NAFLD will progress to NASH and approximately one fifth of patients with NASH will process to cirrhosis, end-stage liver disease and hepatocellular carcinoma.
This means that only a relatively small proportion of patients with NAFLD (compared to the total number of patients) will progress to more severe forms of liver disease. This makes it really important to try and identify patients who are at risk of progression, rather than screening the whole population that is unlikely to be cost-effective.
Clinical features
Patients with NAFLD are usually asymptomatic.
Patients with NAFLD are usually asymptomatic but they may have non-specific right upper quadrant pain due to hepatomegaly. It is important to assess for features of chronic liver disease that may indicate underlying cirrhosis.
Symptoms
- Asymptomatic
- Fatigue
- Right upper quadrant pain
Signs
- Hepatomegaly
- Obesity (high BMI >30 kg/m2)
- High blood pressure
- Features of chronic liver disease: spider naevi, palmar erythema, leuconychia, hepatosplenomegaly
- Features of decompensated cirrhosis (i.e. advanced liver disease): jaundice, ascites, bruising, encephalopathy
For more information on features of liver disease see our Chronic liver disease note.
Diagnosis & investigations
The diagnosis of NAFLD is based on the finding of hepatic steatosis and exclusion of other causes of fatty liver (e.g. alcohol).
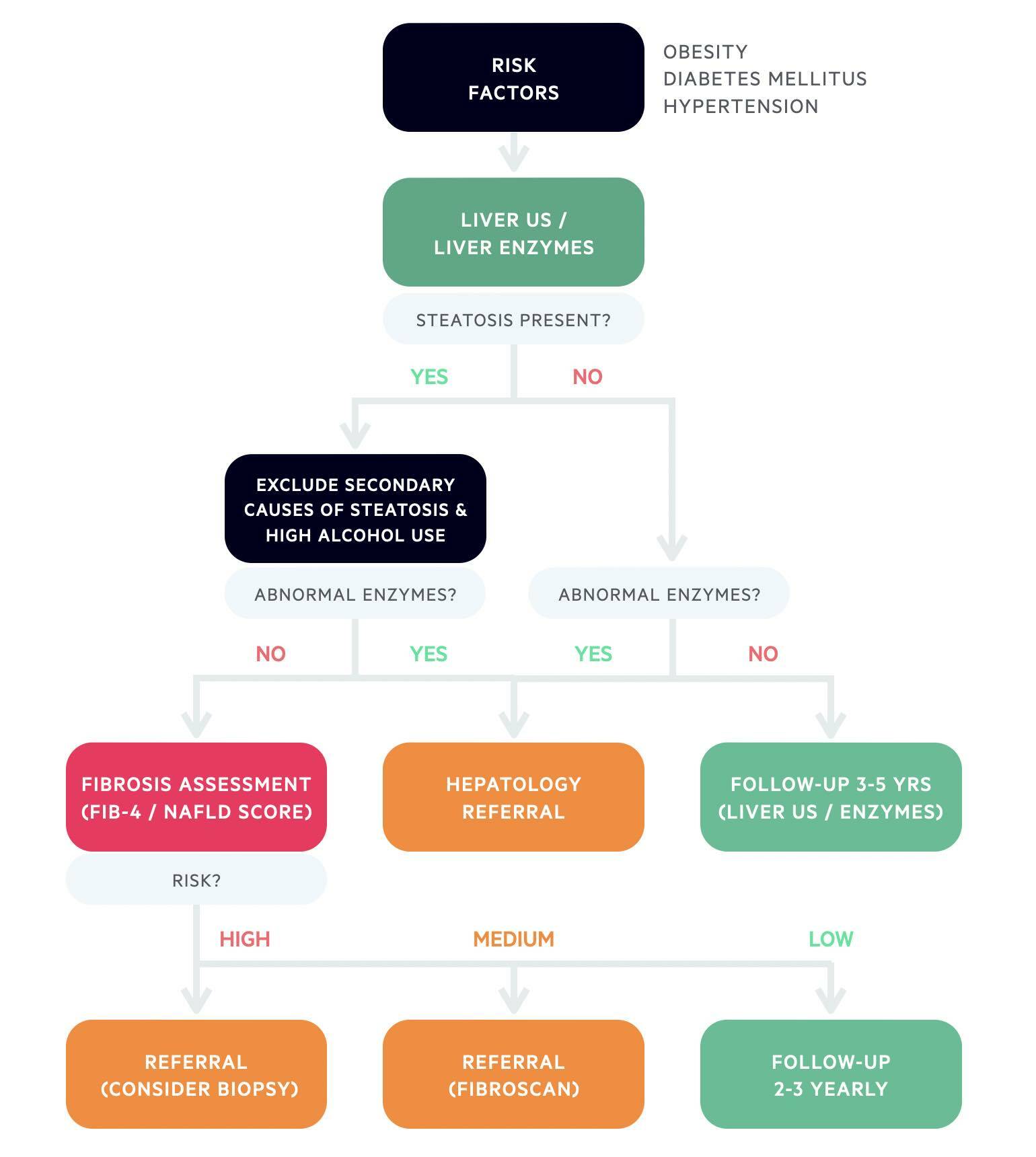
In patients with suspected NAFLD a liver ultrasound and routine blood tests form the basic first line diagnostic tests. These may be requested in patients at risk of NAFLD (e.g. obesity, metabolic syndrome risk factors). Other times, NAFLD may be suspected based on abnormal liver function tests in the context of metabolic risk factors or the incidental finding of hepatic steatosis on imaging.
A liver ultrasound can confirm the presence of a fatty liver and blood tests can help exclude deranged liver function tests (e.g. abnormal ALT/AST). Deranged liver function tests are suggestive of liver inflammation consistent with NASH or another underlying liver pathology. Importantly, routine liver function tests do not exclude NASH (e.g. they may be normal), which is why risk scores have been developed to exclude fibrosis (discussed further below).
Further work-up
As part of the NAFLD work-up patients require a comprehensive assessment to exclude other causes of fatty liver such as alcohol, assess for other metabolic syndrome risk factors, and consider a full non-invasive liver screen. The full screen is to look for other potential caues of liver disease in patienst with abnormal liver function tests.
Other causes of fatty liver include:
- Alcohol
- Drug-induced
- Hepatitis C
- Haemochromatosis
- Autoimmune hepatitis
- Coeliac disease
- Inborn errors of metabolism
- Parenteral nutrition
- Starvation
A comprehensive assessment would include:
- Exclude significant alcohol intake: arbitrarily defined as ≥30g/day in men and ≥20 g in women (8g ethanol = 1 unit). Important because alcohol-related liver disease can also cause a fatty liver
- Assess cardiovascular risk: personal and family history of diabetes, hypertension, ischaemic heart disease
- Patient demographics: BMI, waist circumference, change in body weight
- Hepatic B/C serology
- Any history of drugs causing steatosis
- HbA1c +/- fasting glucose
- Full blood count
- Lipid profile: LDL, HDL, triglycerides, total cholesterol
- Liver ultrasound: if not already completed showing fatty liver
Further tests for coeliac, hypothyroidism and a full non-invasive liver screen (e.g. autoantibodies, careuloplasmin) depends on liver function test results and clinical evaluation.
Hepatology referral
If patients have markedly deranged liver function tests or clinical features of chronic liver disease then it is usually more appropriate to make an urgent referral to hepatology who can undertake these further assessments.
Fibrosis risk assessment
Once NAFLD has been established it is important to determine a patients risk of advanced fibrosis. The only true way to diagnosis NASH is through liver biopsy. However, this is an invasive investigation associated with complications. Therefore, a number of non-invasive markers or risk scores have been established.
There are various pathways recommended that differ slightly depending on the available resources, choice of non-invasive test and access to hepatology.
ELF pathway
The Enhanced Liver Fibrosis (ELF) blood test measures three molecules involved in liver matrix metabolism to give a score reflecting the severity of liver fibrosis. Patients with a score > 10.5 should be referred to hepatology for further assessment of possible advanced fibrosis (may include biopsy). If negative, it can be repeated every 2-3 years.
Non-ELF pathway
Two major risk scores can be used known as the FIB-4 and NAFLD fibrosis score. These scores are based on patient demographic and biochemical data. In those with low scores, advanced fibrosis is effectively ruled out. These non-invasive tests can be repeated every 2-3 years.
If the scores are high, advanced fibrosis cannot be ruled out. In this situation, patients are usually referred for a second line test such as transient elastrography, which is a non-invasive measure of liver stiffness also known as a Fibroscan. Patients who have a very high FIB-4 score may be directly organised for a biopsy by the hepatology team.
Management
Treatment of NAFLD centres on dietary advice, exercise and managing co-morbidities (e.g. diabetes).
The principal treatment for NAFLD is weight loss based on dietary advice and exercise. Lifestyle correction is mandatory in all patients and usually centres around a target of 7-10% weight loss (minimum).
Patients should be given advise to reduce calorie intake by 500-1000 kcal/day to achieve 0.5-1 kg weight loss per week. This should be combined with 150-200 minutes of moderate intensity aerobic exercise per week over 3-5 sessions. Both aerobic and resistance training exercises have been shown to reduce liver fat. Patients should also be advised to reduce alcohol intake and if advanced fibrosis, complete abstinence.
Patients who are unable to loss weight by themselves may need to enter structured weight loss programmes.
Managing co-morbidities
Patients with NAFLD often have other features of the metabolic syndrome including high blood pressure, diabetes and high cholesterol. It is important that these are investigated and treated appropriately.
Pharmacological therapies
There are no licensed pharmacological therapies that are currently available for patients with NAFLD. In clinical trials, there has been some success with the oral hypoglycaemic agent pioglitazone and vitamin E supplementation. The use of these medications should be guided by specialists and may form part of a clinical trial. Newer medications are currently in early clinical trials and there is an emerging role for glucagon-like-peptide 1 analogues and sodium-glucose transport protein 2 inhibitors that are both used in type 2 diabetes mellitus.
Bariatric surgery
Patients who are unable to loss weight despite dietary and exercise advice may be considered for bariatric surgery. There are various methods that are currently available (e.g. sleeve gastrectomy, Roux-en-Y gastric bypass). Patients who may be suitable should be referred to a bariatric centre.
Liver transplantation
Patients with progressive NASH may develop cirrhosis and liver-related complications. Liver transplantation is the only curative treatment for end-stage liver disease and may be an option in patients with advanced liver disease (e.g. decompensated cirrhosis) secondary to NASH. Patients with cirrhosis should also undergo surveillance programmes for hepatocellular carcinoma and oesophageal varices.
For more information see our Chronic liver disease note.
Complications
Patients with advanced liver disease secondary to NAFLD are at risk of multiple complications.
Patients with NALFD are usually overweight with multiple cardiovascular risk factors. They are at risk of both liver-related and non-liver-related complications. Only a small subset of patients with NAFLD will develop advanced liver disease and need for transplantation.
Liver-related complications
- Decompensated cirrhosis
- Hepatocellular carcinoma
- Sepsis
Non-liver complications
Cardiovascular disease is the most common cause of death in patients with NAFLD. These patients are at higher risk of hypertension, type 2 diabetes mellitus, chronic kidney disease and heart disease.

