Macrocytic Anaemia
This is an anaemia with MCV > 100um3, most commonly due to folate or Vitamin B12 deficiency.
– These are needed to make DNA which is needed for cell division.
Causes of macrocytic anaemia can be remembered by the acronym FAT RBC MC:
Foetus
Alcohol excess
Thyroid (hypothyroid)
Reticulocytosis (due to haemolytic anaemia as RBC precursors are bigger)
B12/folate deficiency
Cirrhosis (liver)
Myeloproliferative disorders –> precursors are bigger than RBC so increase average volume
Cytotoxic drugs (e.g. 5-fluorouracil)
Folate deficiency
This is found in green leafy vegetables, nuts and liver and is absorbed in the jejunum.
– The deficiency leads to an inability to synthesise enough DNA which leads to megaloblastic anaemia.
Causes:
– Supply –> poor diet seen in elderly + alcoholics
– Increased demand –> pregnancy + cancer
– Malabsorption –> coeliac disease giving small bowel inflammation
– Antifolate drugs –> Methotrexate + Sulfonamide antibiotics
Symptoms:
– Anaemia symptoms –> fatigue, weakness, light headedness etc.
– Glossitis + Angular cheilosis (not koilonychia)
Tests:
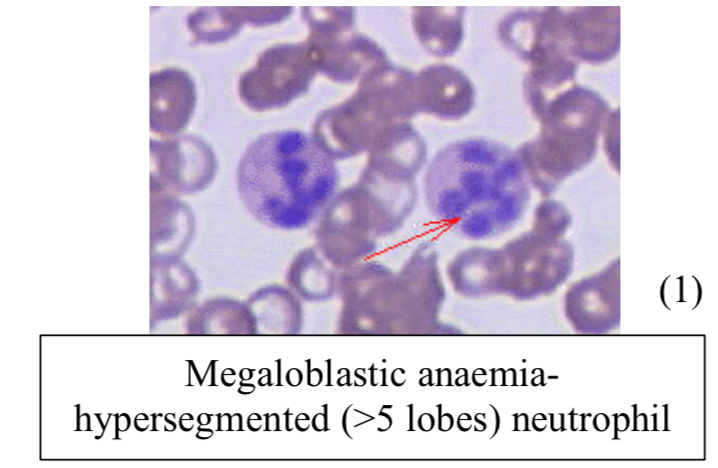
– Blood film –> shows hypersegmented neutrophils (>5 lobes)
– Low folate + High homocysteine (as it is not converted to methionine) + Low methylmalonic acid
– Check serum B12 –> Then do bone marrow biopsy if cause is not revealed by above tests
Management:
1st exclude Vitamin B12 deficiency. Then give folate replacement
Vitamin B12 deficiency
This is common, occurring usually in elderly people – but less common than folate deficiency.
– It takes years to develop unlike folate deficiency due to large hepatic stores of Vitamin B12
Causes:
– Supply –> Vegans do not consume Vitamin B12 as it is only found in animal products
– Malabsorption –> Crohn’s disease and tapeworms affect terminal ileum where it is absorbed
– Pernicious anaemia (most common) –> autoimmune destruction of parietal cells in stomach which produce intrinsic factor
Symptoms:
– Anaemia symptoms –> fatigue, weakness, light headedness + Glossitis + Angular cheilosis
– Lemon tinge to skin due to pallor and mild jaundice (haemolysis)
Tests:
Same as folate deficiency, except there is raised methylmalonic acid
Management:
– B12 3 times/week for 2 weeks, then once/3months by IM injection
– If also folic acid deficient, treat Vitamin B12 first to avoid precipitating spinal cord degeneration.
N.B. In addition to anaemia, Vitamin B12 acts as a cofactor to turn methylmalonic acid to succinyl CoA.
In deficiency, methylmalonic acid builds up demyelinating the spinal cord giving neurological symptoms.


