Overview
The Hepatitis A virus is a non-enveloped single-stranded RNA virus.
Spread via the faeco-oral route, hepatitis A belongs to the Hepatovirus genus of the Picornaviridae family. Hand washing and good hand hygiene are key to reducing transmission.
It causes a viral hepatitis, and is frequently seen in travellers to endemic areas and those engaging in higher-risk sexual activities.
The majority of adults infected experience symptoms (approx 70-95%). Commonly a mild self-limiting illness manifesting with flu like symptoms, abdominal discomfort and nausea. Children under the age of 5 are frequently asymptomatic.
Hepatitis A under a electron microscope
Image courtesy of Wikipedia Commons
Risk factors
Though uncommon in the UK, there are a number of at risk groups.
- Travel: those travelling to endemic areas
- Sexual: high risk activities (e.g analingus, digital-rectal contact, chemsex), multiple partners
- Haematological disorders: factor VIII and factor IX concentrates have been implicated in transmission
- Occupational risks: for example laboratory or sewage workers
- IVDU: known to be at increased risk.
Phases
Hepatitis A is said to follow four clinical phases (though significant variation exists).
- Incubation: Hepatitis A as a relatively long incubation period that may last from 2 – 6 weeks (mean 28-30 days).
- Prodromal: Early part of the disease, characterised by fever, joint pain and rash. Flu-like symptoms may be present
- Icteric: In addition to jaundice, the icteric phase is characterised by anorexia, abdominal pain and change in bowel habit.
- Convalescent: Recovery phase as the body returns to normal and symptoms subside. Symptoms like malaise may last months.
Clinical features
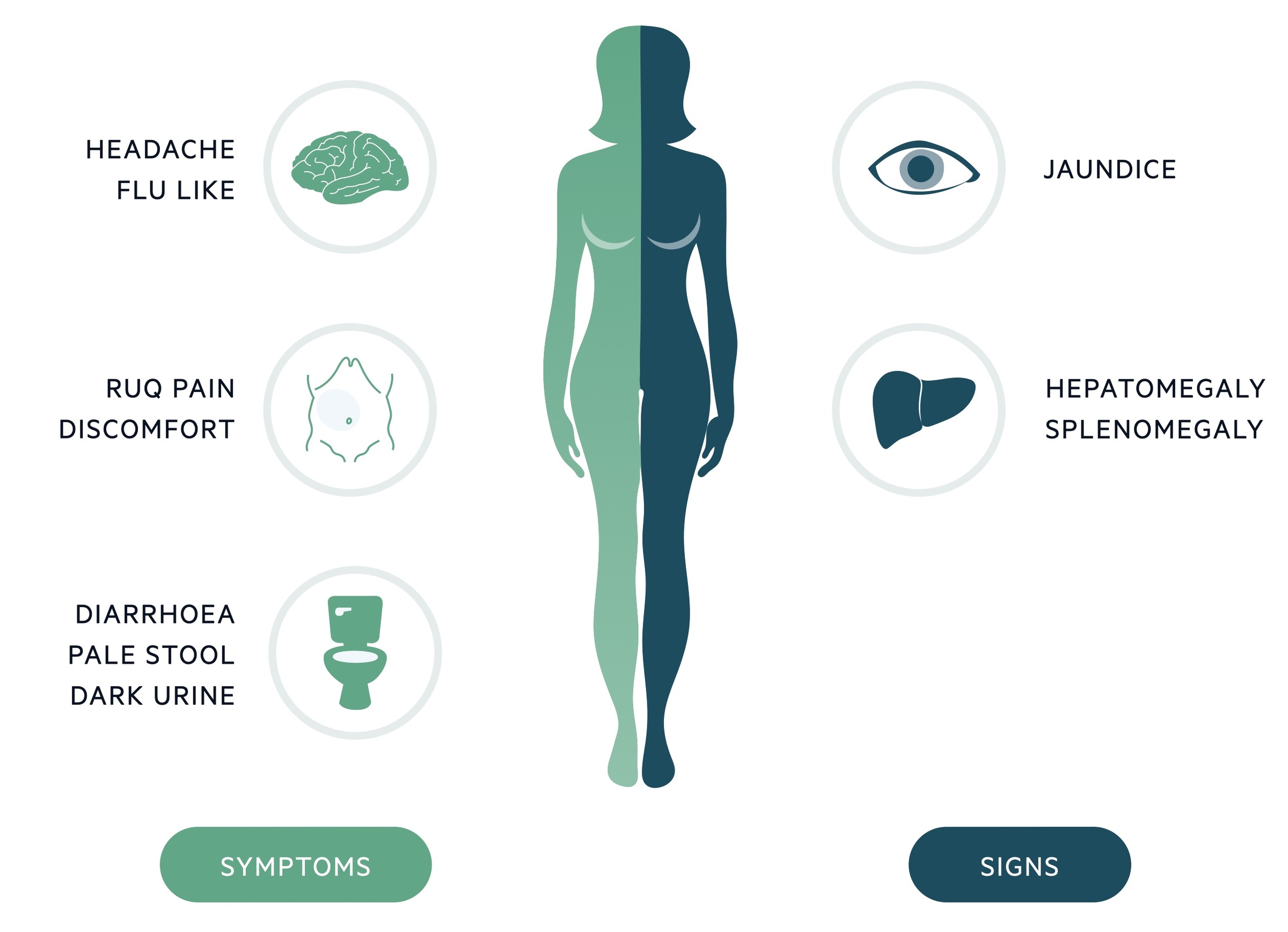
Hepatitis A tends to cause a mild illness characterised by a flu-like illness and GI upset.
Symptoms
- Abdominal discomfort
- Nausea
- Anorexia
- Diarrhoea
- Flu-like illness
- Pruritus
- Dark urine, pale stool
- Rash
Signs
- Jaundice
- RUQ tenderness
- Hepatomegaly (85%)
- Splenomegaly (15%)
- Lymphadenopathy (5%)
NOTE: One unusual symptom seen in smokers is a sudden distaste for cigarettes.
Investigations
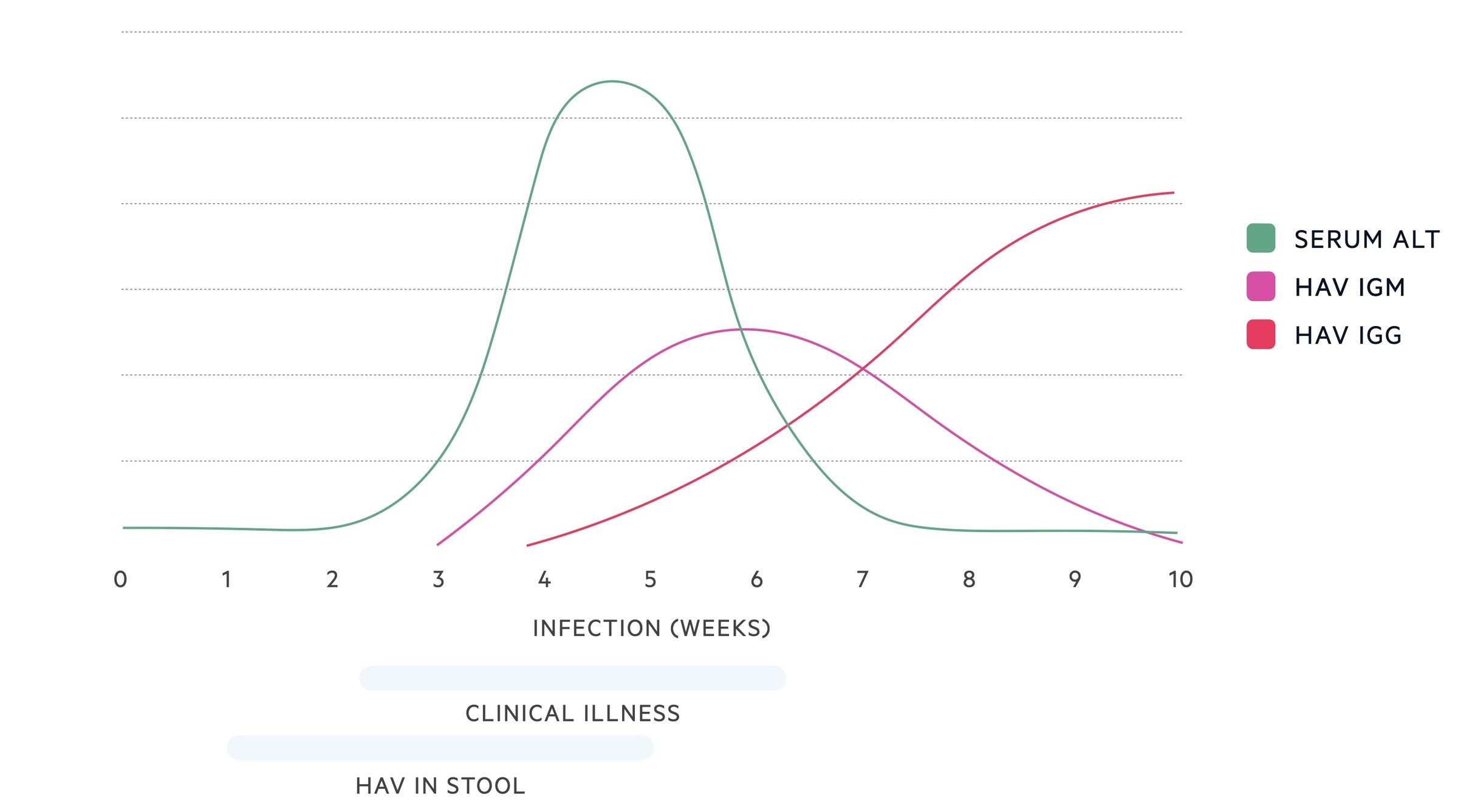
Hepatitis A IgM and Hepatitis A IgG antibodies (HAV-IgM, HAV-IgG) may be used to diagnose the infection.
Liver enzymes
- ALT/AST: Tends to be significantly elevated, between 500 and 10,000 IU/L
- Bilirubin: Tends to be moderately elevated, between 50 and 200 micromols/L
- Prothrombin time: Tends to be normal, may be elevated in complicated disease
Serology
HAV-IgM is positive soon after symptoms develop and tends to remain detectable for a few months. HAV-IgG becomes positive 5-10 days after symptoms develop and remains lifelong.
- +ve HAV-IgM, +ve HAV-IgG: Likely acute hepatitis A infection
- +ve HAV-IgM, -ve HAV-IgG: May indicate acute infection or false positive IgM
- -ve HAV-IgM, +ve HAV-IgG: Indicates previous infection or vaccine based immunity
- -ve HAV-IgM, -ve HAV-IgG: No evidence of infection, may be very early or still in the incubation phase
Repeat serology may be sent if negative but the patient is in the first 7-10 days of symptomatic disease.
NOTE: A hepatitis A RNA PCR has been developed but is not commonly available.
Management
Management tends to be supportive except in the most severe cases.
The majority of patients do not need hospital admission. However any patient who is unwell or has significant liver impairment should be admitted and referred to hepatology.
Supportive
- General points: the majority of patients simply require supportive care. Advise good oral hydration and rest. Alcohol should be avoided.
- Nausea: metoclopramide (max. 5 days) or cyclizine can be given if there is no significant liver impairment. In the presence of liver impairment discuss with specialists.
- Pruritus: chlorphenamine can be prescribed in the absence of liver impairment. In the presence of liver impairment discuss with specialists.
- Reduce transmission: stay at home, good hygiene, avoid unnecessary contact and unprotected sex for 7 days after jaundice appears or symptoms began.
Pregnancy
The information on the impact of hepatitis A on pregnancy is limited. There is thought to be an increased risk of miscarriage or pre-term labour when it occurs in the second and third trimester.
Breastfeeding is not known to transmit the virus. Good personal hygiene is advised.
Notification and contacts
Clinicians should contact their local Health Protection Unit to allow contact tracing and monitoring of outbreaks.
In England hepatitis A is a ‘notifiable disease’, meaning you must notify a Proper Officer of the local authority.
At risk contacts should be reviewed, if they have not been vaccinated, immunoglobulin should be considered. Typically the hepatitis vaccine will be offered.
Further care
- Referral: Consider the need for a GUM clinic or drug rehabilitation services.
- Follow up: Patients should be reviewed on a weekly basis for clinical review and repeat LFTs. Refer to specialist services if clinically worsening or worsening or persistently abnormal LFTs.
Vaccination
Hepatitis A vaccine is recommended to those at risk of infection and at risk of complications off infection.
Individuals who should be offered vaccination include:
- Travel (to endemic areas)
- Chronic liver disease
- Sexual (MSM, high risk activities e.g analingus, digital-rectal contact, chemsex)
- Occupational risks
- IVDU
It is available as a monovalent vaccine or in combination with hepatitis B or typhoid. The contents of each vaccine and the patients allergy status must be checked.
The first dose should be given at least 2-3 weeks prior to travel. Extra doses may be recommended if long term protection is needed.
Complications
Rarely hepatitis A leads to more serious illness and complications needing specialist care.
- Relapsing hepatitis (may occur in 5-15%)
- Fulminant liver failure
- Prolonged cholestasis
- Others (interstitial nephritis, acute pancreatitis, red cell aplasia, Guillain-Barre syndrome)

