Platelet Disorders
These can arise due to decreased bone marrow production, excess destruction or poor functioning
– These abnormalities are divided into quantitative (low platelet count due to bad supply or removal) and qualitative disorders (where there is a problem with the structure or function of the platelet)
– Clinical features usually involve mucosal and skin bleeding.
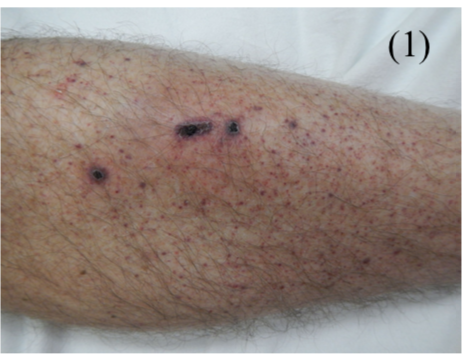
– Skin bleeding –> leads to petechiae + Purpura (3mm) + Easy bruising.
– Mucosal bleeding –> leads to epistaxis (most common symptom) + GI bleeding + hematuria
Qualitative Platelet Disorders
Immune Thrombocytopenic Purpura (ITP)
This is an autoimmune production of antibodies directed against platelet antigens, such as the glycoprotein IIb/IIIa or Ib-V-IX complex
– It can be associated with autoimmune haemolytic anaemia – this is called Evan’s syndrome.
– Can be acute –> seen in children weeks after viral infection, but self-limiting and resolves within weeks
– Can be chronic –> Seen in women of childbearing age, primary or secondary to conditions (e.g. SLE)
– IgG antibodies can cross placenta to give thrombocytopenia in offspring for a short time after birth.
Symptoms:
– Purpura and petechiae, especially on the extremities
– Bleeding (Epistaxis and menorrhagia)
Tests:
A diagnosis of exclusion (need to ensure not due to other blood conditions)
– Low platelet count + increased megakaryocytes on bone marrow biopsy
– Normal PT/APTT as the coagulation cascade is unaffected
Management:
– 1st line corticosteroids (children respond well, but adults may relapse)
– In symptomatic bleeding, give IV immunoglobin to raise platelet count
Microangiopathic Haemolytic Anaemia (MAHA)
This is the pathological formation of platelet microthrombi in small vessels, which consumes up platelets.
– RBCs are sheared as they cross microthrombi, resulting in hemolytic anaemia with schistocytes.
– This can be seen in a few different conditions
Haemolytic Uraemic Syndrome (HUS):
This is a conditions which is seen in children usually after an infective gastroenteritis (food poisoning) episode
– Primary HUS occurs due to complement dysregulation
– Secondary HUS is usually due to Shiga-toxin from E. Coli (STEC) 0157:H7.
– The bacterias produces a toxin damaging endothelium causing excessive platelet aggregation
Symptoms:
(history of diarrhoea)
– AKI
– Bleeding (purpura and epistaxis)
– Microangiopathic Haemolytic Anaemia
Tests:
– U&E shows AKI
– FBC – shows anaemia and thrombocytopenia
– Stool culture – shows E. Coli infection
Management:
Usually supportive, with fluids and blood transfusion (no antibiotics required)
– Plasmapheresis (blood plasma exchange) used in severe cases
Thrombotic Thrombocytopenic purpura (TTP)
This is a condition which occurs due to a deficiency of the enzyme which usually cleaves vWF into monomers
– This leads to large, uncleaved vWF giving abnormal platelet adhesion, resulting in microthrombi
– It can be congenital or due to an acquired autoantibody, more commonly in adult females
Symptoms:
– Haemolytic Anaemia
– Thrombocytopenia (giving bleeding with purpura and epistaxis)
– AKI
– Fever
– Neurological features e.g. headache, seizures
Management:
A haematological emergency –> Plasma exchange (removes antibodies) + Steroids
Heparin-Induced Thrombocytopenia (HIT)
This is one of the most severe side effects of heparin therapy, where antibodies form against the heparin platelet complex, which leads to platelet destruction
– Paradoxically, the fragments of destroyed platelets can activate the remaining platelets, giving thrombosis
– Unlike the other heparin side effects, this is slower and takes longer to develop, around a week.
Symptoms:
Reduction in platelets, allergy + thrombosis giving MI/stroke or DVT
Tests:
Complete platelet count

