Overview
Hodgkin lymphomas are characterised by the presence of Hodgkin/Reed-Sternberg cells.
Lymphoma is a haematological malignancy arising from lymphoid tissue. They are commonly categorised as Hodgkin or Non-Hodgkin lymphoma:
- Hodgkin lymphoma (HL): Characterised by the presence of Hodgkin/Reed-Sternberg cells. Further categorised as classical Hodgkin’s lymphoma (nodular sclerosis, mixed cellularity, lymphocyte-rich and lymphocyte-depleted) and nodular lymphocyte-predominant Hodgkin’s lymphoma.
- Non-Hodgkin lymphoma (NHL): Reed-Sternberg cells are not seen in NHL. There are more than 60 subtypes and they can be B-cell or NK/T-cell in origin. B-cell lymphomas are more common accounting for around 80%, though there is significant geographic variation. NHLs are more common than Hodgkin lymphoma, accounting for around 80-85% of lymphomas.
This note is an introduction to HL, primarily focused on classical HL. The cause of HL is poorly understood though it has been linked with Epstein Barr Virus (EBV). Other risk factors include smoking, HIV and immunosuppression.
Epidemiology
In the UK, there are approximately 2,100 cases of Hodgkin lymphoma diagnosed each year.
It is more common in men (1,300 cases in 2017) than women (880 cases in 2017). In the past decade incidence has increased by almost 20%.
HL is far less common than NHL which has around 14,000 cases a year. Approximately 330 people die from Hodgkin lymphoma each year.
HRS cells
HL is characterised by the presence of Hodgkin/Reed-Sternberg cells (HRS cells)
Reed-Sternberg cells are large, multinucleated malignant cells – they are often described as having an owl like appearance. Hodgkin cells refer to the mononuclear variant of Reed-Sternberg cells.
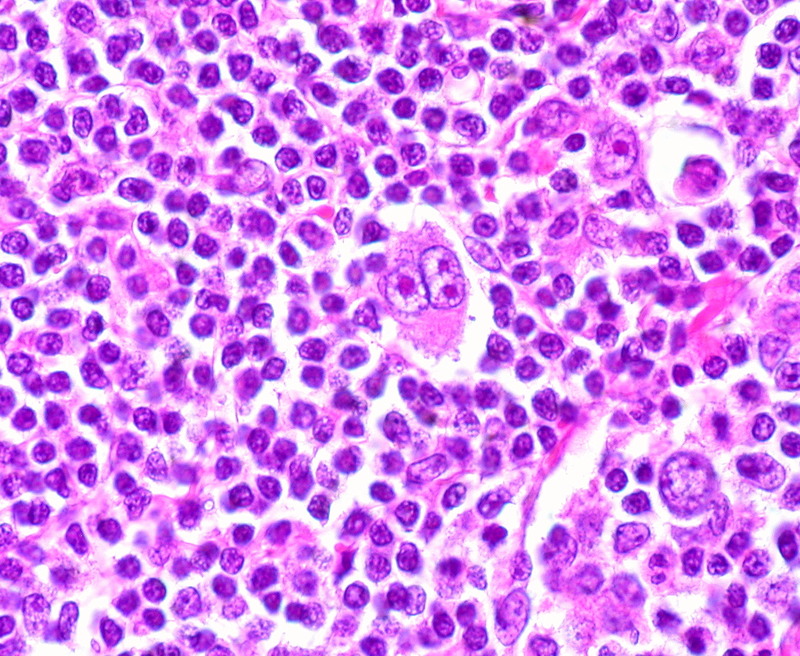
Multinucleated Reed-Sternberg cell seen in centre of image
Image courtesy of Dr Ed Uthman
A rare form of HL, nodular lymphocyte-predominant Hodgkin lymphoma is characterised by the lymphohistiocytic Reed-Sternberg variant.
Types
HL may be subdivided into classical and nodular lymphocyte-predominant Hodgkin lymphoma.
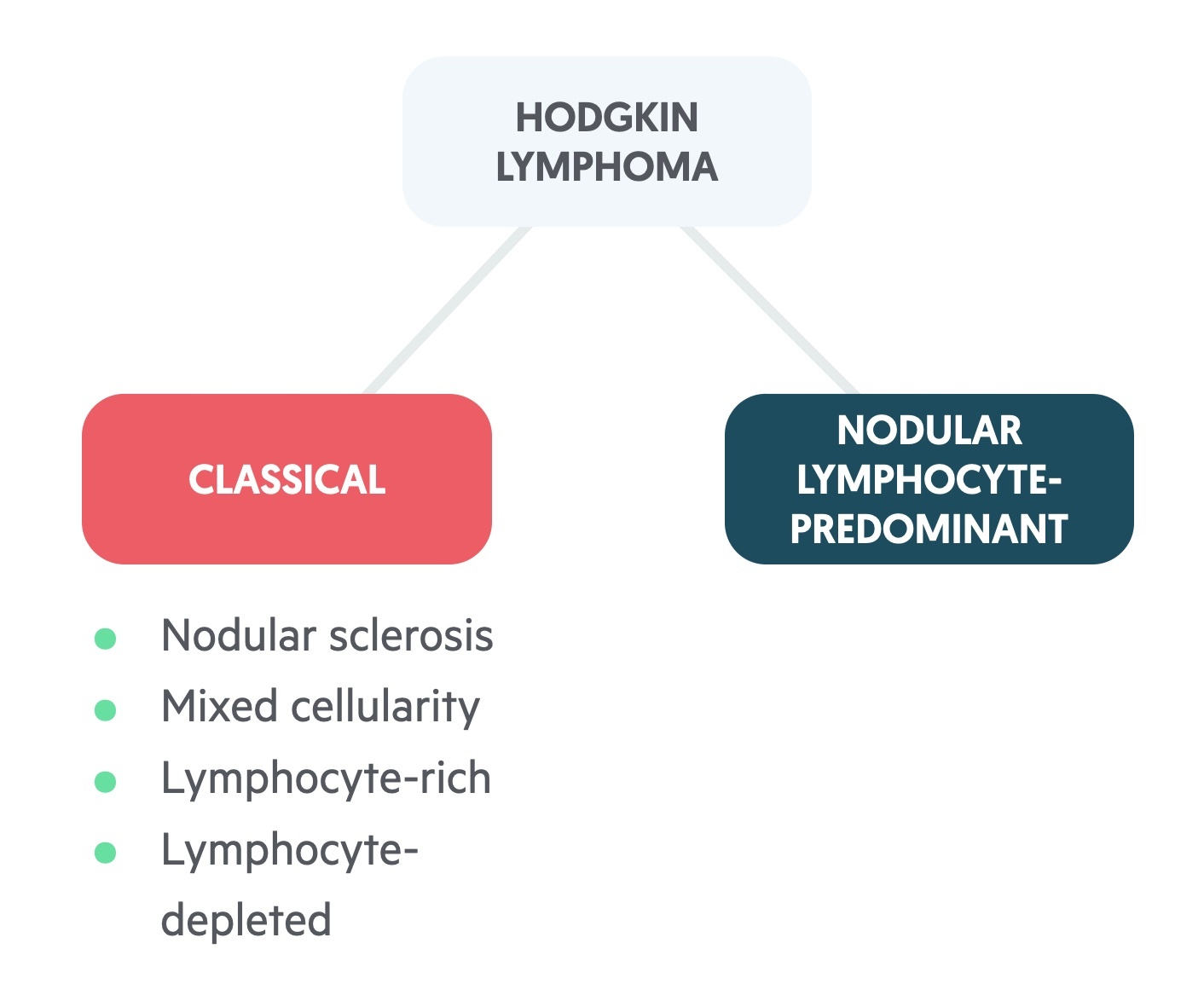
Classical
The four ‘classical’ forms of HL (cHL) account for around 95% of cases of HL. There are four subtypes:
- Nodular sclerosis: Most common subtype, accounts for around 70% of cHL.
- Mixed cellularity: Accounts for around 20% of cHL.
- Lymphocyte-rich: Accounts for around 5% of cHL. Has the best prognosis.
- Lymphocyte-depleted: Rare, accounting for <1% of cHL. Has the the worst prognosis.
Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL)
An exceedingly rare condition accounting for around 5% of HL. It is characterised by the lymphohistiocytic Reed-Sternberg variant.
It shows a significant male preponderance and is more common in those of black ethnicity. It tends to follow a different course and is managed uniquely. This is beyond the scope of this note which focuses on cHL.
Clinical features
HL tends to present with gradual lymphadenopathy, malaise and fatigue.
- Lymphadenopathy: Typically painless, firm, enlarged lymph nodes, most commonly found in the neck.
- ‘B’ symptoms: ‘B’ symptoms refer to fever, night sweats and weight loss (unexplained, >10% in 6 months).
- Mediastinal mass: May be incidental finding on chest imaging or present with shortness of breath, cough, pain or superior vena cava obstruction.
- Pruritis
- Hepatosplenomegaly
- Malaise
- Fatigue
Diagnosis
Excision biopsy of affected lymph nodes is normally required in patients with suspected cHL.
Excisional biopsy is preferred to fine needle aspiration or core biopsy. cHL is diagnosed following biopsy and immunophenotyping of HRS cells.
Investigations
PET/CT is the preferred imaging modality for staging disease.
Bloods
- FBC
- UE
- LFT
- Bone profile
- LDH
- Uric acid
- ESR
- HIV, Hep B and Hep C
- HTLV-1
Imaging
- Chest x-ray
- PET CT: Used in the staging of disease.
- CT neck, chest, abdomen and pelvis: May have been organised prior to diagnosis. Also used to characterise disease seen on PET, particularly in the neck.
- MRI: MRI brain used If CNS involvement suspected, also useful to image the liver.
Additional
- Lumbar puncture and CSF analysis: In those with suspected CNS disease.
- Echocardiogram: Assess cardiac function, particularly if considering doxorubicin chemotherapy.
- Pulmonary function tests: Tests pulmonary function, particularly if considering bleomycin chemotherapy.
- Bone marrow biopsy: Due to modern imaging techniques biopsy is often not needed. May be considered if diagnosis uncertain or imaging indeterminate.
Lugano staging
The Lugano staging system is used to classify HL.
It describes the anatomical distribution of disease and is of both prognostic and therapeutic importance.
The system originates from an international conference in Switzerland in 2011 (and many further meetings), and is an attempt to update the Ann-Arbor system to reflect changes in the decades since it was introduced.
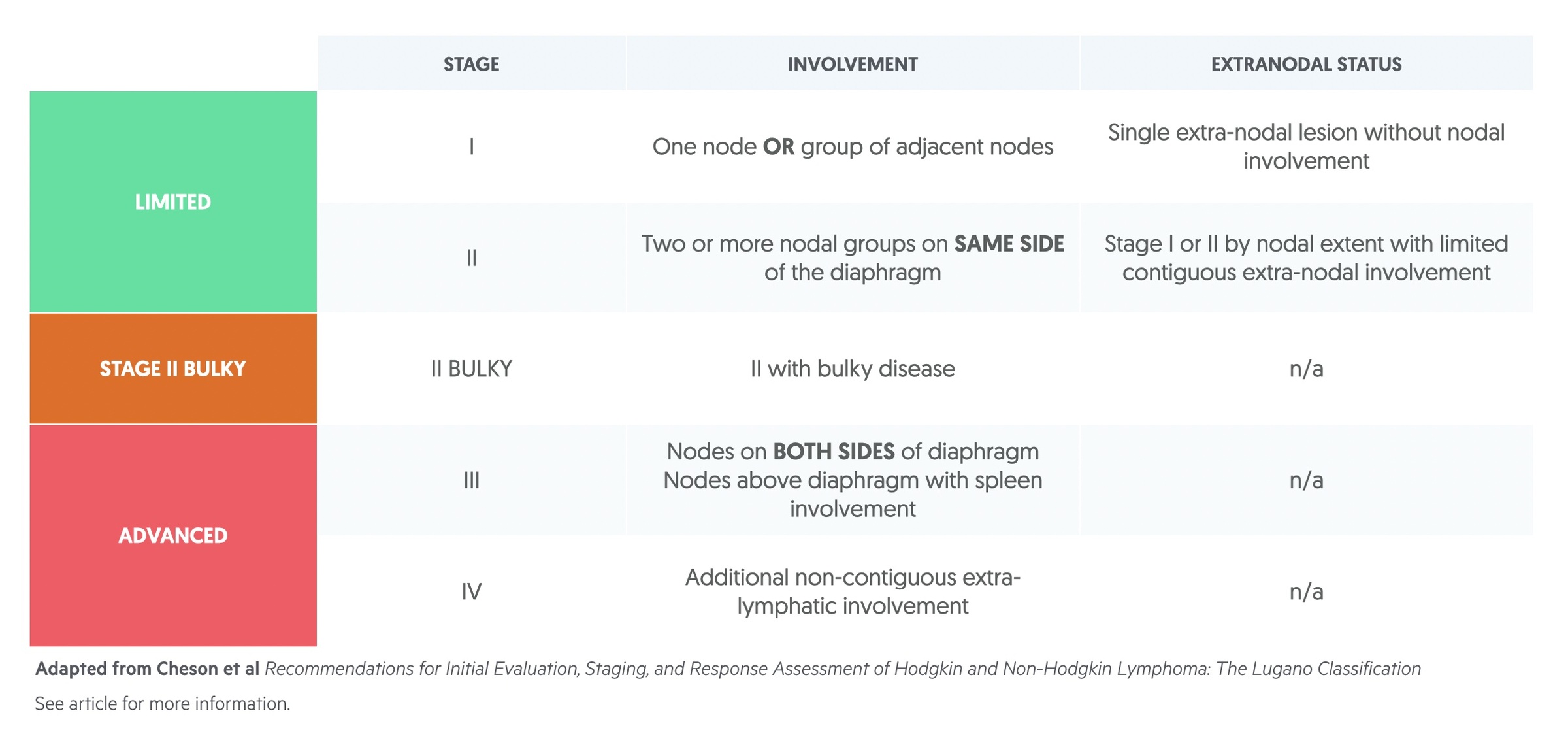
The staging is further modified by the presence or absence of a number of features:
- ‘B’ symptoms: ‘B’ symptoms refer to fever, night sweats and weight loss (unexplained, >10% in 6 months). ’B’ denotes presence and ‘A’ denotes absence.
- Extranodal involvement: In limited stage disease ‘E’ is used to denote extranodal tissue involvement.
- Bulky disease: Definition of bulky is nuanced but typically refers to disease > 10cm.
Management
Chemotherapy and radiotherapy are the mainstay of management in patients with cHL.
The management of cHL is complex and depends on the Lugano staging and other prognostic markers (age, ESR, number of regions involved and presence of bulky mediastinal disease).
ABVD
ABVD is a commonly used regimen in the treatment of cHL, and the one you will be expected to be aware of at an undergraduate level. It consists of four chemotherapy agents:
- Doxorubicin (A): An anthracycline that inhibits topoisomerase II leading to inhibition of DNA and RNA synthesis. Side effects include cardiomyopathy, myelosuppresion and skin reactions.
- Bleomycin (B): Inhibits DNA synthesis. Side effects include pulmonary fibrosis and severe idiosyncratic reaction (characterised by hypotension, confusion, fever, wheeze)
- Vinblastine (V): Inhibits microtubule formation by binding to tubulin. Side effects include peripheral neuropathy and bladder atony.
- Dacarbazine (D): Converted to MTIC an alkylating agent that acts on guanine and causes methylation. Side effects include bone marrow suppression and hepatic necrosis.
Early stage
In patients with stage I/II disease ABVD chemotherapy is the mainstay of treatment. Number of cycles vary case to case but 3 to four are common. This may be followed by radiotherapy.
Advanced stage
Advanced stage refers to stage III/IV, sometimes stage II bulky disease will be included here. A number of treatment regimens may be used:
- ABVD
- BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone)
- Stanford V (doxorubicin, vinblastine, mechlorethamine, vincristine, bleomycin, etoposide, and prednisolone)
Radiotherapy may be used as an adjunct to chemotherapy.
Relapse
Treatment of relapsed disease depends on many factors including prognostic indicators, timing (following first treatment) and number of relapses. Treatment options include salvage chemotherapy, radiotherapy and autologous haematopoietic cell transplantation.
Blood transfusion
If a blood transfusion is required, patients with or treated for Hodgkin lymphoma must received irradiated blood. This is to reduce the risk of transfusion-associated graft-versus-host disease.
The advice is ‘all adults and children with Hodgkin lymphoma at any stage of the disease should have irradiated red cells and platelets for life’. There are a number of other indications for irradiated blood products. For more information see the British Society of Haematology page.
Prognosis
Overall cHL has a reasonably good prognosis.
- Limited disease: Of those with stage I and II disease, 90% survive 5 years.
- Advanced disease: Of those with stage III and IV disease, 75-90% survive 5 years.
Upwards of 75% of patients will be cured of the condition, though this is dependent somewhat on the staging at diagnosis.

