Sodium
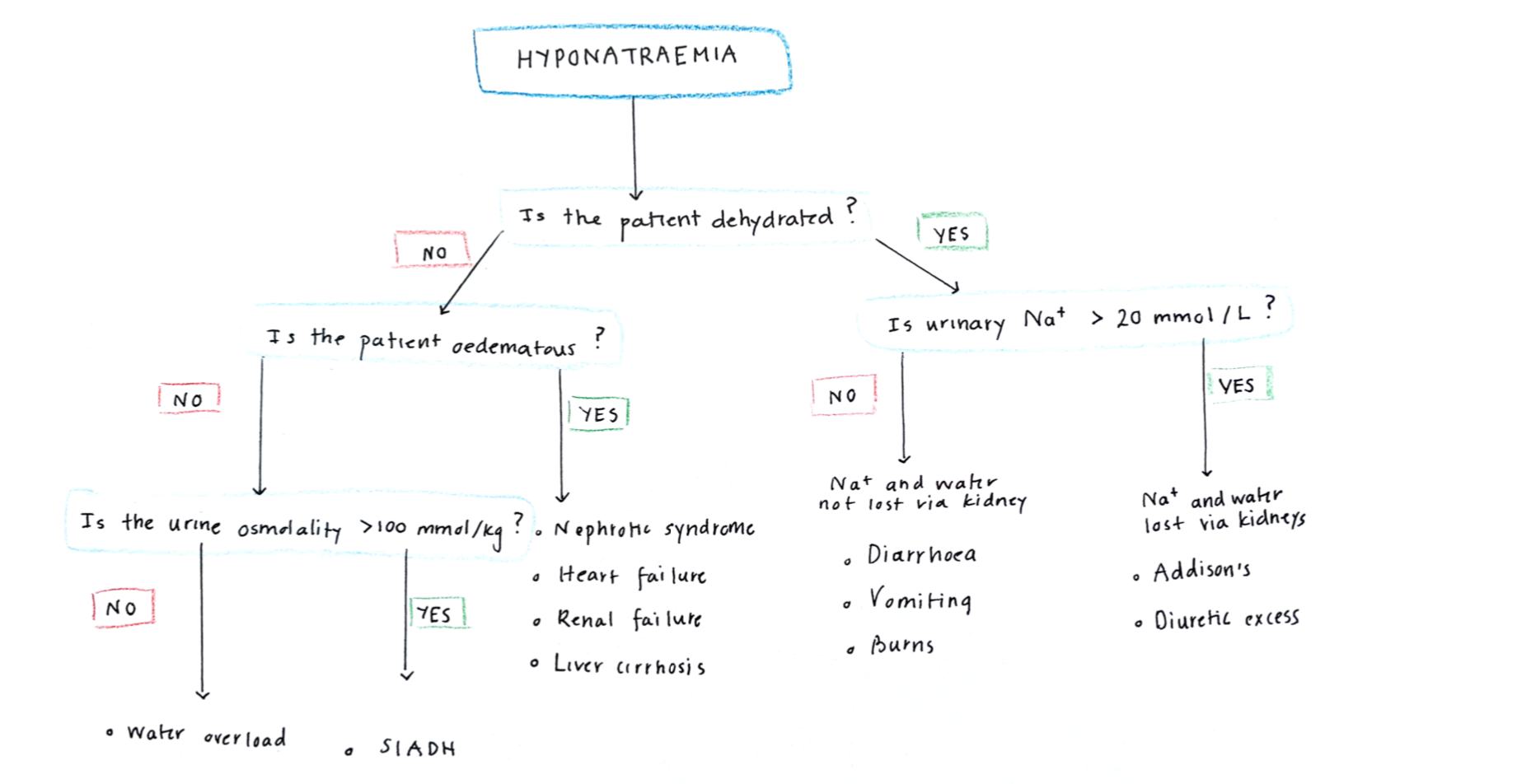
Hyponatraemia
This is a low concentration of plasma Na+. As the concentration depends on both sodium levels and water volume, hyponatreamia can either be due to a lack of sodium ions or too much water.
Causes:
The main way to distinguish the causes is first assessing if the patient is dehydrated or full of water.
– If dehydrated, this suggests the primary problem is losing Na+ ions, and water indirectly follows as a result.
–> Kidney etiology – Addison’s disease or renal failure
–> Outside kidneys – Burns, diarrhea, small bowel obstruction
– If not dehydrated, this suggests that there is excessive relative water retention occurring, causing the plasma to become more diluted.
–> If patient has oedema (hypervolaemic), suggests kidney, liver, heart failure
–> If no oedema (euvolemic), either SIADH or water overload
Symptoms:
(Low osmolality will make the brain swell giving symptoms of raised ICP)
– Starts with anorexia, nausea and malaise
– Then get headache, confusion, low GCS and seizures
– Increased risk of falls in the elderly
Artefacts:
– Hyponatremia can occur if blood sample was taken from an arm with a drip
– If there are high levels of lipid/protein/glucose
– Iatrogenic hyponatremia ➔ if 5% glucose is infused IV without saline, glucose gets metabolized giving a hypotonic solution causing hyponatreamia. Can give cerebral oedema usually in young adults
Management
Correct underlying cause, never just treat Na+ concentration alone
– Fluid restriction and rehydration with saline
Central Pontine Myelinosis
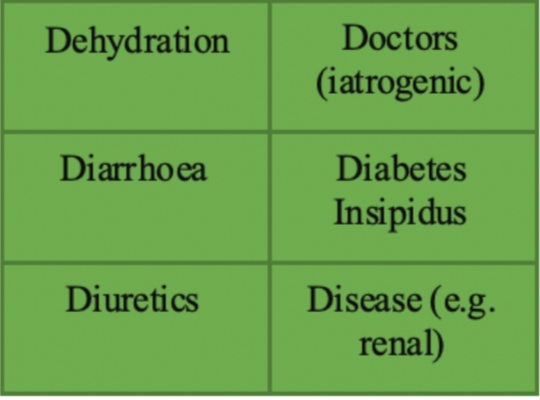
Hypernatremia
This usually occurs due to water loss in excess of Na+ loss (high osmolality):
– DEHYDRATION –> vomit, burns
– DIABETES insipidus
– DOCTORS: incorrect IV fluid replacement (excessive saline)
Symptoms:
– Thirst
– Weakness and lethargy
– Irritability, confusion and coma
Management:
If in coma –> glucose 5% IV slowly guided by fluid balance and sodium levels
– Again, be careful when correcting levels as quick correction can lead to cerebral oedema raising ICP
Potassium
Hypokalaemia
This hyperpolarizes the cell and reduces the excitability of nerve and muscles, causing muscular weakness which leads to muscular paralysis and cardiac arrhythmias
Symptoms:
– Muscle weakness, with hypotonia and hyporeflexia (decreases excitability of nerve + muscle)
– Light-headedness – Arrhythmias + Palpitation – Constipation
Tests:
ECG shows small or inverted T waves, long PR interval + prominent U wave
– If person is on diuretics, raised HCO3- is best indicator that hypokalemia is long standing
Management:
– If mild, oral K+ supplement
– If <2.5mM, IV KCl replacement with cardiac monitoring. (Max rate infusion = 10mM/hour)
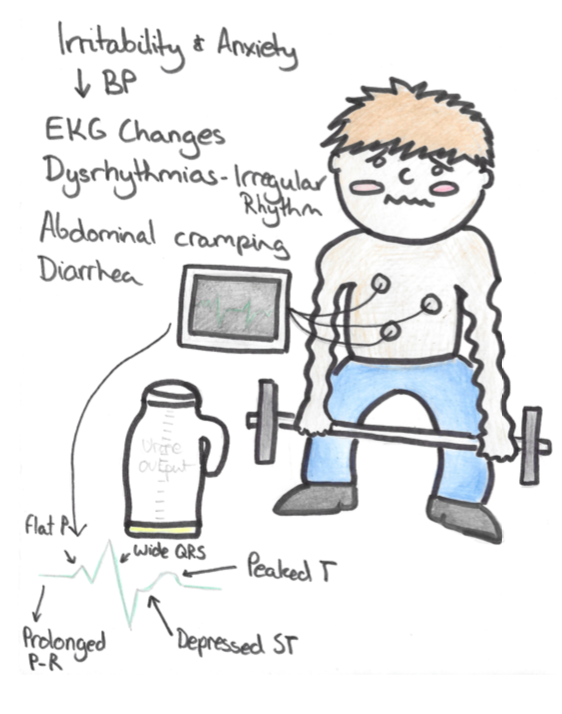
Hyperkalaemia
This often due to renal failure where GFR drops below 20%
– Depolarises cells bringing them closer to threshold, increasing excitability of nerve and muscle and raising chances of cardiac arrhythmias.
Symptoms:
– Tachycardic irregular pulse,
– Palpitations, chest pain and light-headedness
Tests:
– ECG shows tall tented T waves, wide QRS (can lead to VF)
N.B. If patient is well but has a high K+ this can be due to artefact. This is caused by K+ leaking out of RBCs –> due to haemolysis, contamination, delayed analysis
Management:
– If single random high K+ reading, do ECG to ensure not an artefact:
– Treat if K+ >6.5mM or if there are visible ECG changes
1. 10ml of 10% calcium chloride/ or calcium gluconate IV, repeated if necessary
2. IV insulin in dextrose solution
3. Nebulized salbutamol (but avoid in tachycardias)
Phosphate
Phosphate is key in making DNA, proteins and membranes – and is a key buffer for H+ ions in the body.
Hypophosphatemia
This is common and of little clinical significance unless very severe
Causes:
Vitamin D deficiency + primary hyperparathyroidism + inadequate intake + refeeding syndrome
Symptoms:
Muscle weakness/rhabdomyolysis, arrhythmias/cardiac arrest, white cell dysfunction
Treatment:
Oral phosphate supplementation
N.B. Never give IV phosphate to a patient who is hypercalcemic/hyperparathyroid (will give precipitates)
Refeeding Syndrome
Calcium
Hypocalcaemia
Ca2+ is tightly bound to negative glycoproteins on the membrane and stabilizes sodium channels
– A decrease in calcium reduces threshold for action potentials – increases excitability of motor neurones.
Causes:
Levels of PTH and Phosphate are very useful in determining cause of hypocalcaemia:
– If raised Phosphate –> chronic kidney disease, hypoparathyroidism, rhabdomyolysis
– If low Phosphate – –> Vitamin D deficiency, pancreatitis, osteomalacia
Symptoms:
Remembered by the acronym SPASMODIC
SPASMODIC
Management:
– If mild, give calcium 5mM/6h
– If severe, 10ml of 10% calcium gluconate
– If due to chronic kidney disease, treat with Vitamin D supplements, Alfacalcidol/Calcitriol
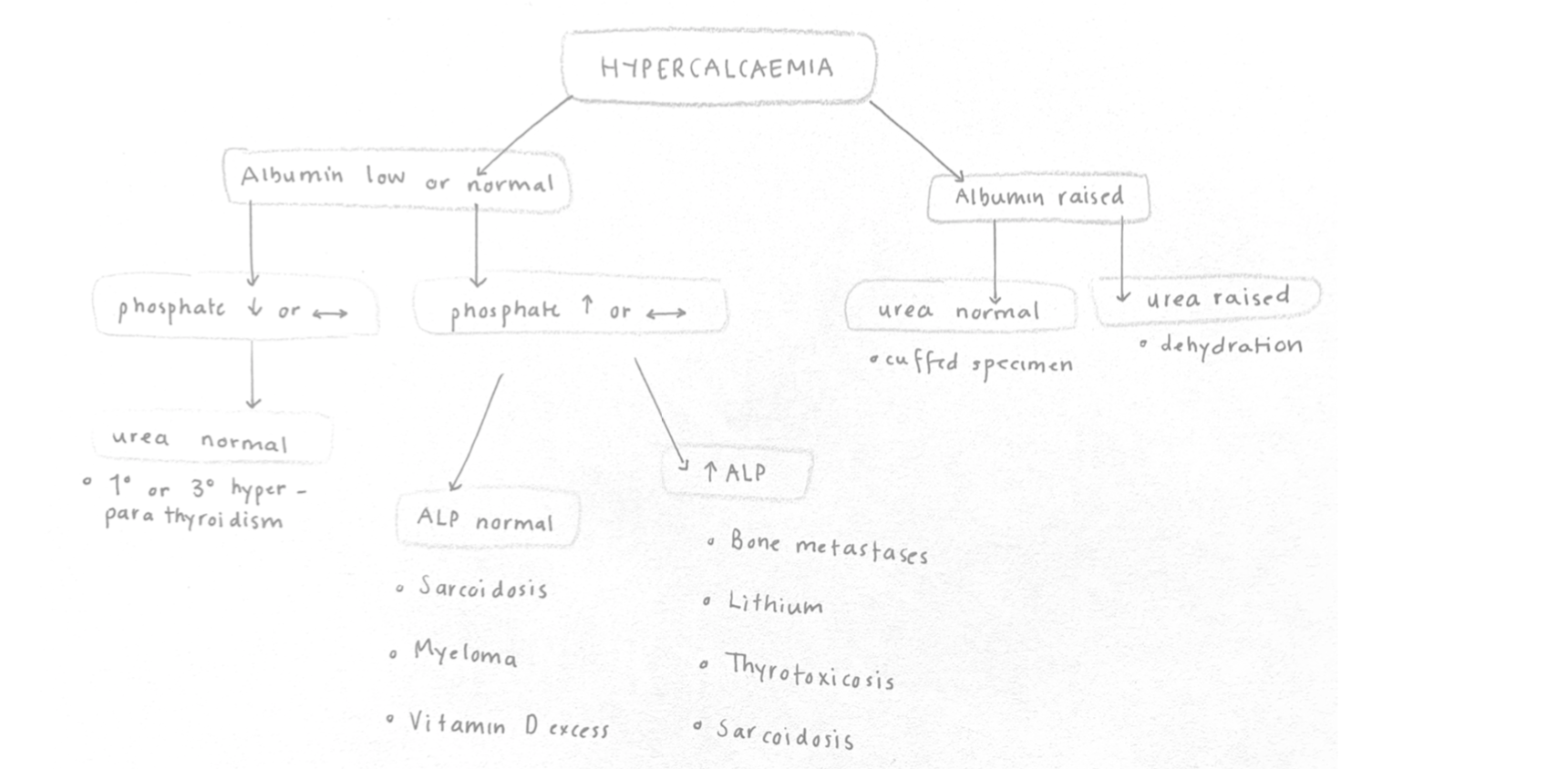
Hypercalcaemia
Most common reasons are malignancy (bone metastases, myeloma) and primary hyperparathyroidism.
– In the blood 40% of Ca2+ is bound to albumin, and the rest is free Ca2+
Symptoms:
– Bones –> Ectopic calcification (e.g. cornea) and bone pain
– Stones –> Renal stones and renal failure
– Groans –> Abdominal pain, vomiting, constipation
– Psychiatric Moans –> Confusion + irritability + Depression
– Other –> polyuria, polydipsia, weakness, fatigue (as it decreases excitability of nerve and muscle)
Investigations
– The main distinction to make is malignancy vs primary hyperparathyroidism
– Look at albumin first –> indicates whether it is due to dehydration (urea also raised) or just an artefact
– If albumin is normal, main determinant is PO43-
– If low, suggests hyperparathyroidism –> also gives high PTH
– If high, look at ALP –> raised ALP from bone turnover (bone metastases)
Management:
1. Give fluids –> IV 0.9% saline
2. Bisphosphonates
3. Treat underlying cause
– e.g. chemotherapy for malignancy
Zinc deficiency
Zinc is required for transcription factors to help transcribe DNA and act as a cofactor in enzymes.
Cause:
Parenteral nutrition or poor diet
Symptoms:
– Dermatitis (red, crusted skin lesions around nostrils and mouth)
– Night blindness
– Diarrhoea
– Alopecia
Management:
Zinc supplements
Magnesium
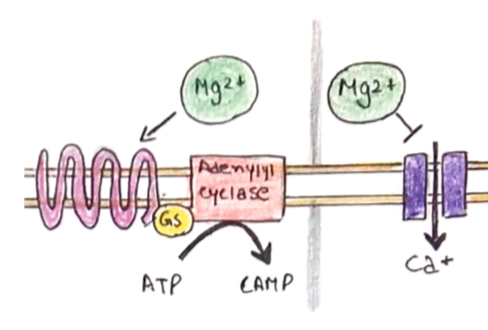
This is a key intracellular ion which has a host of roles within the body. Magnesium is distributed 60% in bone and 35% in cells.
– Ca2+ antagonist stop entry into smooth muscle + enhances Ca2+ uptake to SR
– Also inhibits ACh release whilst giving B2 agonism, increased cAMP
– Plasma concentration tends to follow that of Ca2+ and K+.
Hypomagnesaemia
Like hypocalcaemia this raises the excitability of nerve and muscle as there is less Ca2- reuptake into the SR
Causes:
– Drugs –> Loop and thiazide diuretics
– Poor supply –> Total parenteral nutrition
– Excessive loss –> diarrhea (natural or due to IBD)
– Secondary to low Ca2+, low K+ and low PO43-
Symptoms:
– Increased nerve and muscle excitability (tetany, seizures etc.), seizures, tetany, arrhythmias
– Secondary hypoparathyroidism –> as Mg is needed for PTH secretion
– Can exacerbate digoxin toxicity
Tests:
ECG resembles hypokalaemia (small or inverted T waves, long PR interval + prominent U wave)
Management:
– If <0.4mM –> IV replacement
– If >0.4mM, oral magnesium salts
Hypermagnesemia
Causes:
Renal Failure or iatrogenic (excessive antacids)
Symptoms:
(Weakness) neuromuscular depression, low BP, low pulse, CNS and respiratory depression
Management:
Rarely requires treatment unless very severe
Lipids
Raised cholesterol is a major risk factor for cardiovascular disease, which can be primary or secondary
(Primary) Familial hypercholesterolemia
This is a condition which is due to an autosomal dominant mutation in the LDL receptor
– Means that hepatocytes are unable to internalize LDLs, this raises the concentration in blood
– Should be suspected if cholesterol >7.5mM or cardiovascular events <60 years
Diagnosis:
– This involves measuring cholesterol/LDL level + 1 factor
– In adults, total cholesterol >7.5mM with LDL-C >4.9mM (Children > 6.7mM and LDL >4.0mM) +
– Tendon xanthoma in patients/relative or DNA evidence of FH
Management:
–Atorvastatin 80mg and referral to specialist clinic
N.B. For children if one parent affected, arrange test by age 10. If both parents affected, test by age 5.
(Secondary) Hypercholesterolemia
This can be due to nephrotic syndrome + cholestasis + hypothyroidism
– In these patients it is good to assess QRISK in these patients, this is a risk of CVD of 10% or more
Management:
– If QRISK > 10%, start atorvastatin 20mg 1st line
– If there is already established CVD, then atorvastatin 80mg is 1st line
If on statin, follow up patients every 3 months with full lipid profile ➔ can increase dose up to 80mg.
– Risk of congenital defects means that statins should be stopped in women 3 months before conception.

