Overview
This is a four-part series covering gastrointestinal physiology.
- Part I – Overview of the gastrointestinal system & the oral cavity.
- Part II – Digestion: stomach & control of digestion.
- Part III – Secretion: pancreas & hepatobiliary system.
- Part IV – Absorption: small intestines.
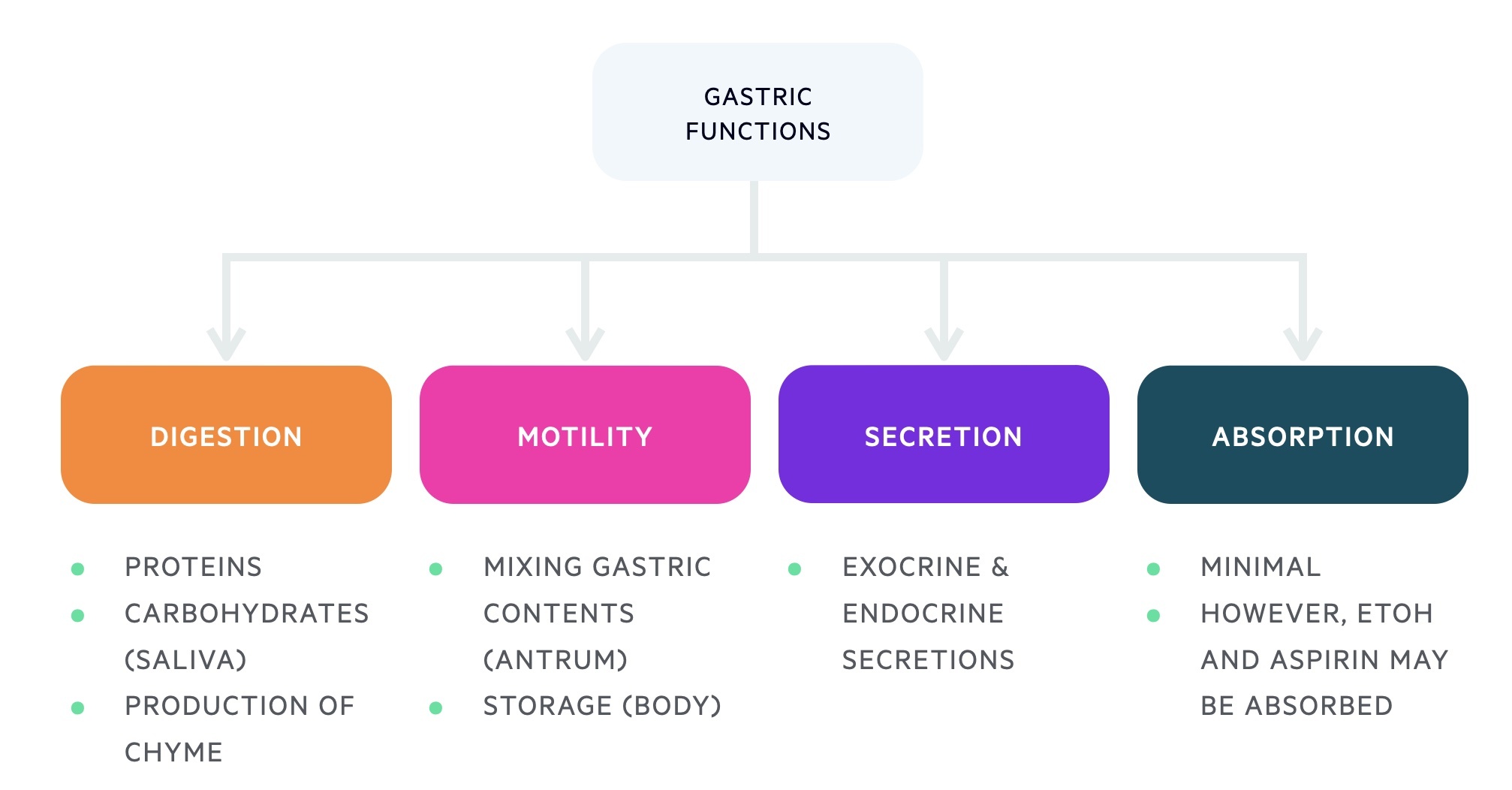
In part II we will take a look at the stomach and its role in digestion. The stomach is a highly specialised organ whose epithelium secretes hydrochloric acid and digestive enzymes. Its capacity reaches around 1-1.5L in adults.
It receives food from the oesphagus and mixes it with gastric secretions, aiding digestion and forming chyme (acidic semi-liquid partially digested material). Chyme is then released into the duodenum under the regulation of a number of factors.
Little absorption occurs in the stomach (the vast majority occurs in the small intestines), however, certain compounds like alcohol and aspirin can be.
Anatomy of the stomach
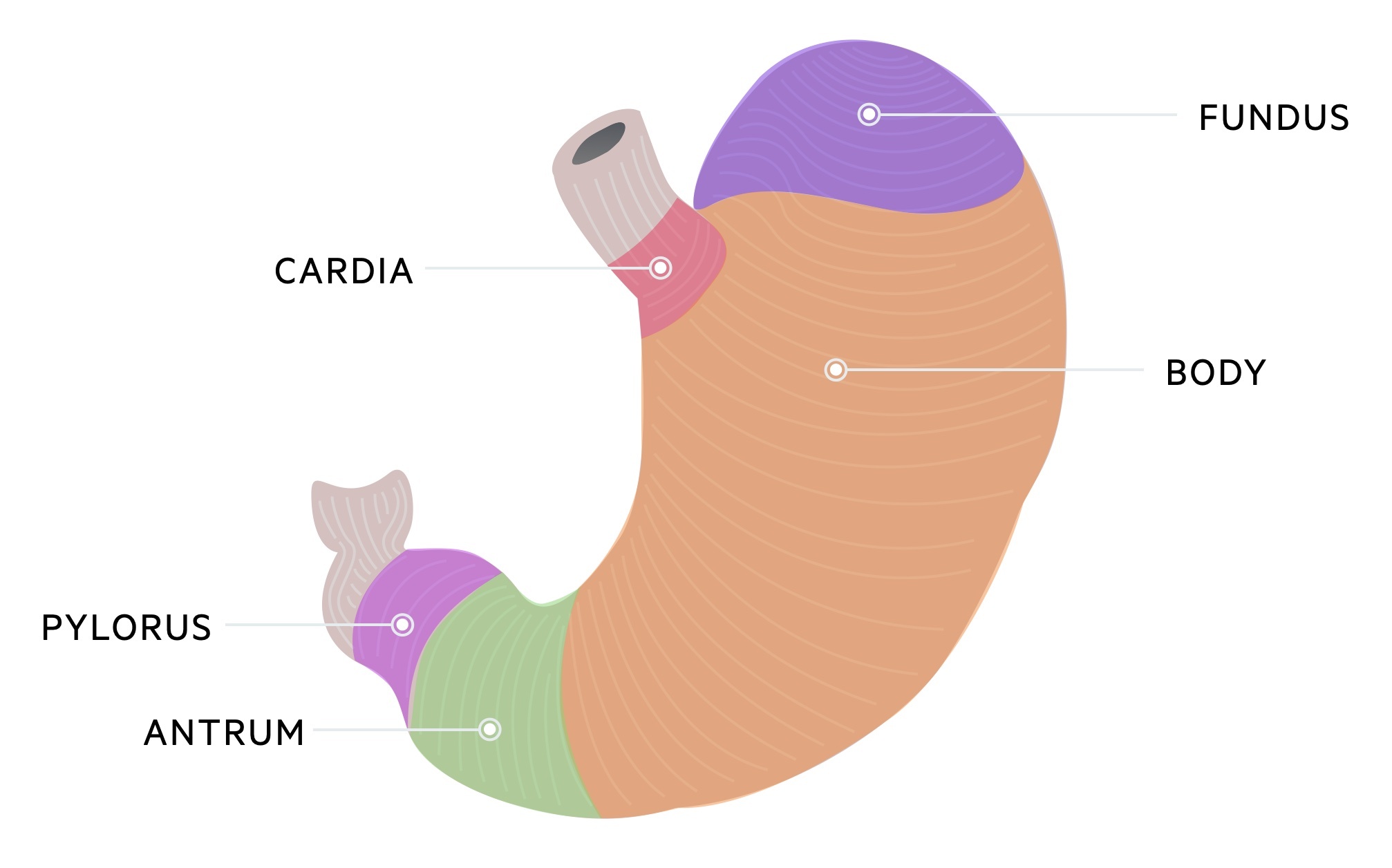
The stomach is divided into five distinct areas; fundus, cardia, body, antrum and pylorus.
The stomach begins at the distal end of the oesophagus beyond the gastroesophageal sphincter. It ends at the pylorus and pyloric sphincter which is in continuity with the first part of the duodenum.
The fundus is the uppermost part of the stomach. It connects to the cardia, which is the superior inlet to the stomach located inferior to the gastro-oesophageal sphincter. The body is the main portion of the stomach and is important in the storage of ingested food.
The muscular antrum comprises the lower section of the stomach, which is vital for mixing gastric contents. The pylorus forms the distal aspect of the stomach, it ends at the pyloric sphincter. This is important for the control of gastric emptying.
Gastric secretions
The mucosa of the stomach is important for the secretion of enzymes and digestive juices.
It is composed of simple columnar epithelium lined by an alkaline mucous layer that protects the cells from the acidic stomach contents. This mucosa contains numerous deep pockets due to infolding, termed gastric pits which themselves contain glands.
Gastric glands are all tubular but have differences in both structure and cell composition and are found in different parts of the stomach. There are three major types of gastric glands:
- Cardiac glands: at the lower oesophageal sphincter
- Oxyntic glands: in the fundus and body
- Pyloric glands: in the antrum and pylorus
Cardiac glands
Cardiac glands contain mucous cells. These produce an alkaline mucous that protects the epithelium of the stomach and acts as a lubricant.
Oxyntic glands
The oxyntic glands are found in the body and fundus of the stomach. It primarily contains important exocrine cells including; mucous cells, chief cells and parietal cells:
- Chief cells: secrete the proenzyme pepsinogen. Pepsinogen is activated by hydrochloric acid into the active enzyme pepsin. Pepsin breaks polypeptides into peptide fragments.
- Parietal cells: also termed oxyntic cells, secrete both hydrochloric acid (HCl) and intrinsic factor:
- HCL acid is responsible for the acidic environment in the stomach (pH 2). HCl is involved in pepsinogen activation, the breakdown of connective tissue, denaturing proteins and has antimicrobial activity.
- Intrinsic factor aids the absorption of vitamin B12. Intrinsic factor binds to vitamin B12, is transported through the intestines and absorbed in the terminal ileum. Impaired intrinsic factor function (pernicious anaemia) results in B12 deficiency.
Other cell types include mucous neck cells, stem cells and neuroendocrine cells.
Pyloric glands
The pyloric glands are found in the antrum and pylorus. Mucous cells are the predominant cell type, they produce an alkaline mucous that protects the epithelium of the stomach and acts as a lubricant.
It contains two important endocrine cells that help to regulate gastric secretions:
- G cells: are involved in the secretion of gastrin, which stimulates parietal cells to secrete hydrochloric acid.
- D cells: secrete somatostatin which has inhibitory action on gastric secretions.
Parietal and chief cells may be sparsely present (parietal cells are seen in the foetal and postnatal period).
Control of digestion
Gastric secretions are coordinated by a series of neurohormonal mechanisms.
Approximately 2 litres of gastric secretions are produced each day. Gastric secretions are crucial for digestion and absorption of nutrients from our diet. The control of digestion is divided into three stages: cephalic, gastric and intestinal.
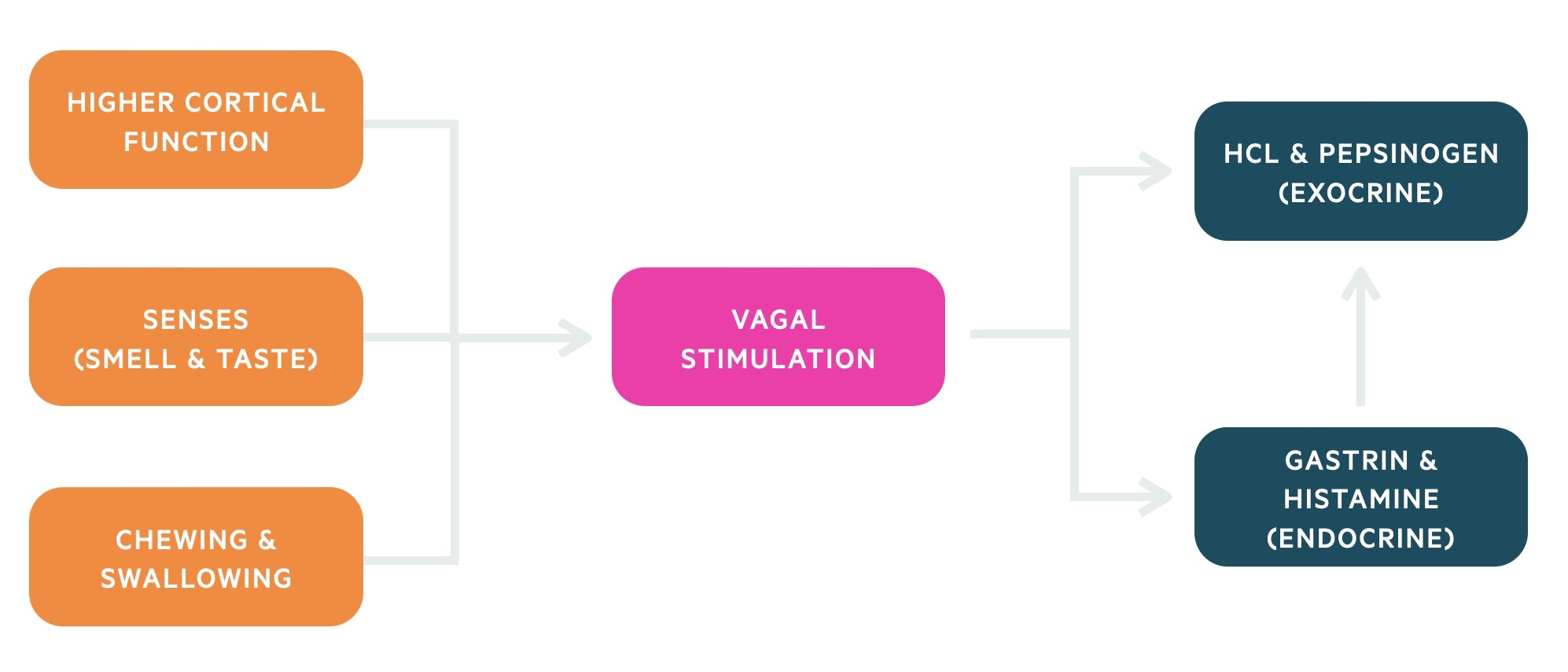
Cephalic
The cephalic stage of digestion occurs prior to the entry of food into the stomach. During the cephalic stage, there is an increase in hydrochloric acid and pepsinogen.
Higher cortical functions, senses (e.g. taste, smell), chewing and swallowing all drive the increases in gastric secretions. These processes lead to vagal stimulation which increases ACh release. ACh acts directly on parietal and chief cells triggering them to secrete HCl and pepsinogen respectively. It can also act indirectly via endocrine cells (e.g. G cells and enterochromaffin-like cells).
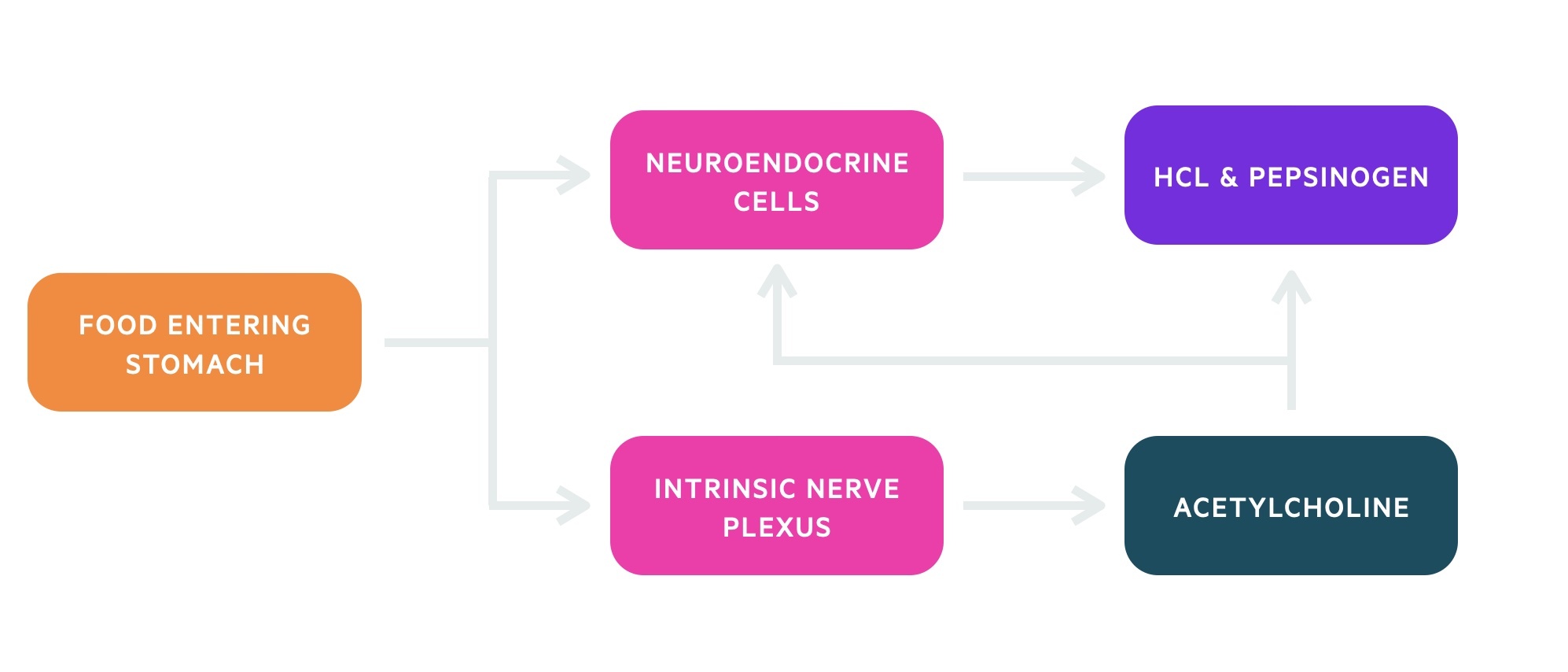
Gastric
The gastric stage features a significant increase in gastric secretions and follows food entering the stomach. Food entering the stomach leads to stimulation of the enteric nervous system and endocrine cells. Protein is the most powerful stimulus during the gastric stage of digestion.
Ultimately, there are many overlapping pathways that occur during the gastric phase of digestion, this culminates in increased secretion of two key products: pepsinogen and hydrochloric acid.
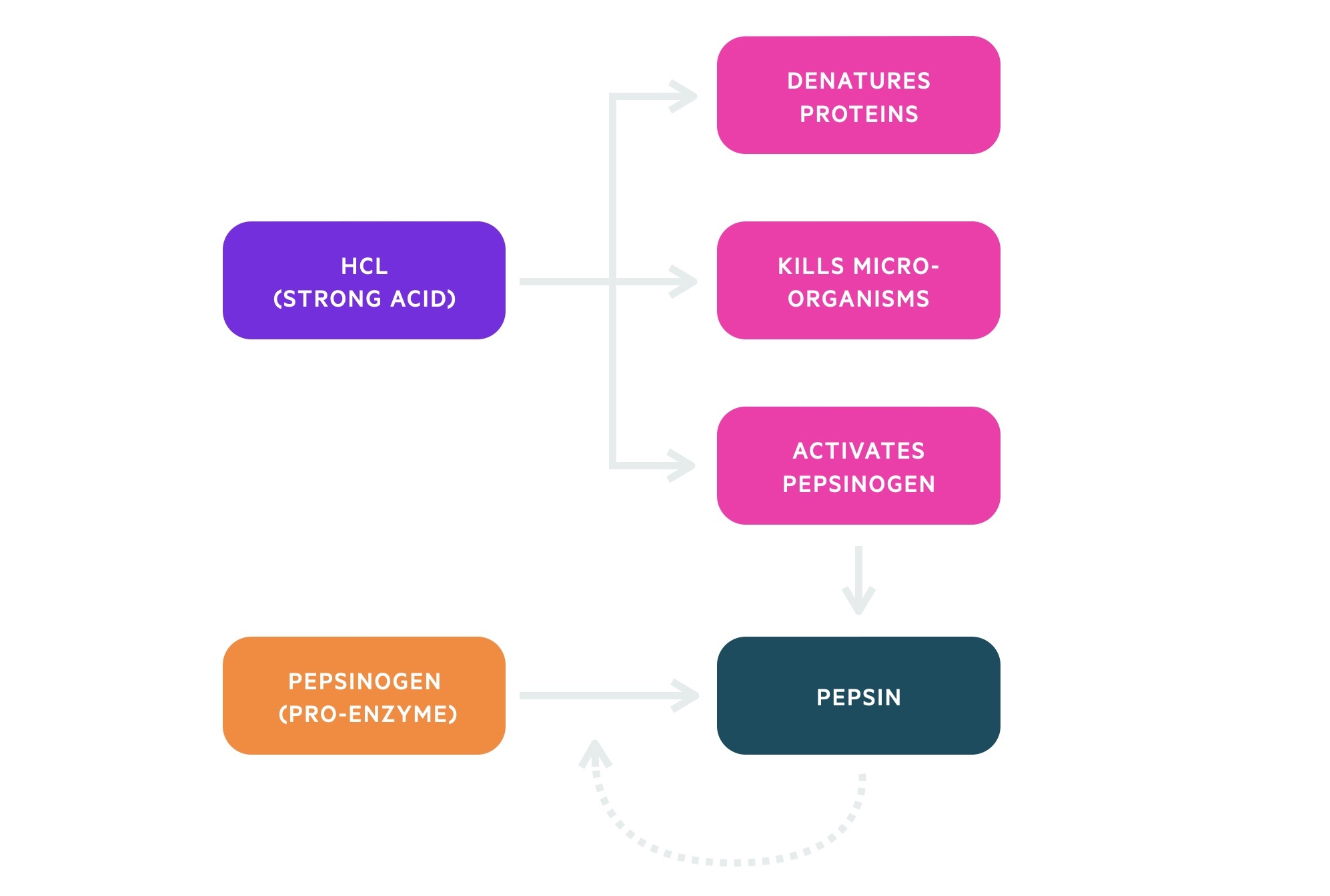
Hydrochloric acid (HCl), a strong acid, has numerous important functions within the stomach. It helps denature proteins and its low pH is key to the innate immune defence. It is also critical for the activation of the proenzyme pepsinogen into the active enzyme pepsin.
Pepsin is important in the breakdown of polypeptide chains into small peptide fragments. Pepsin is able to autocatalyse itself, this mean pepsin can activate pepsinogen. This leads to a significant increase in the availability of the active enzyme.
Intestinal
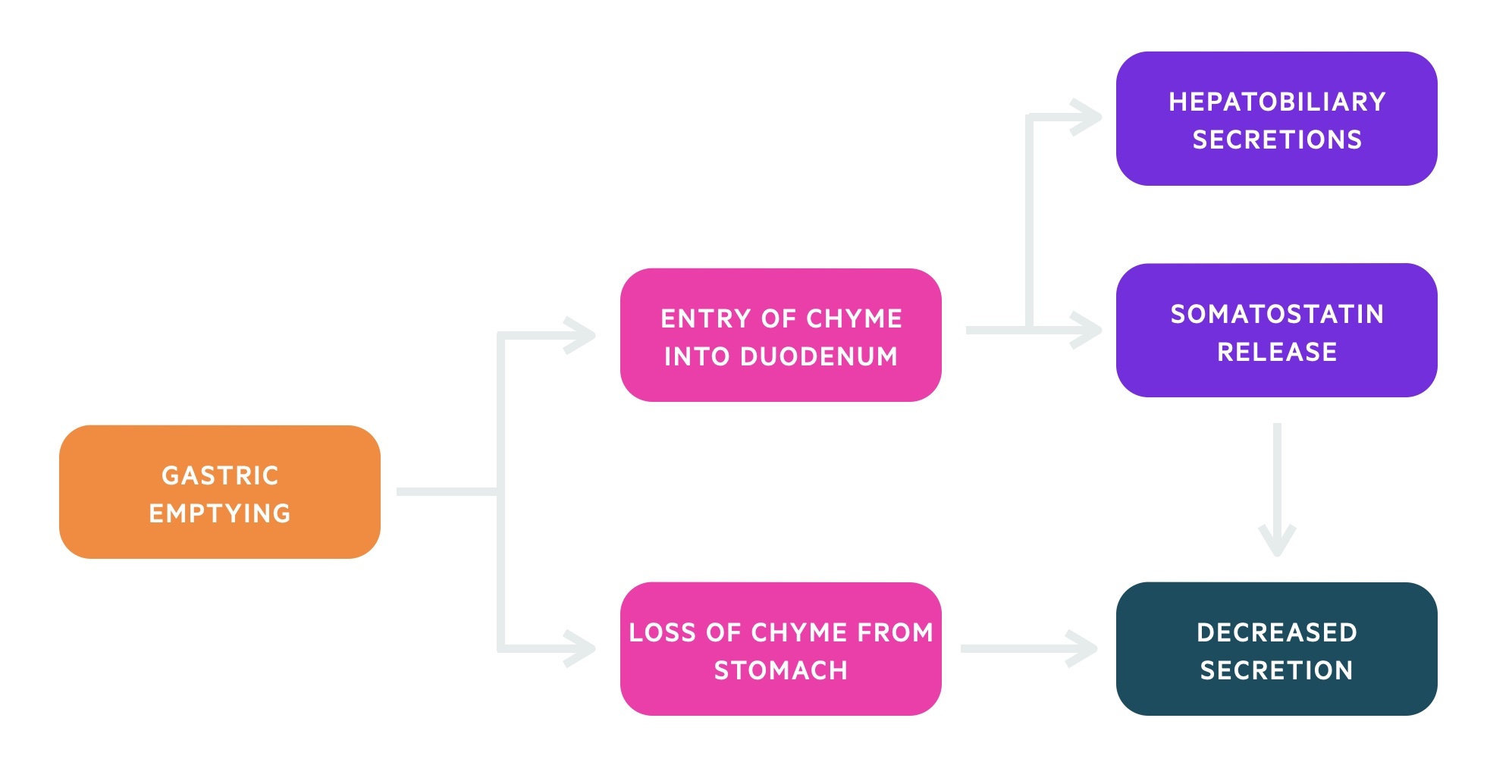
The intestinal stage of digestion is the final phase, which is chiefly inhibitory of gastric secretions. Gastric emptying of chyme into the duodenum stimulates the release of hormones from endocrine cells and activates local neurones.
Activation of D cells leads to the release of the inhibitory hormone somatostatin. This leads to a decrease in gastric secretions. Additionally, the loss of food from the stomach reduces the stimulus for further gastric secretions.
Gastric emptying
Gastric emptying is the process of moving acidic gastric chyme into the duodenum.
It may be regulated by factors arising from the stomach, duodenum or the cortex of the brain (pain/emotion). Factors arising from the duodenum are the main regulatory mechanisms. These include fat, acidity, tonicity and distension.
These four factors trigger both neural and hormonal responses. The neural response is mediated by both the autonomic nervous system and enteric nervous system. They trigger an enterogastrone reflex that slows gastric emptying. The hormonal response leads to the secretion of enterogastrones (CCK, secretin) which delay gastric emptying and initiate hepatobiliary secretions.
NOTE: enterogastrone refers to any hormone that inhibits the forward movement of chyme.


