Overview
The thyroid is an endocrine gland responsible for the production of thyroid hormones T3 and T4.
The major functional cells of the thyroid are the follicular cells. These are arranged into spheres that form a functional unit termed a follicle.
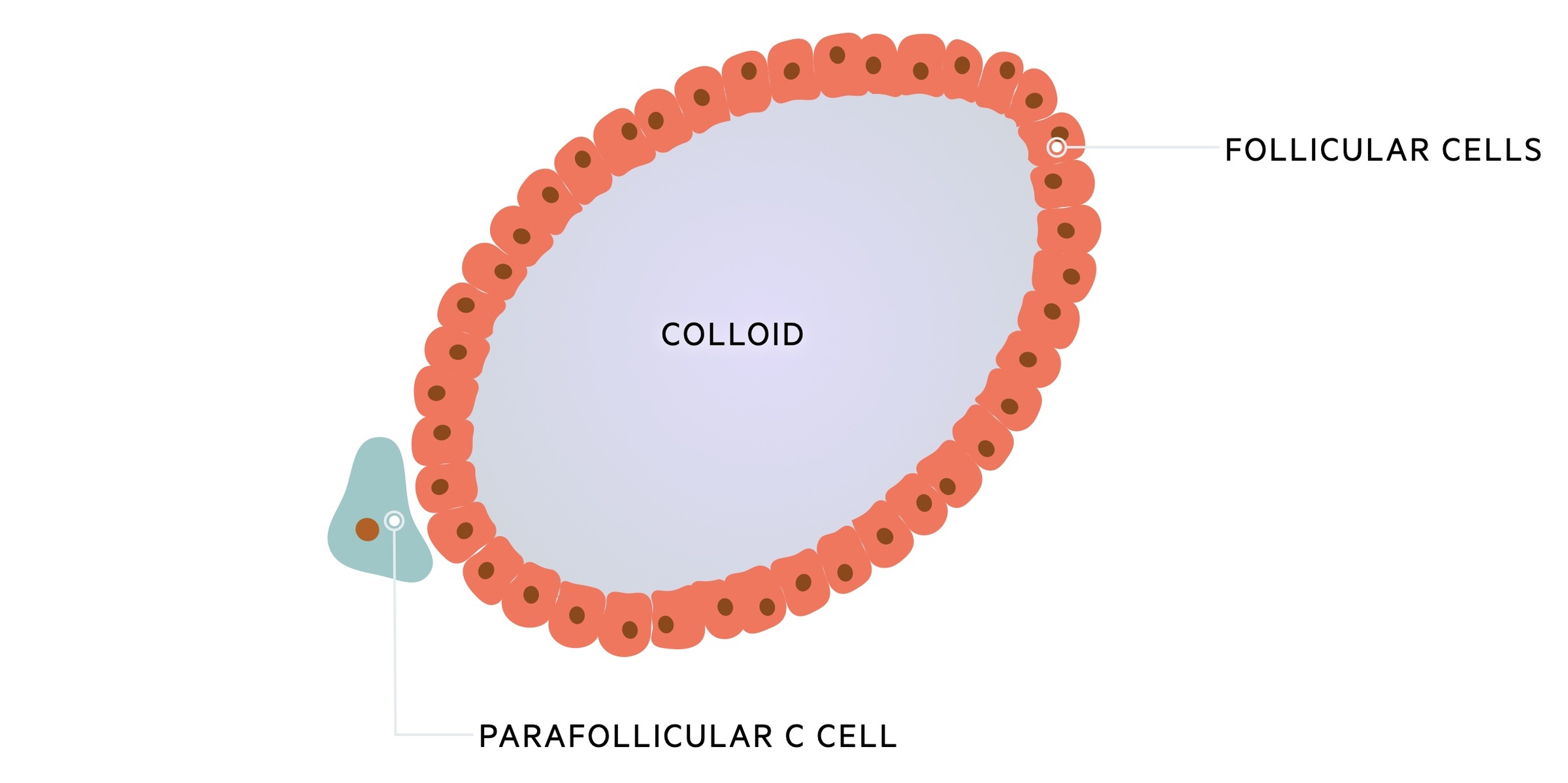
Within these follicles is a central lumen containing colloid; the extracellular storage site for thyroid hormone. Colloid is composed largely of thyroglobulin (Tg) a glycoprotein involved in thyroid hormone synthesis.
Parafollicular C cells secrete calcitonin, a hormone involved in calcium regulation.
H-P-T axis
Thyroid hormone release is controlled by the hypothalamic-pituitary-thyroid axis.
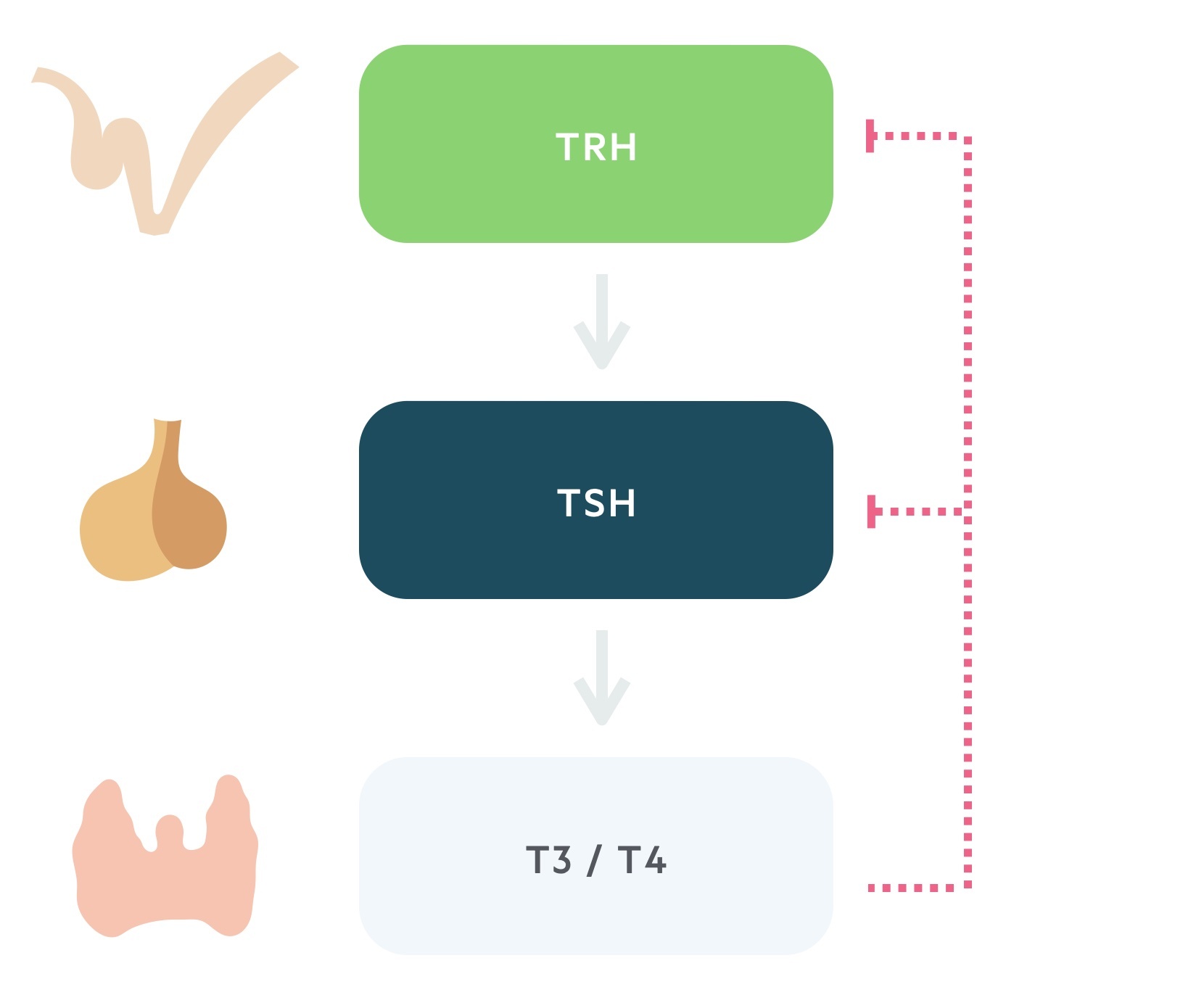
1. Thyrotropin releasing hormone
TRH is secreted from the paraventricular nucleus of the hypothalamus. As the name suggests it is a tropic hormone i.e one that acts upon another endocrine gland.
It reaches the anterior pituitary via the hypophyseal portal system. Here it causes the release of thyroid stimulating hormone.
2. Thyroid stimulating hormone
TSH, produced by the thyrotrophs of the anterior pituitary, is released following stimulation by TRH.
Transported in the blood, TSH acts upon the thyroid gland promoting the synthesis and release of thyroid hormone.
3. Triiodothyronine and thyroxine
The thyroid is stimulated to synthesise and release thyroid hormone by TSH. The thyroid produces two hormones, thyroxine (T4) and triiodothyronine (T3).
These thyroid hormones complete a negative feedback loop through the suppression of TRH and TSH release.
Though T3 is more biologically active than its counterpart T4, secreted thyroid hormone is 90% T4. Peripherally much of T4 is converted to T3.
Both are highly lipophilic, act on intracellular receptors and bind to thyroxine-binding globulin (TBG) in the blood. Only the ‘free pool’ is active: <0.1% T4 and <1% of T3.
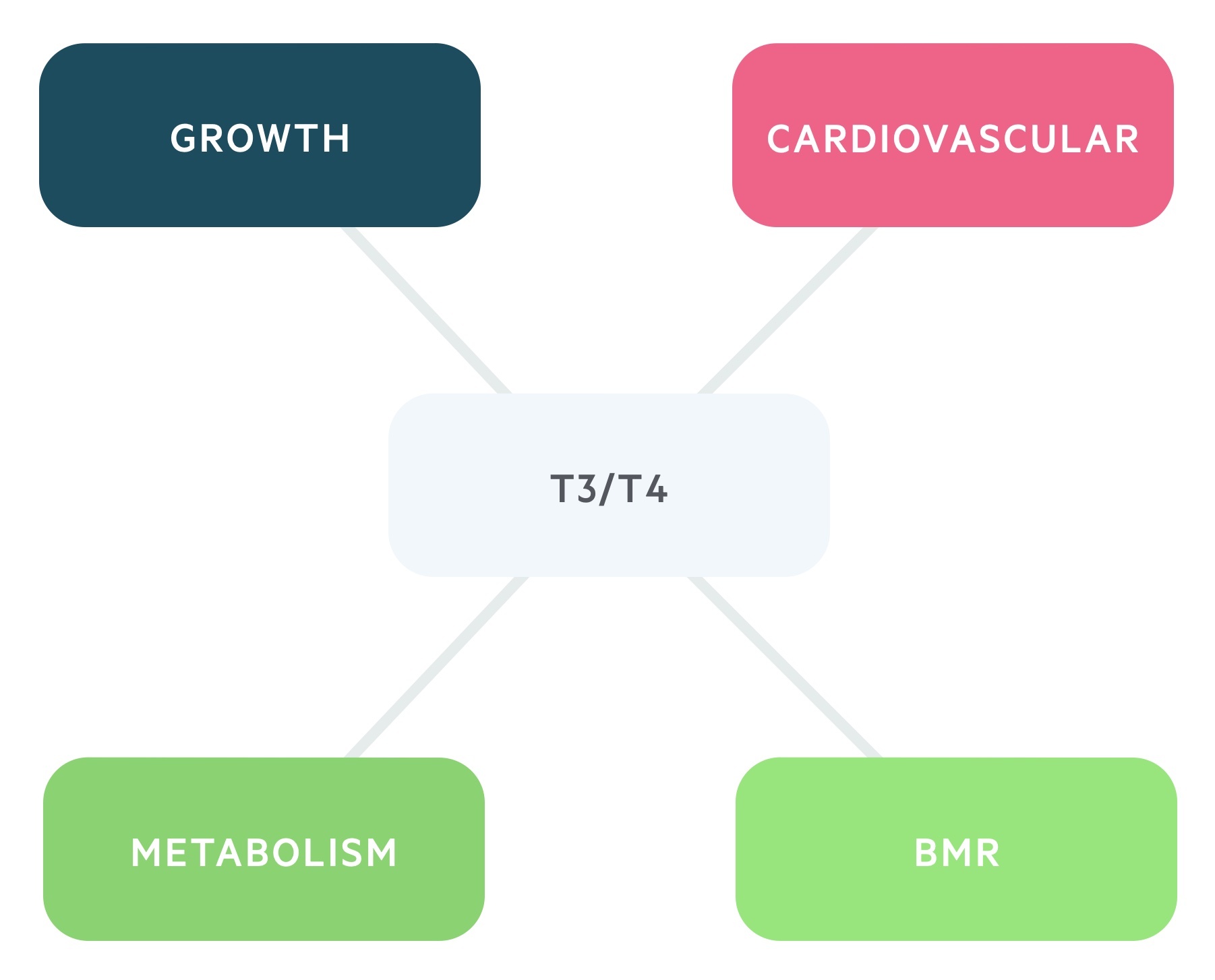
The effects to T3/T4 are numerous:
- BMR: increases the basal metabolic rate.
- Metabolism: it has anabolic effects at low serum levels and catabolic effects at higher levels.
- Growth: increases release and effect of GH and IGF-1.
- Cardiovascular: increases the heart rate and contractility through increasing sensitivity to catecholamines.
Thyroid hormone synthesis
Thyroid hormone has two constituents, tyrosine and iodine.
Background
Thyroid hormone is made with two basic building blocks:
- Tyrosine (amino acid) – synthesised by the body.
- Iodine – obtained in the diet and reduced to iodide before being absorbed in the small intestines.
These building blocks are assembled on the glycoprotein thyroglobulin (Tg) and synthesis occurs in the central colloid.
1. Preparation
Iodide enters the cell across the basolateral membrane via a sodium symporter. This process is driven by secondary active transport mediated by a Na+/K+-ATPase pump.
At the luminal membrane, iodide is activated by thyroperoxidase (TPO) before entering the colloid via the ion exchanger Pendrin.
Thyroglobulin, containing tyrosine, is produced by Golgi complexes and the endoplasmic reticulum in the follicular cells. The thyroglobulin/tyrosine complex is exocytosed across the luminal membrane into the colloid.
2. Synthesis
Within the colloid, one iodide may attach to a tyrosine (attached to a thyroglobulin) to form monoiodotyrosine (MIT). This reaction is catalysed by TPO. A second iodide may attach to MIT to form di-iodotyrosine (DIT).
Coupling of MIT and DIT yield the thyroid hormones. One MIT and one DIT gives triiodothyronine (T3) while two DITs give thyroxine (T4).
3. Release
When stimulated (by TSH) the surrounding follicular cells phagocytose a portion of the colloid. Once within the follicular cell, this vesicle is subject to lysosomes which act to release the T3/T4 from Tg.
The thyroid hormones T3/T4 may then diffuse into the blood stream. Any remaining MIT and DIT is deiodinated (a reaction catalysed by iodinase) and recycled.
Calcitonin
Calcitonin is produced by the parafollicular C cells.
Calcitonin release is stimulated by increases in serum calcium. It acts to lower calcium through its action on numerous tissues:
- Intestines: Reduces calcium absorption
- Bones: Stimulates osteoblasts, inhibits osteoclasts
- Kidneys: Inhibits phosphate reabsorption
It is not an essential hormone, following thyroidectomy no hormonal replacement of calcitonin is required.
It may be used therapeutically to treat hypercalcaemia and osteoporosis. Furthermore, it can be used as a marker of recurrence in medullary thyroid cancer.

