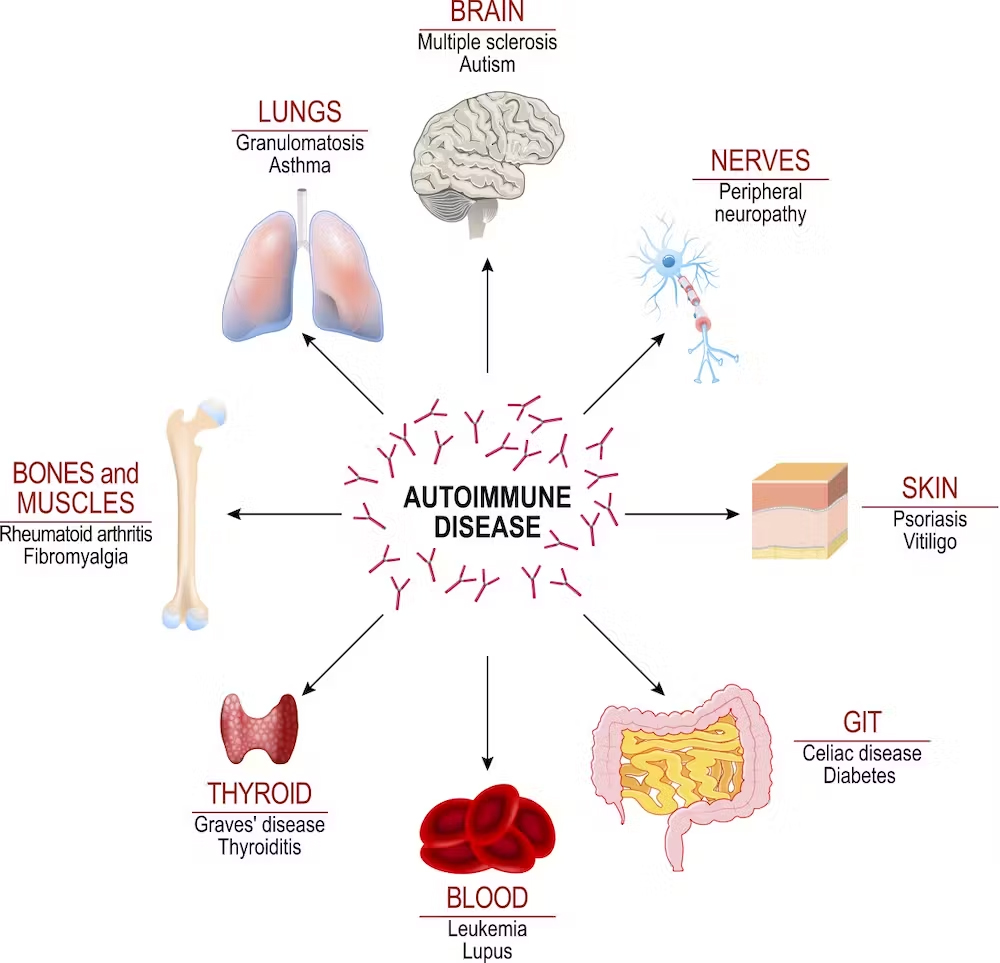
Bullous pemphigoid
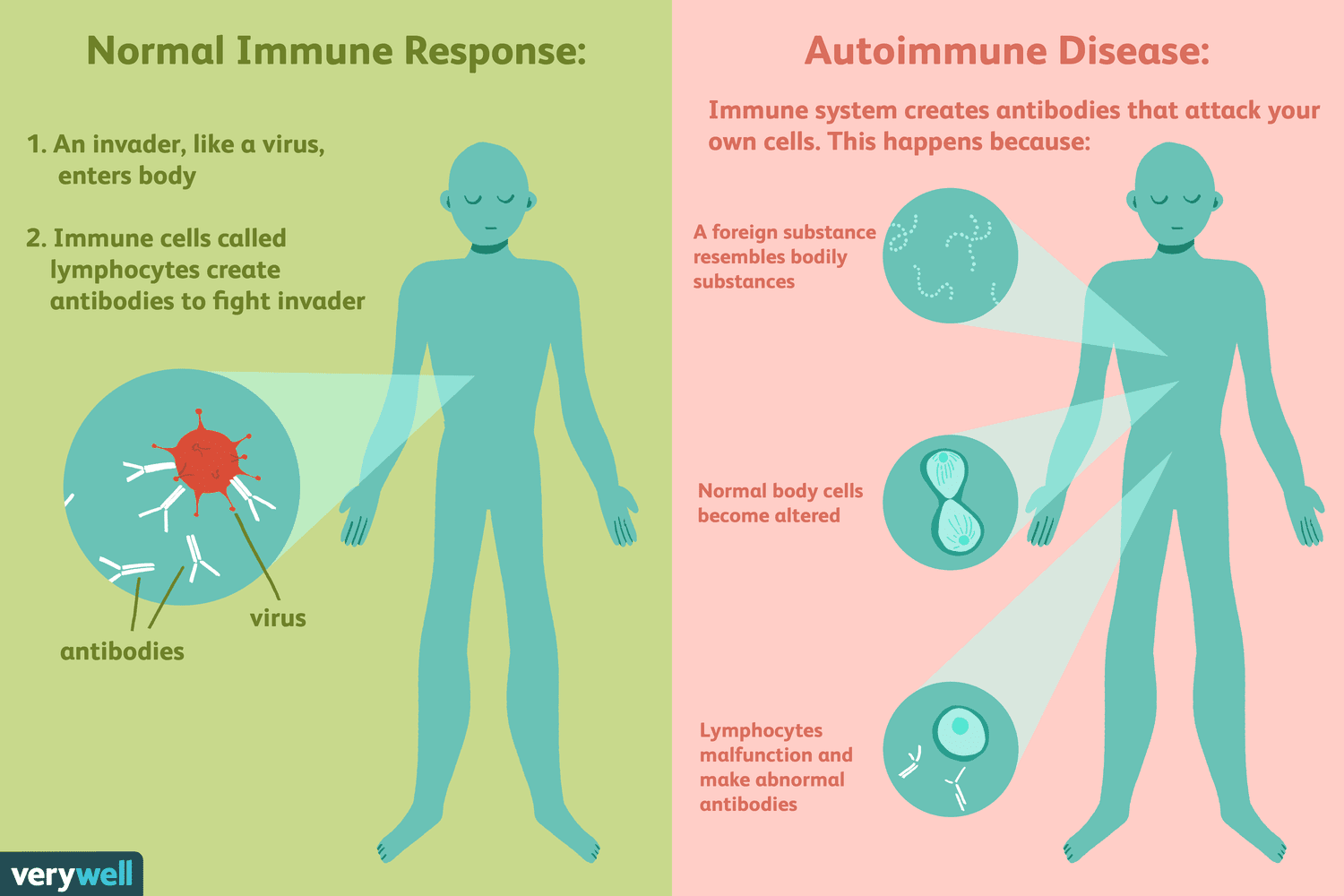
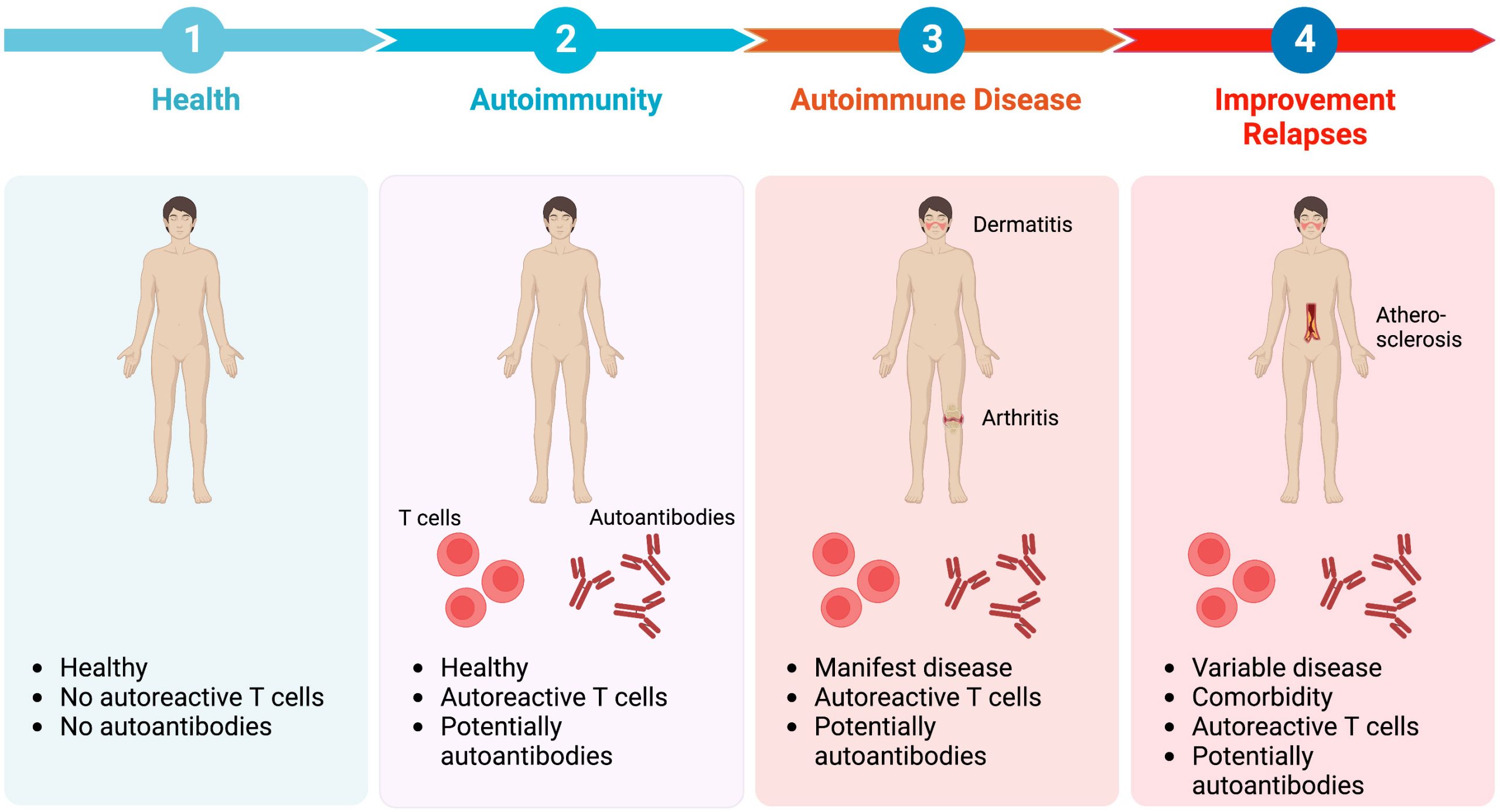
This is an autoimmune skin condition causing blisters under the epidermis.
– Due to a type II hypersensitivity reaction which gives destruction of hemi- desmosomes between basal cells and basal membrane.
– IgG antibody is directed against BP180 and BP 230 of basement membrane – More common in elderly patients >70 years but there is no obvious cause

Appearance
– Starts as a non-specific rash a month before the blisters
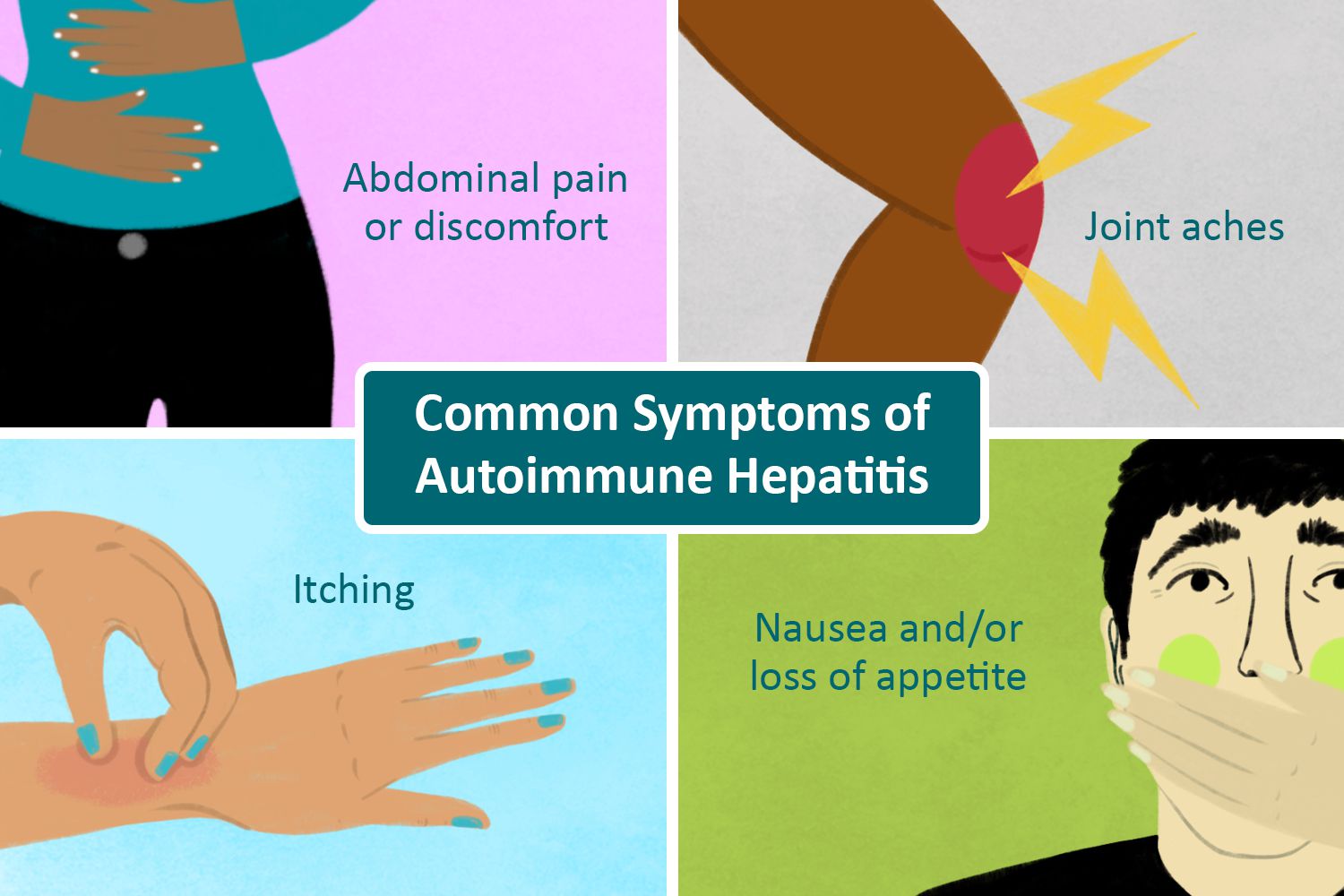
– Then itchy blisters form around the skin folds.
– Blisters are sup-epidermal and quite tense (do not rupture very easily) and heal without scarring – Blisters contains clear or cloudy yellowish fluid, but rarely affect the mouth/genital areas.
– Nikolsky sign negative
Tests – Skin biopsy –> Immunofluorescence staining shows IgG antibodies between the epidermis and dermis
Management – Corticosteroids to reduce blisters –> followed by immunosuppressants to wean off steroids
Pemphigus Vulgaris
This is an autoimmune condition, which leads to the formation of superficial blisters
– It is classically seen in the Ashkenazi Jewish population, aged between 30-60
– Due to IgG autoantibodies against desmoglein 3, an epithelial cell adhesion molecule which is found in desmosomes which are found near the bottom of the epidermis
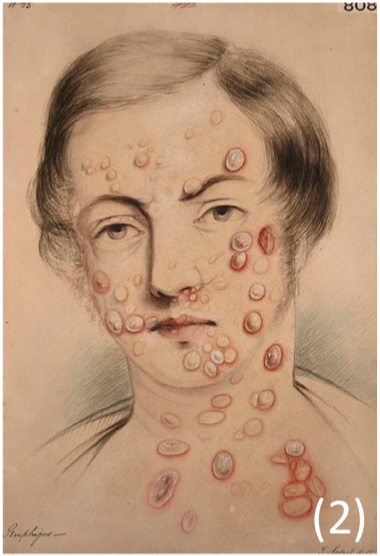
Appearance
– Starts with mucosal ulceration (very common)
– Later you get thin walled, flaccid blisters that easily rupture and painful and are slow-healing – Nikolsky sign positive (epidermal separation following horizontal pressure on skin)
Diagnosis – Skin biopsy –> Immunofluorescence staining shows IgG antibodies or complement on keratinocytes
Management – Systemic corticosteroids to induce remission –> then move to azathioprine/mycophenolate
Alopecia Areata
This is a chronic inflammatory condition which leads to patches on hair loss on the scalp usually, but can also affect the beard, eyebrows and eyelashes.
– Thought to be an autoimmune mediated reaction which occurs due to a breach in the immune privilege of the hair follicles
– Hair loss is usually patchy whereas total loss of scalp hair is more rare
– However, the prognosis is good, and hair regrows in most patients after a year

Management – If hair loss is <50%, try watchful waiting
– If hair loss >50% try potent topical corticosteroids –> decreases inflammation levels
– If severe refer to dermatology for specialist treatment e.g. minoxidil, immunotherapy
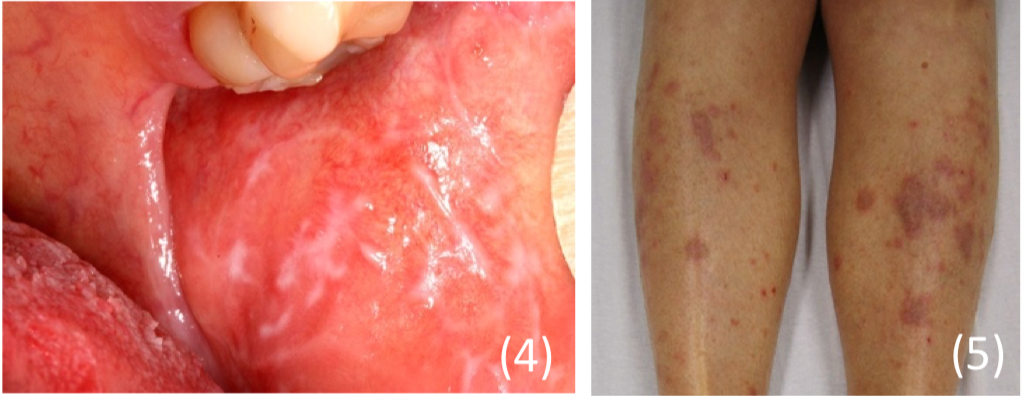
Lichen planus
A common, pruritic rash seen in adults, thought to be autoimmune.
– Results in a very itchy rash most commonly found on the wrists, ankles and the lumbar region, but can be widespread.
– Can also be caused by graft vs host disease, and drugs like thiazide diuretics and quinine
Appearance:
– Itchy planar, polygonal, purple papules (no fluid)
– Often has white reticular lines on surface (Wickham striae)
– Half of patients have involvement of the mouth, especially on the buccal mucosa with a white lacework pattern. – Lesions also are seen on the female genitalia, the penis and the nails
– Lesions demonstrate Koebner phenomenon –> where new lesions appear at the site of minor injury
Management:
– No cure is possible, but with treatment, half of patients clear by 9 months
– Skin disease –> Potent topical steroids
– Oral disease –> Topical analgesia as a mouthwash (Difflam)