Definition & classification
Hypertension refers to a persistent elevation of arterial blood pressure.
Prevalence is 30% in the UK (defined as adults with BP >140/90 mmHg). It is higher in men than in women before 60 years of age, but equal after this point.
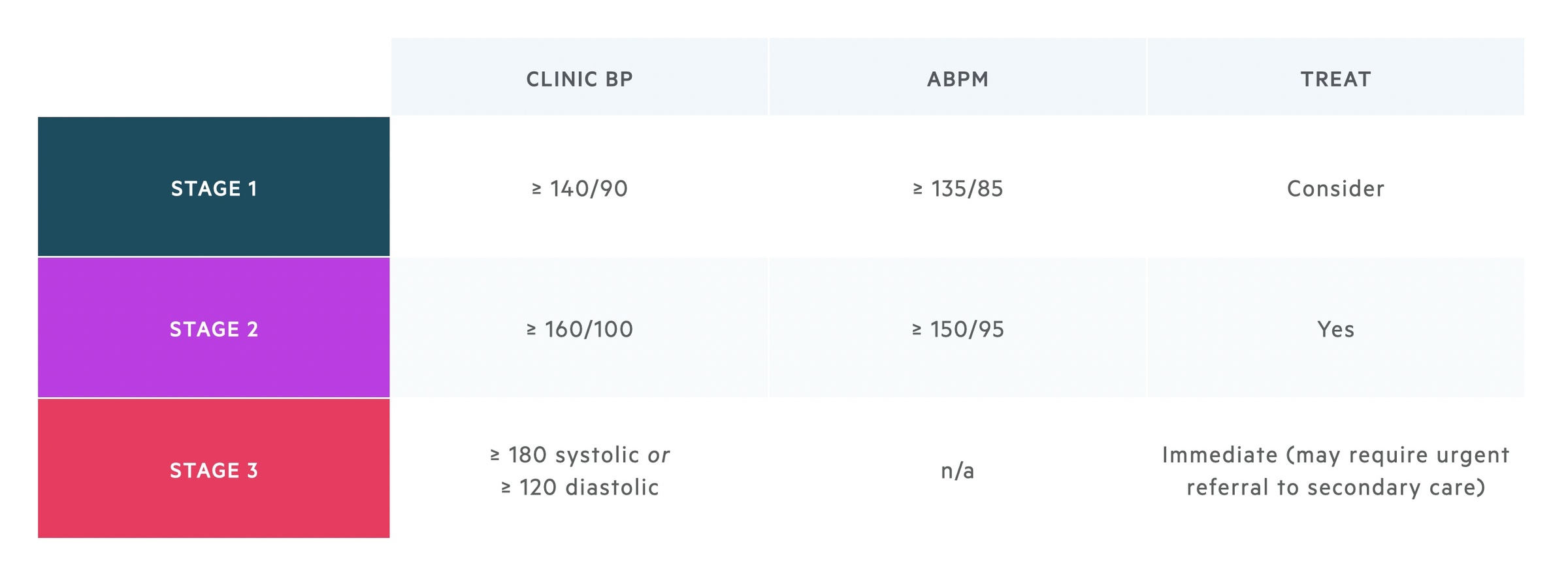
Hypertension is a major risk factor for myocardial infarction (MI), stroke and chronic kidney disease (CKD). It is classified into ‘stages’ to help guide management (Based on NICE NG 136 Hypertension guidelines).
Aetiology
The majority of hypertension is essential (primary), however in a significant number of cases there may be a secondary cause or contributory factor.
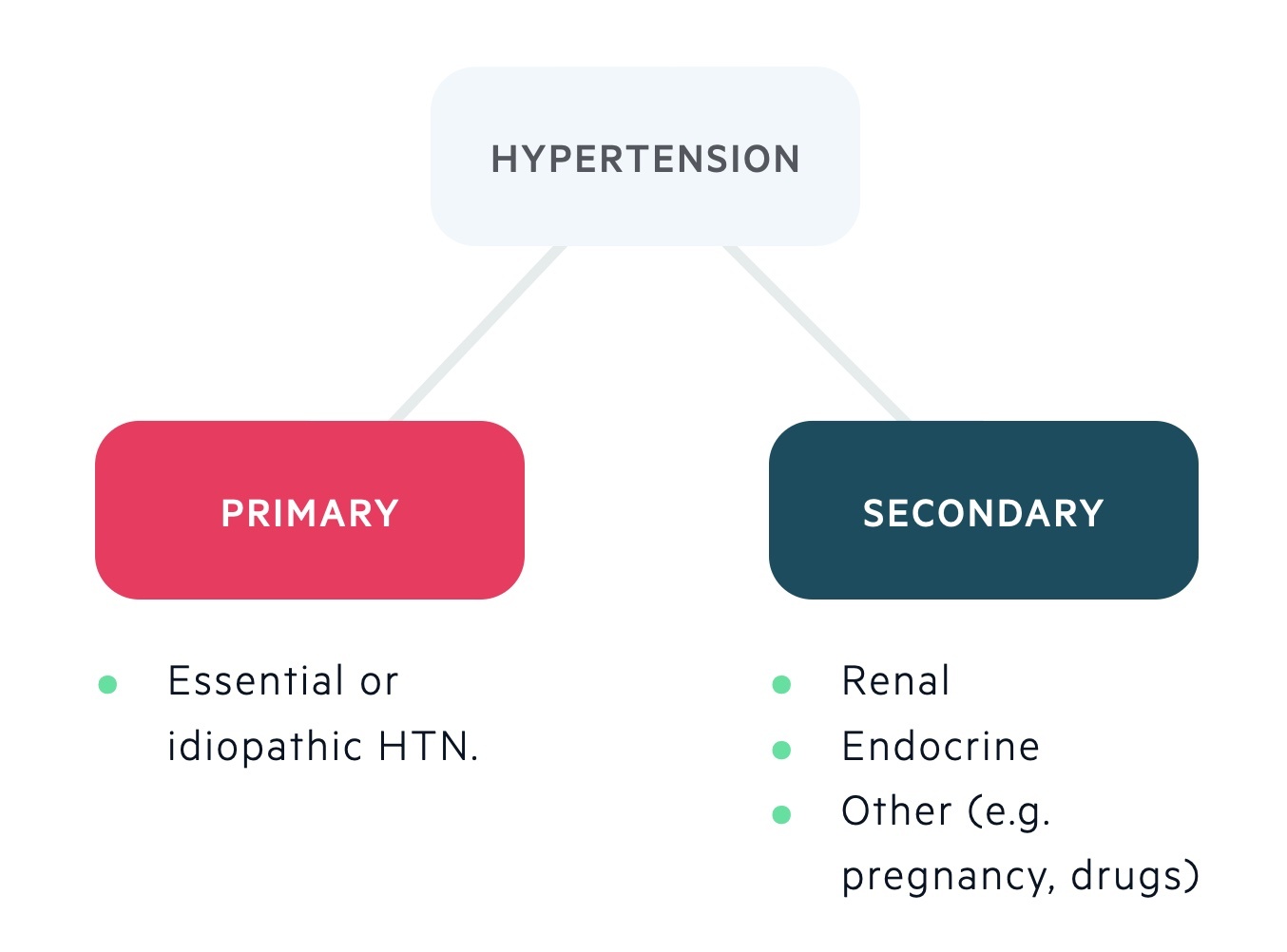
Primary – 95%
- No identifiable underlying cause.
Secondary – 5%
- Endocrine:
- Primary aldosteronism (increasingly recognised as a major cause of hypertension, see notes )
- Phaeochromocytoma
- Cushing’s syndrome (see notes)
- Acromegaly (see notes)
- Renal
- Renovascular disease (e.g. atheromatous, fibromuscular dysplasia)
- Intrinsic renal disease (e.g. CKD, AKI, glomerulonephritis)
- Drugs
- Glucocorticoids
- Oral contraceptives
- SSRIs
- NSAIDs
- EPO
- Coarctation of the aorta (consider in children / young adults with hypertension).
NOTE: This is an evolving area. It is now thought that a greater proportion of cases of hypertension have a secondary cause. Some studies indicate primary aldosteronism is responsible for 5-15% of cases of hypertension.
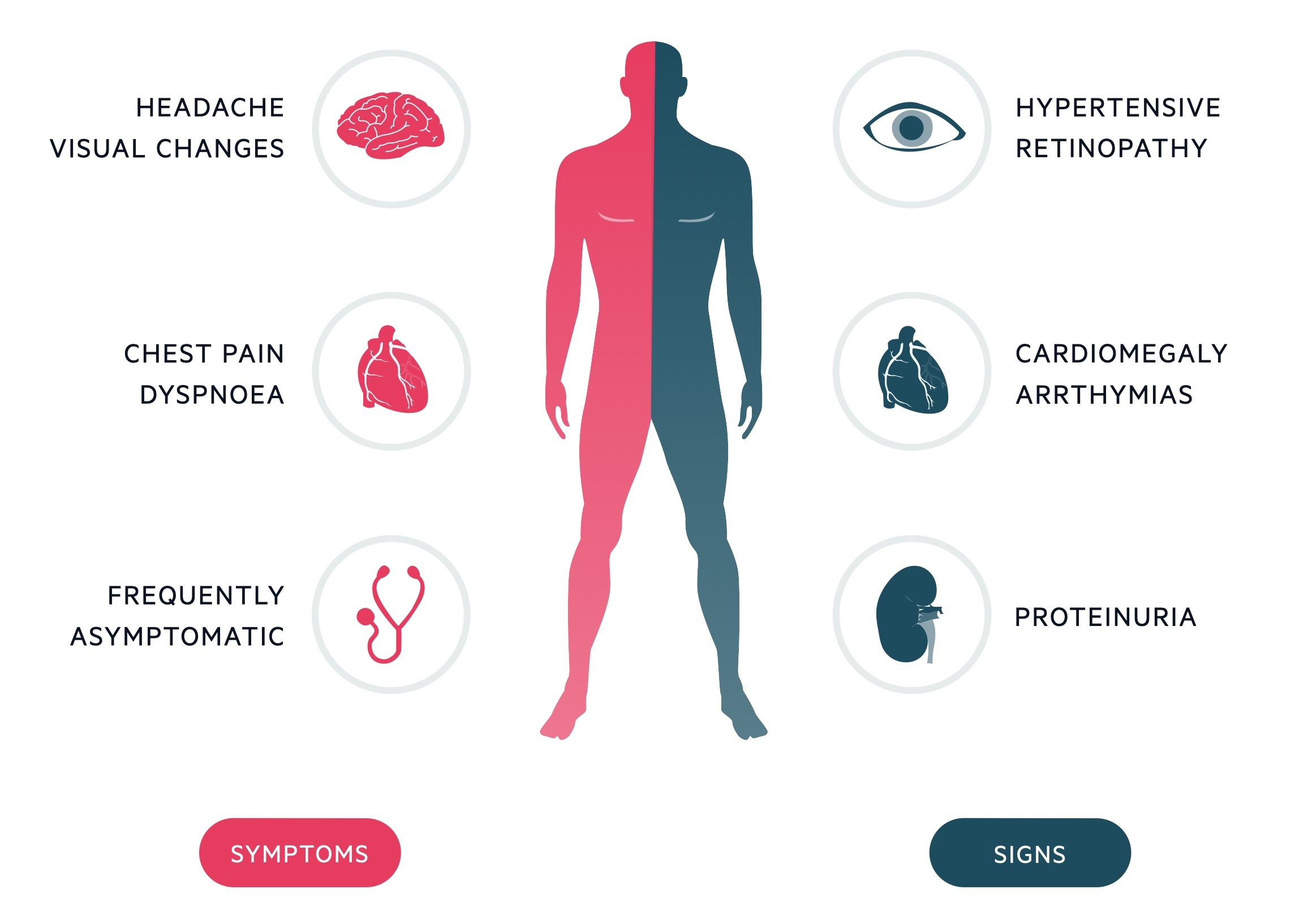
Clinical features
Hypertension is typically asymptomatic. However, signs and symptoms may reflect underlying end-organ damage or a potential secondary cause.
Symptoms
- Palpitations
- Angina
- Headaches
- Blurred vision
- New neurology (e.g. limb weakness, paraesthesia)
Signs
- New neurology (e.g. limb weakness, paraesthesia)
- Retinopathy
- Cardiomegaly
- Arrhythmias
- Proteinuria
Hypertensive retinopathy
Hypertension may cause progressive retinal microvascular changes.
These changes have been classified by the Keith-Wagener Barker (KWB) grades:
- Grade 1: Generalised arteriolar narrowing (silver wiring).
- Grade 2: Focal narrowing and arteriovenous nipping.
- Grade 3: Retinal haemorrhages, cotton wool spots (retinal nerve fibre layer micro-infarcts leading to exudation of axoplasmic materials).
- Grade 4: Papilloedema
Recently there has been a move away from the KWB grades with a new three stage system proposed.
Investigations
It is important to consider investigations for secondary causes in some individuals.
In the following patients underlying causes should be thoroughly excluded:
- Age < 40 years
- Reduced eGFR (suggestive of renal disease)
- Proteinuria or haematuria (suggestive of renal disease)
- Hypokalaemia and hypernatraemia (suggestive of Conn’s syndrome)
- Hypertension that is sudden onset, variable or worsening.
Bedside
- Observations
- Blood pressure
- Urinalysis
- Urinary protein creatinine ratio (uPCR)
- ECG
- Direct ophthalmoscopy
Bloods
- FBC
- U&Es
- Fasting glucose
- Cholesterol (CVS risk)
- HbA1c
Special tests
- Ambulatory BP monitoring (ABPM or HBPM)
- Renal USS
- Endocrine tests (e.g. aldosterone: renin ratio, if indicated)
Diagnosis
NICE now recommends the use of ambulatory BP measurements (ABPM) for the diagnosis of Stage 1 & 2 hypertension.
If clinic BP is 140/90 mmHg or higher, ABPM is used to confirm the diagnosis (except in Stage 3 hypertension, in which immediate treatment is initiated). With ABPM, at least two measurements an hour are taken during the patient’s usual waking hours (e.g. 8 am – 10 pm). The average value of these measurements is used to confirm the diagnosis. Alternative strategies can be considered including doing a full 24-hour assessment that includes nocturnal readings.
Alternatively, home blood pressure monitoring (HBPM) can be used. This involves taking two measurements a day (morning & evening) over a period of at least 4 days, ideally 7. At each recording, two consecutive measurements should be taken at least 1 minute apart when the person is seated. The readings on the first day are discarded and the average of the following readings are used to confirm a diagnosis of hypertension.
Stage 1
- ABPM ≥ 135/85, or
- Clinic BP ≥ 140/90 (must be confirmed by ABPM)
Stage 2
- ABPM ≥ 150/95, or
- Clinic BP ≥ 160/100 (must be confirmed by ABPM)
Stage 3
- Clinic BP ≥ 180/120
White coat hypertension
This refers to an elevated blood pressure above the normal range in a clinical setting (e.g. GP appointment, hospital outpatients). It is defined as a discrepancy of > 20/10 mmHg between clinic and average ABPM/HBPM
In white coat hypertension, blood pressure is thought to be artificially elevated due to the stress of being in a clinical setting. Patients with suspected white coat hypertension should have ABPM monitoring prior to a diagnosis of hypertension, unless blood pressure is dangerously elevated (i.e. stage 3).
Management
Management of hypertension is based upon NICE guidelines.
Modifiable risk factors
Lifestyle modification & patient education are important in treating hypertension.
- Offer advice that targets the patient’s modifiable risk factors.
- Discourage excessive caffeine and alcohol, if appropriate offer smoking cessation advice.
- Consider the need for anti-platelets or a statin.
Whom to treat
If clinic BP < 140/90 mmHg or ABPM < 135/85 mmHg, check BP at least every 5 years or more often if clinic BP close to 140/90 mmHg. If evidence of end-organ damage, consider other causes.
Antihypertensive drug therapy is initiated in patients:
- Aged < 80 years with stage 1 hypertension and with one of the following; end organ damage, cardiovascular disease, renal disease, diabetes or 10-year cardiovascular risk ≥10%.
- of any age with stage 2 hypertension
- of any age with stage 3 hypertension (consider immediate treatment)
Consider treatment in patients > 80 years old with stage 1 hypertension if clinic BP is > 150/90 mmHg. However, take into account frailty and co-morbidities. Patients < 60 years with stage 1 hypertension can be considered for antihypertensive therapy even if the 10-year cardiovascular risk < 10%.
Specialist assessment
Patients with stage 3 hypertension (≥ 180/120 mmHg) should be referred for same-day specialist assessment if any features of accelerated hypertension are identified:
- New onset confusion
- Chest pain
- Signs of heart failure (e.g. shortness of breath, fluid overload)
- Acute kidney injury
- Papilloedema
- Retinal haemorrhage
In addition, any patient with suspected phaeochromocytoma needs same day assessment. If none of these features are present, patients should be urgently assessed for end-organ damage. If present, treatment should be considered immediately before ABPM/HBPM. If absent, blood pressure should be reviewed within 7 days in clinic.
Any patient aged < 40 years should be considered for specialist assessment to exclude a secondary cause of hypertension.
Medical therapy
Hypertension is managed in a step-wise fashion. If blood pressure is not controlled with each step, medication should be reviewed to ensure that the treatment is optimal before moving onto the next step.
For patients aged > 80 years, offer the same anti-hypertensive therapies as for people aged 55-80 years, however take into consideration comorbidities.
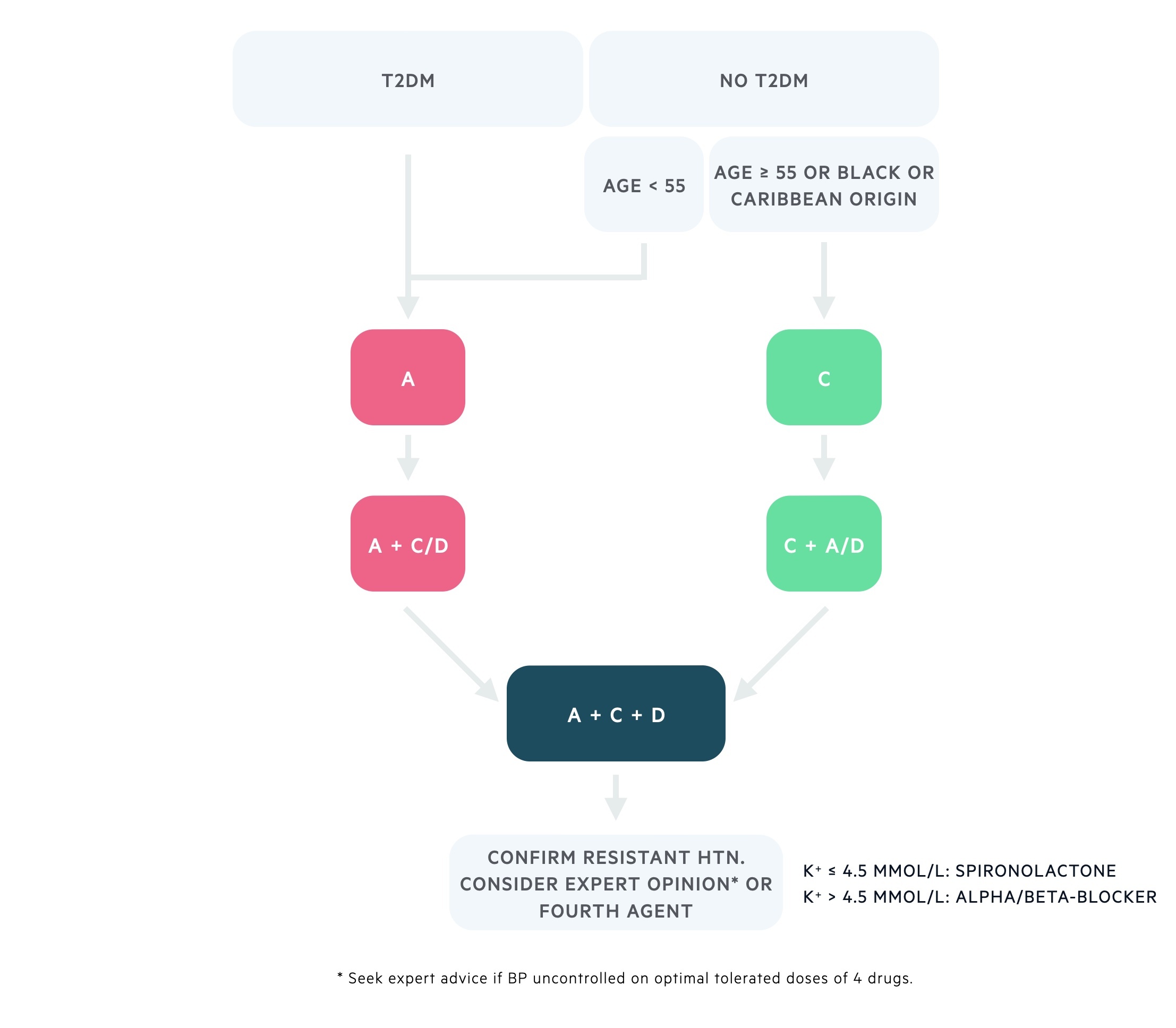
A = ACE-inhibitor / Angiotensin receptor blocker (ARB)
C = Calcium channel blocker (CCB)
D = Thiazide-like diuretic
T2DM = Type 2 diabetes mellitus
NOTE: if patients do not tolerate an ACE-inhibitor (e.g. dry cough), offer an ARB. A combination of ACE-inhibitor and ARB should NOT be used to manage hypertension.
Blood pressure targets
- Patients < 80 years: clinic BP < 140/90 mmHg / ABPM < 135/85 mmHg
- Patients ≥ 80 years: clinic BP < 150/90 mmHg / ABPM < 145/85 mmHg
For management of blood pressure in chronic kidney disease (CKD). See the NICE guidelines on CKD.
Hypertensive emergencies
Hypertensive emergencies occur when high BP results in acute end-organ damage.
The term malignant (or accelerated) hypertension is typically reserved for when papilloedema is present and is defined by NICE as:
A BP >180/120 with signs of papilloedema and/or retinal haemorrhage.
It is a severe condition resulting in neurological, renal and cardiac damage, requiring admission and immediate management.
Treatment attempts to reduce BP over 24-48hrs. This is to prevent hypoperfusion. Changes may have occurred to autoregulatory mechanisms of blood pressure control. Therefore, a rapid reduction in blood pressure, even to normal levels, may result in profound organ hypoperfusion.
Therapies include:
- IV Nitroprusside (a nitric oxide releasing drug), labetalol and glyceryl trinitrate infusions are options.
- Phentolamine (alpha-adrenergic antagonist) also used in phaeochromocytoma crisis.

