Introduction
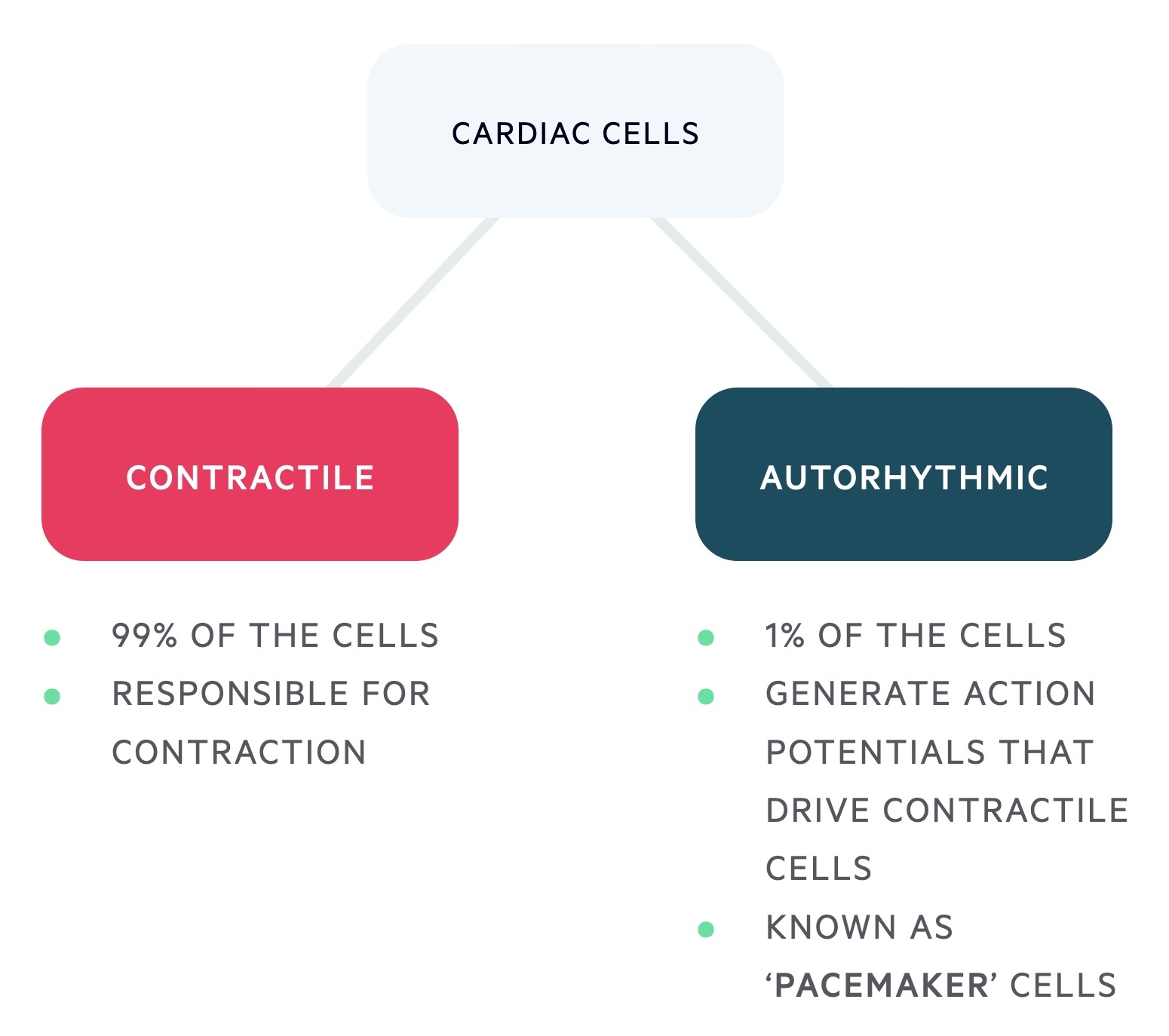
The heart is able to beat independently, devoid of nervous input. This is achieved through special ‘pacemaker’ cells.
Myocardial contraction is dependent on two cell types:
- Autorhythmic cells (1%):
- Generate action potentials that drive contractile cells.
- Do not have a resting potential, instead, they slowly depolarise, hence ‘pacemaker cells’.
- Contractile cells (99%):
- Responsible for myocardial contraction.
- Able to undergo rapid depolarisation, driven by the autorhythmic cells.
Conduction system
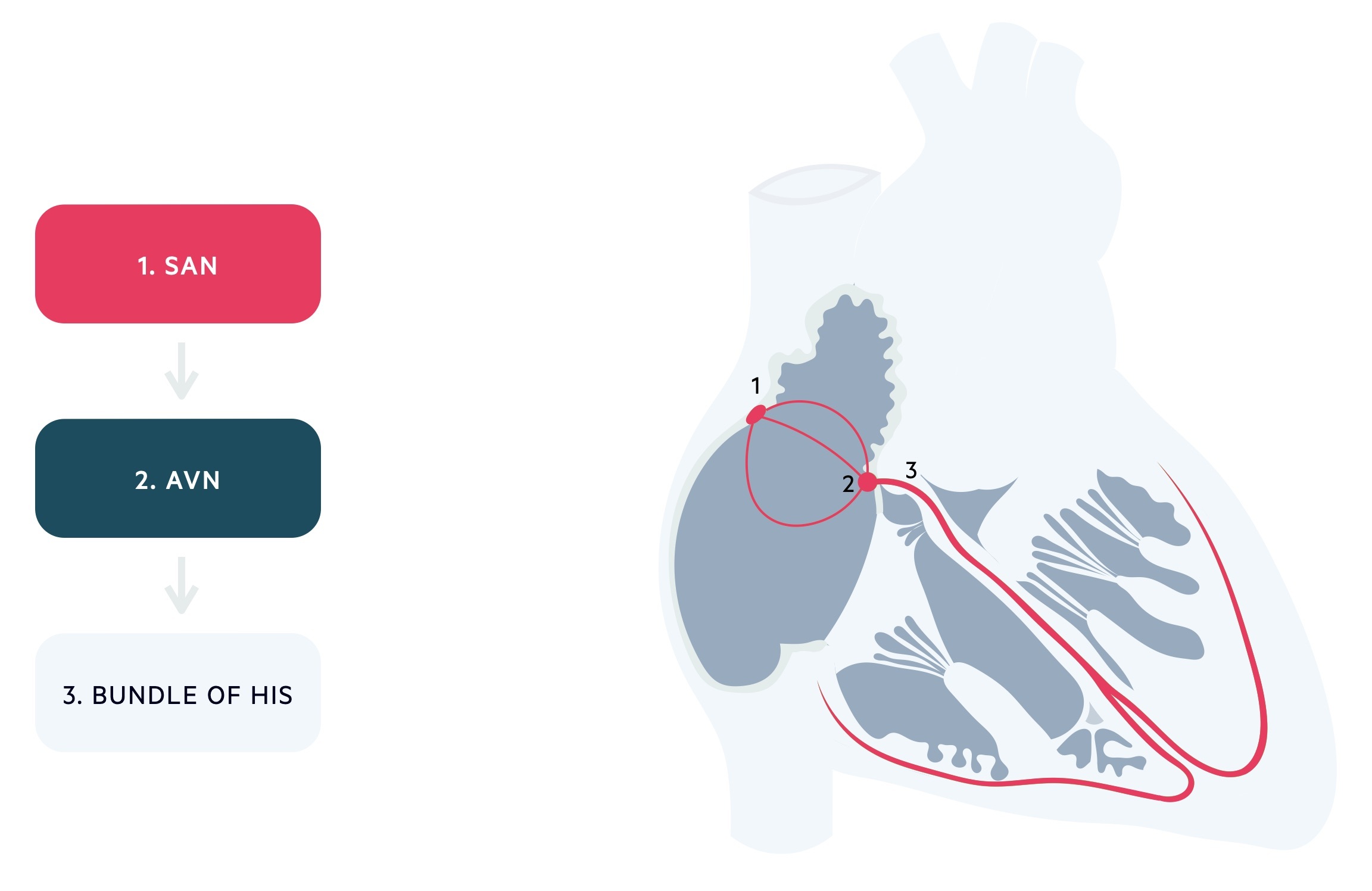
Conduction through the heart is dependent on pacemaker cells organised into key structures.
1. Sinoatrial node (SAN)
- Location: Spindle-shaped structure located at the junction of the superior vena cava (SVC) and right atrium.
- Function: The pacemaker of the heart. Spontaneous depolarisation occurs at a rate faster than other cardiac cells and as such it sets the pace (sinus rhythm).
- Rate of autorhythmicity: 70-80 bpm.
2. Atrioventricular node (AVN)
- Location: A bundle found near the septum at the base of the right atrium.
- Function: Receives pacemaker potential from SAN and conducts this to the ventricles via the bundle of His. It delays conduction (typically by 0.21 seconds) to allow completion of atrial contraction and ventricular filling.
- Rate of autorhythmicity: 40-60 bpm.
3. Bundle of His
- Location: Forms a tract from the AVN to the interventricular septum.
- Function: Spreads the action potential through the ventricle. Divides into the right and left bundle branches (of His) which terminate in the Purkinje fibres.
- Rate of autorhythmicity: 20-40 bpm.
Autorhythmic cells
Autorhythmic cells do not possess a resting potential, instead they slowly depolarise exhibiting pacemaker potential.
In these cells, the membrane potential slowly drifts until the threshold is reached. This is in contrast to most nerve and skeletal muscle cells, in which membrane potential remains constant unless the cell is stimulated. Through repeated cycles of drifting and firing, these cells rhythmically initiate action potentials.
The action potential of autorhythmic cells is divided into several phases:
Phase 4
‘Funny’ sodium channels (If) open allowing a slow inward flow of Na+ ions into the cell causing depolarisation. Transient (T-type) calcium channels (IcaT) open at -50mv, bringing the membrane closer to threshold.
Once the threshold is reached, long-lasting (L-type) voltage-gated calcium channels (IcaL) open.
Phase 0
The long-lasting (L-type) calcium channels remain open continuing depolarisation.
Phase 3
Outward potassium channels (Ik) open resulting in repolarisation.
Contractile cells
Contractile cells, unlike autorhythmic cells, have a resting potential. They typically require an impulse from another myocardial cell to depolarise.
The action potential of contractile cells is divided into several phases:
Phase 4
Unlike autorhythmic cells, the membrane of contractile cells remains essentially at rest at about -90 mV until excited. Leaky potassium channels (Ik) maintain the cell at resting potential through the outward movement of potassium ions.
Phase 0
Depolarisation occurs in an adjacent cell and the threshold potential is met. Fast voltage-gated sodium channels (INa) open and sodium ions enter the cell rapidly.
Phase 1
The first stage of repolarisation. Potassium ions leave the cell via transient K+ channels (Ikto).
Phase 2
Plateau phase. Inward movement of calcium ions via voltage-gated L-type channels (IcaL) prolongs repolarisation.
Phase 3
Completion of repolarisation. Outward movement of potassium ions (via Ik channels) returns the membrane to its resting potential.
Autonomic nervous system
The autonomic nervous system exerts a degree of control over the electrophysiology of the heart; vagal innervation (parasympathetic) tends to dominate sympathetic stimulus.
Parasympathetic nervous system
The vagus nerve supplies the atria, in particular, the SAN and AVN.
- SAN: stimulation results in enhanced potassium permeability with reduced frequency of action potentials.
- AVN: enhanced potassium permeability results in increased AV nodal delay.
- Contractile cells: shortens the plateau phase, reducing atrial contraction.
Sympathetic nervous system
Sympathetic fibres supply the atria, SAN, AVN, and ventricles.
- SAN: increased rate of depolarisation, increased frequency of action potentials.
- AVN: reduced AVN delay.
- Conduction pathway: faster spread of action potentials.
- Contractile cells: increased strength of contraction and quicker relaxation.
ECG
An electrocardiogram (ECG) is a recording of the hearts electrical activity.
A 12 lead ECG records from 10 electrodes but offers 12 ‘views’ the heart.
ECG waveforms
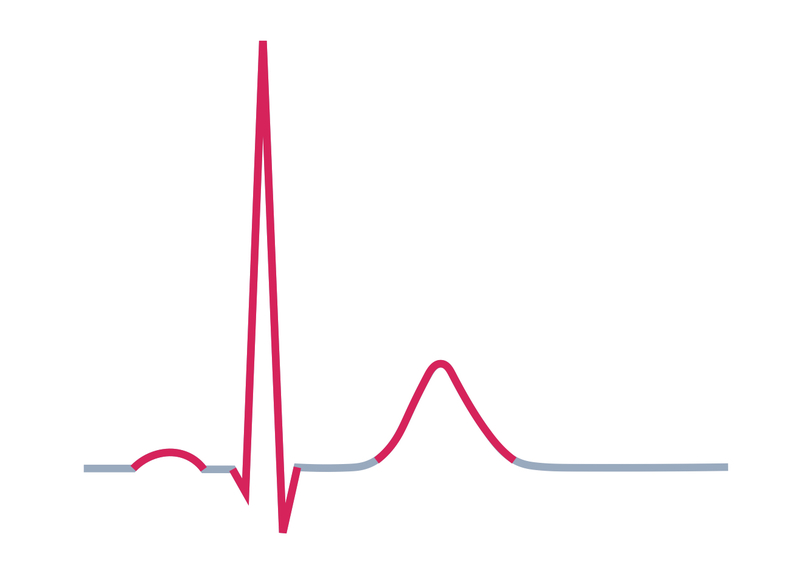
An ECG strip is made up of a baseline with deflections caused by movement of electrical impulses either toward (positive deflection) or away (negative deflection) from electrodes. The deflections that make up a normal ECG are termed waves and are assigned arbitrary letters.
A normal ECG waveform is composed of:
- P-waves: atrial depolarisation.
- QRS complexes: ventricular depolarisation. If first deflection is down it is a Q-wave, if the first deflection is up it is an R-wave.
- T-waves: ventricular repolarisation.
- U-waves: sometimes seen, origin disputed. May be pathological if follows abnormal T-wave.
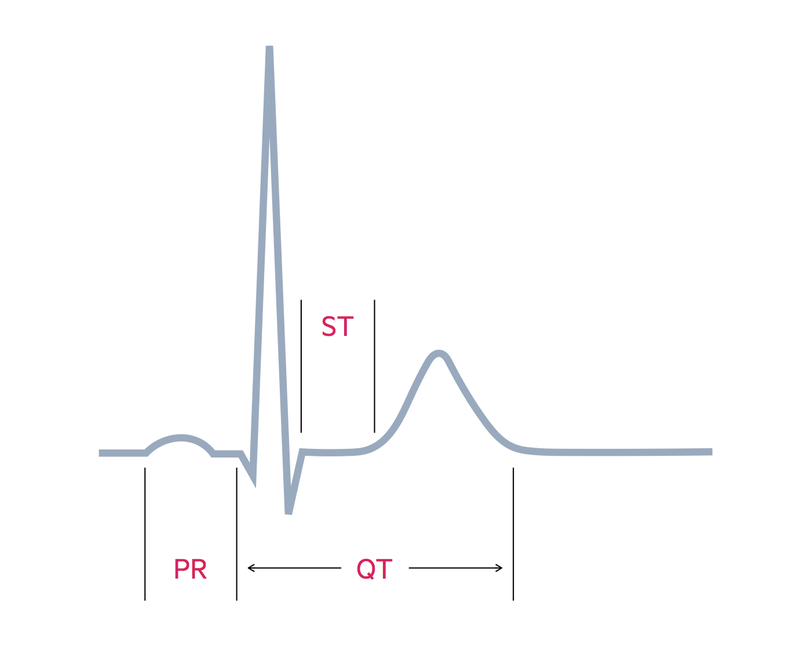
The ECG may be deconstructed into additional key components:
- PR-interval: time taken for the electrical impulse to travel between the atria and ventricles.
- QRS complex: duration of ventricular depolarisation.
- ST-segment: changes generally seen in myocardial ischaemia / infarction.
- QT-interval: varies with heart rate, long QT has many causes but may predispose to polymorphic ventricular tachycardia.
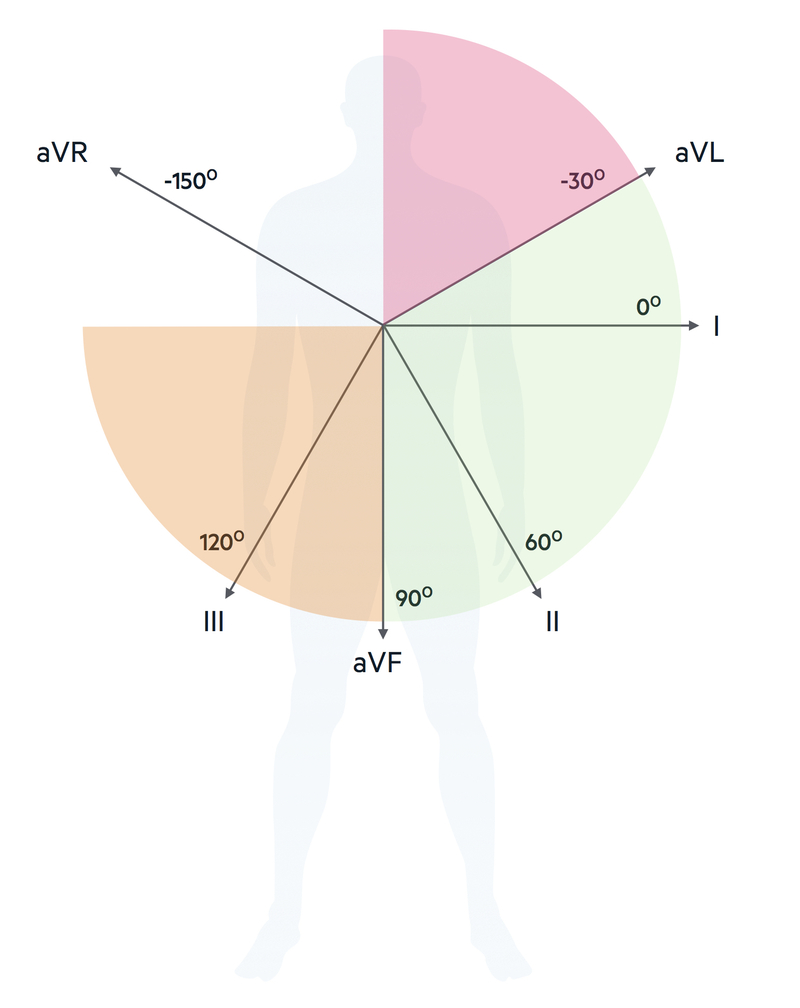
Cardiac axis
The cardiac axis refers to the net effect of all of the action potentials that are generated.
A normal axis is said to lie between -30° and 90°. If conduction is delayed in one direction or one side exerts greater electrical influence, the axis may be deviated to either the left or right.
Left axis deviation (LAD) may be caused by:
- Left anterior fascicular block
- Left ventricular hypertrophy (rarely, only if severe disease)
Right axis deviation (RAD) may be caused by:
- Left posterior fascicular block (uncommon)
- Right ventricular hypertrophy
- Pulmonary embolism
Isolated left or right bundle branch block has little effect on the axis.
Cardiac cycle
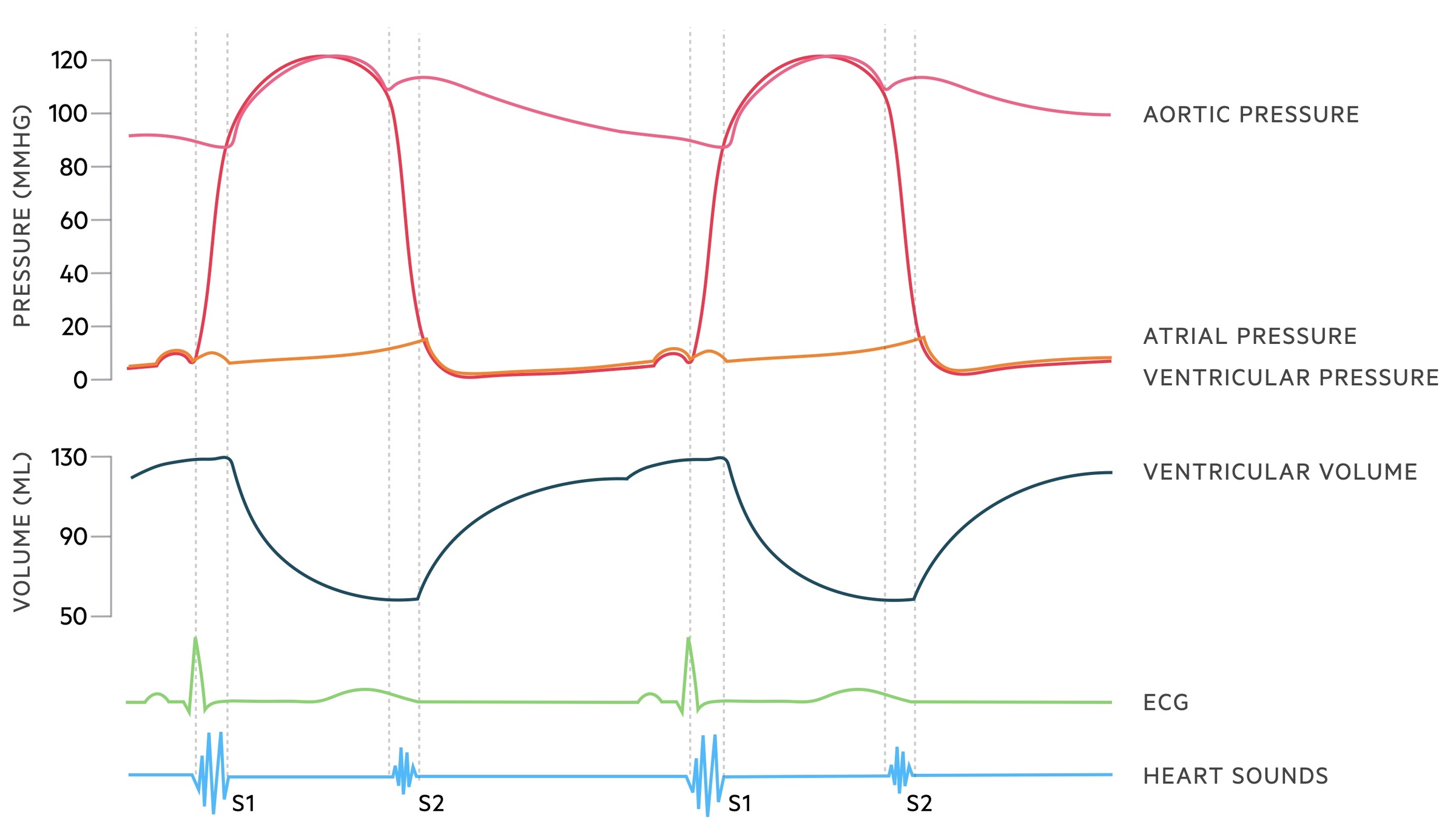
Wigger’s diagram illustrates the entirety of the cardiac cycle; it describes the precise relationship between electrical and mechanical activity.
Electrical activity is initiated at the SAN. This sends a wave of excitation across the atria towards the AVN (observed as a p wave on the ECG). This wave of excitation leads to contraction of the atria, which forces blood into the ventricles.
The AVN then continues the wave of excitation throughout the ventricles via the conduction system. This wave of excitation leads to contraction of the ventricles (QRS complex on the ECG). The onset of contraction marks the start of systole.
The ventricles contract leading to the closure of the mitral and tricuspid valves, which generates the first heart sound (S1). As pressure increases the volume within the ventricles stays the same. This is termed isovolumetric contraction. Eventually, the pressure within the ventricles overcomes the pressure within the aortic and pulmonary vessels. This leads to blood being forced out of the ventricles and into the systemic and pulmonary circulation.
As blood leaves the ventricle the volume decreases but the pressure within the aorta (120 mmHg) and pulmonary trunk (30 mmHg) increases. At the end of contraction, the ventricles start to relax. The backflow of blood from the aortic and pulmonary vessels leads to closure of the aortic valve and pulmonary valves, which generates the second heart sound (S2). The rebound of blood off the aortic valve causes the dicrotic notch in the aortic pressure graph.
Initially, the pressure within the ventricles continues to fall without any change in volume. This is termed isovolumetric relaxation. Eventually, pressure within the ventricles falls below that of the atrial pressure and the atrioventricular valves open. This marks the onset of diastole.
The cycle then repeats itself.