Introduction
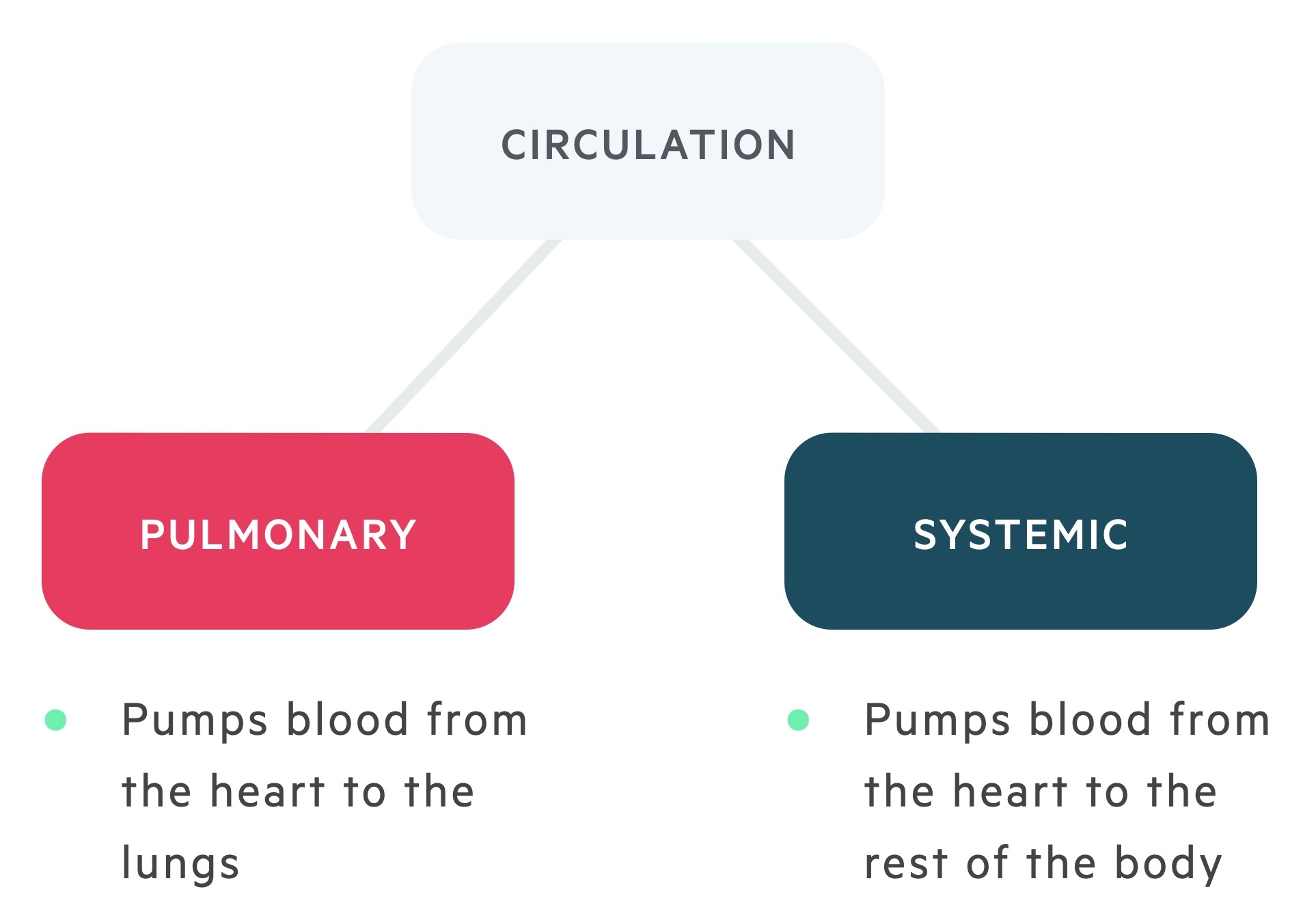
The cardiovascular system delivers blood to the body providing both oxygen and nutrients.
It is organised into two circuits, pulmonary and systemic.
The heart
The heart is a dual pump that sits at the centre of the cardiovascular system.
It is composed of four chambers:
- Two atria (left & right)
- Two ventricles (left & right)
Right side: blood is received from the body to be delivered to the lungs.
Left side: blood is received from the lungs to be delivered to the body.
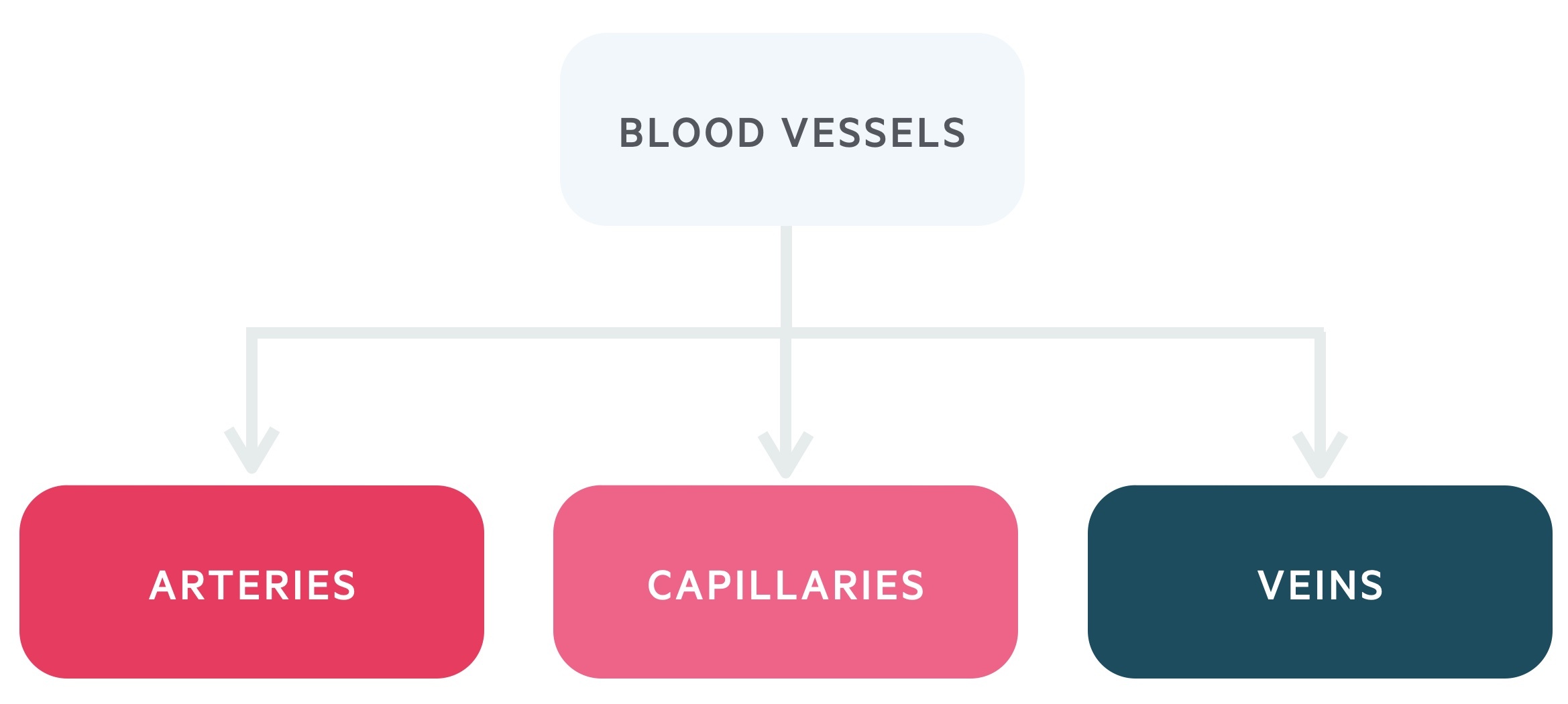
Blood vessels
The flow of blood is mediated by a network of vessels:
- Arteries – carry oxygenated blood away from the heart.
- Capillaries – form a microcirculation enabling nutrient and gaseous exchange to occur.
- Veins – carry deoxygenated blood back to the heart.
Capillary exchange
Capillaries are microscopic single-celled blood vessels that form networks around tissue where exchange of oxygen & nutrients occurs.
Capillaries are connections between the arterial and venous systems. In contrast to the plasma membrane of most cells, the capillary wall is relatively leaky. The extent of ‘leakiness’ varies between tissues; the liver is particularly permeable, whilst in the brain, free movement of solutes is considerably less.
Precapillary sphincters help to control and direct flow.
The exchange of substances between capillaries and extracellular fluids is achieved by two main mechanisms:
- Diffusion: net movement of solutes (e.g O2, CO2) down their respective concentration gradients due to the random motion of individual molecules.
- Bulk flow: movement of water and solutes together due to a pressure gradient (ultrafiltration).
- The capillary wall is semipermeable, fluid is pressured out via ultrafiltration, plasma proteins are retained.
- These pressures are described by the Starling equation.
The capillary wall permits free passage of water and solutes less than a particular size. As a consequence, small molecules achieve equal concentrations on both sides, and there is no net contribution to the effective osmotic pressure. Since larger plasma proteins cannot cross the capillary wall, they produce an effective osmotic pressure (oncotic pressure).
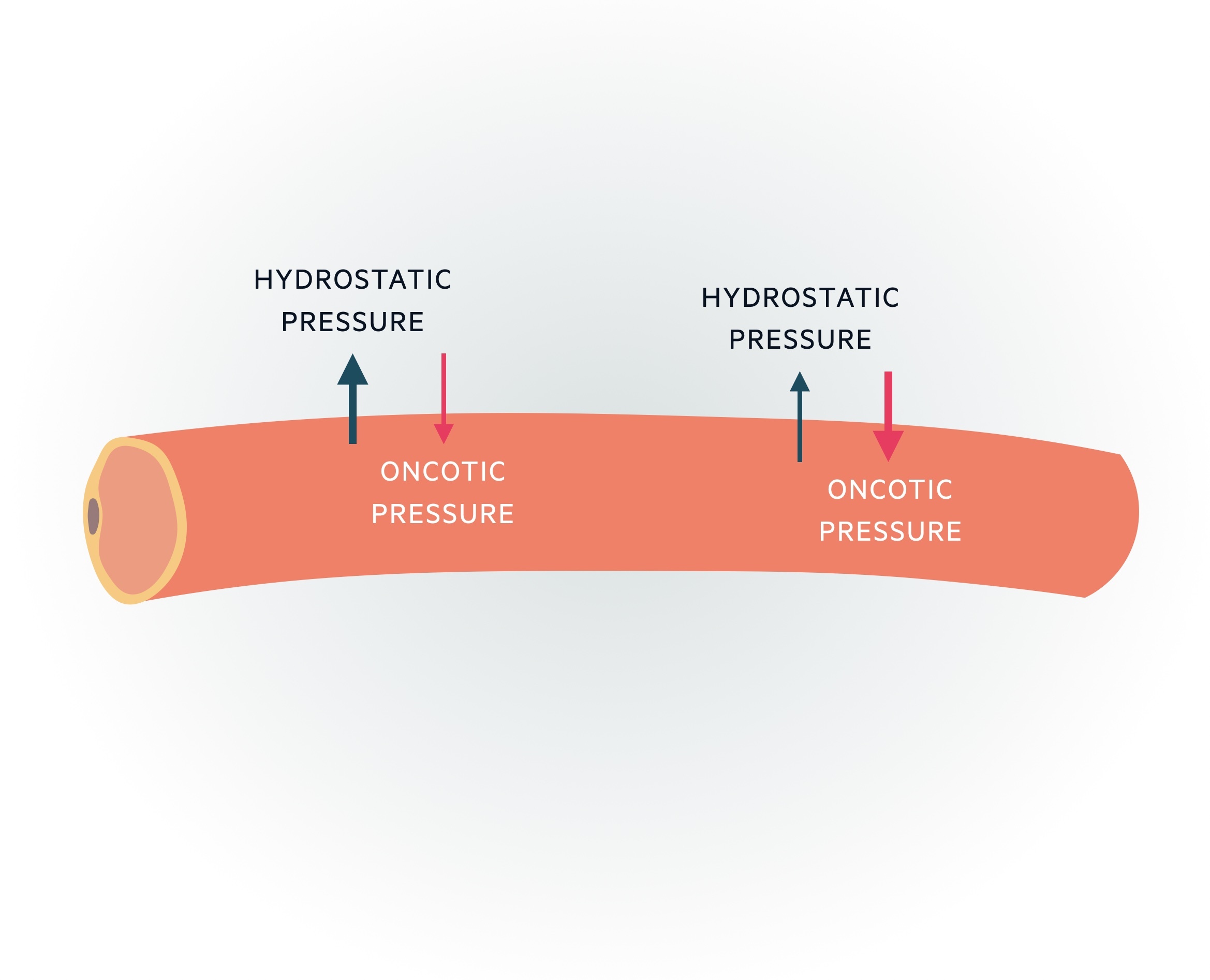
Hydrostatic pressure refers to the pressure that any fluid in a confined space exerts.
Starling’s equation
Describes the role of hydrostatic and oncotic forces in the movement of fluid across capillary membranes.
Starling’s equation was formulated in the 19th-century by the British physiologist Ernest Starling (also known for the Frank-Starling law of the heart).
Bulk flow is controlled by a number of factors termed ‘Starling’s forces’:
- Hydrostatic pressure:
- By the time blood reaches the arteriolar end of the capillary the pressure is around 37 mmHg.
- At the venous end, it drops to 17 mmHg.
- Oncotic pressure:
- This is the pull plasma proteins have, attracting fluid into the capillaries.
- Around 25 mmHg.
- Other factors (essentially have insignificant effects):
- Interstitial fluid hydrostatic pressure: the hydrostatic pressure of the interstitial fluids; a minor force that is around 1 mmHg.
- Interstitial fluid colloid osmotic pressure: the oncotic pressure of the interstitial fluid, insignificant force in health; may become significant if vasculature permeability increases.
Essentially, net pressure = hydrostatic pressure – oncotic pressure:
- Arteriolar end = 37 – 25 = 12 mmHg
- Venous end = 17 – 25 = – 8 mmHg
At the arteriolar end, this net difference results in ultrafiltration with fluid leaving the capillary. At the venular end, however, the hydrostatic pressure is much less and so the net difference results in reabsorption.
Interestingly, this apparent equilibrium is not total; slightly more fluid is lost into the interstitial space than is reabsorbed. This additional fluid is drained by the lymphatic system.
Haemodynamics
The vascular system delivers blood by a network of vessels, this process is regulated by the dynamics of fluid flow.
Blood flows in concentric streams, known as laminar flow. At higher velocity, laminar flow may become disrupted and turbulent.
Ohm’s law
Ohm’s law describes flow’s dependence on pressure gradient & resistance.
Flow through a vessel is dependent on the pressure difference at either end of the vessel (𝚫P) and the resistance to flow (R). Ohm’s law, which you may remember from physics, describes the relationship between these two variables. It states that
Flow (F) = 𝚫P/R.
Poiseuille’s law
Poiseuille’s law describes laminar flow of an incompressible liquid through a tube and determines that proportional to the fourth power of the pipe’s radius. These variables are: vessel radius (r), vessel length (L), viscosity (η) and pressure gradient (𝚫p)
Resistance (R) ∝ η x L / r4
Flow (F) ∝ 𝚫p x r4 / η x L
As described by the equation resistance is inversely proportional to r4, therefore small changes to a vessel diameter have significant implications for flow. If the radius were to be doubled the resistance would fall by sixteen times. In essence, flow through a vessel is proportional to the pressure exerted across it and the radius and inversely proportional to the length of the vessel and viscosity of fluid.
Cardiac output
Cardiac output is the volume of blood pumped out of the heart in one minute.
It can be calculated by multiplying the heart rate (HR) by the stroke volume (SV). SV is the volume of blood pumped out of the heart from each contraction.

The heart is responsible for maintaining adequate cardiac output through rate and stroke volume. With an average of 70 bpm and 70 ml per beat, cardiac output can be estimated at 5L / min.
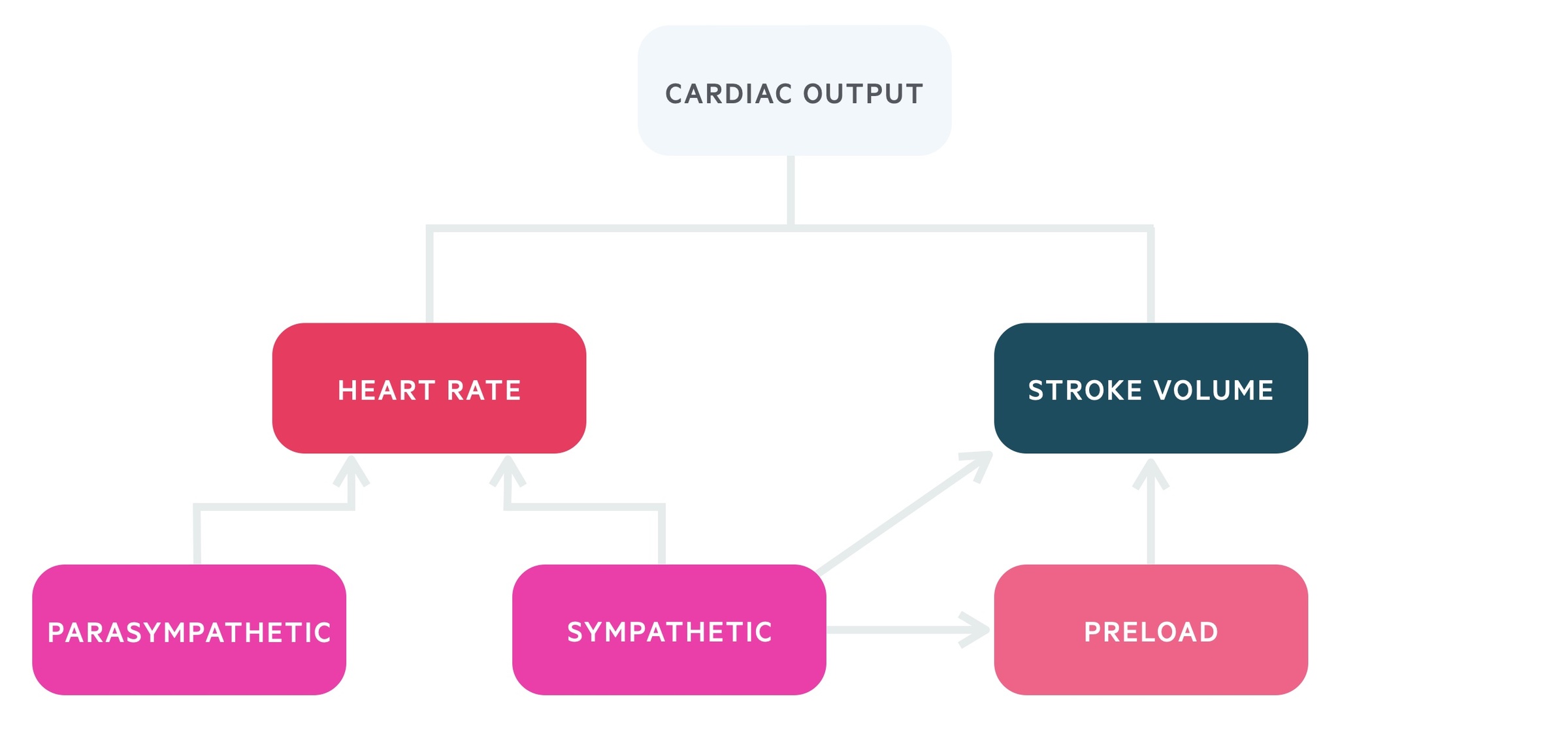
Heart rate
The heart rate is predominantly determined by the sympathetic nervous system and parasympathetic nervous system (autonomic nervous system).
Parasympathetic nervous system
Acts on the sinoatrial node (SAN), atrioventricular node (AVN) and contractile cells to reduce the heart rate.
- Innervation: via vagus nerve which supplies the atria, particularly the SAN and AVN.
- Actions:
- SAN: Enhanced K+ permeability, reduced frequency of action potentials.
- AVN: Enhanced K+ permeability increased AVN delay.
- Contractile cells: Shortens plateau phase, reducing the strength of atrial contraction.
Sympathetic nervous system
Acts on the SAN, AVN, conduction fibres and contractile cells to increase heart rate.
- Innervation: fibres that supply the atria, SAN, AVN, and ventricles.
- Actions:
- SAN: increased rate of depolarisation, increased frequency of action potentials.
- AVN: reduced AVN delay.
- Conduction pathway: faster spread of potentials.
- Contractile cells: increased strength of contraction and speed of relaxation.
Stroke volume
Stroke volume is determined by the sympathetic nervous system and the preload.
The primary determinants of stroke volume are:
- Preload – stretching of cardiomyocytes at the end of diastole.
- Myocardial contractility – changes to stroke volume can be brought about through changes to contractility.
- Afterload – pressure or load against which the ventricles must contract.
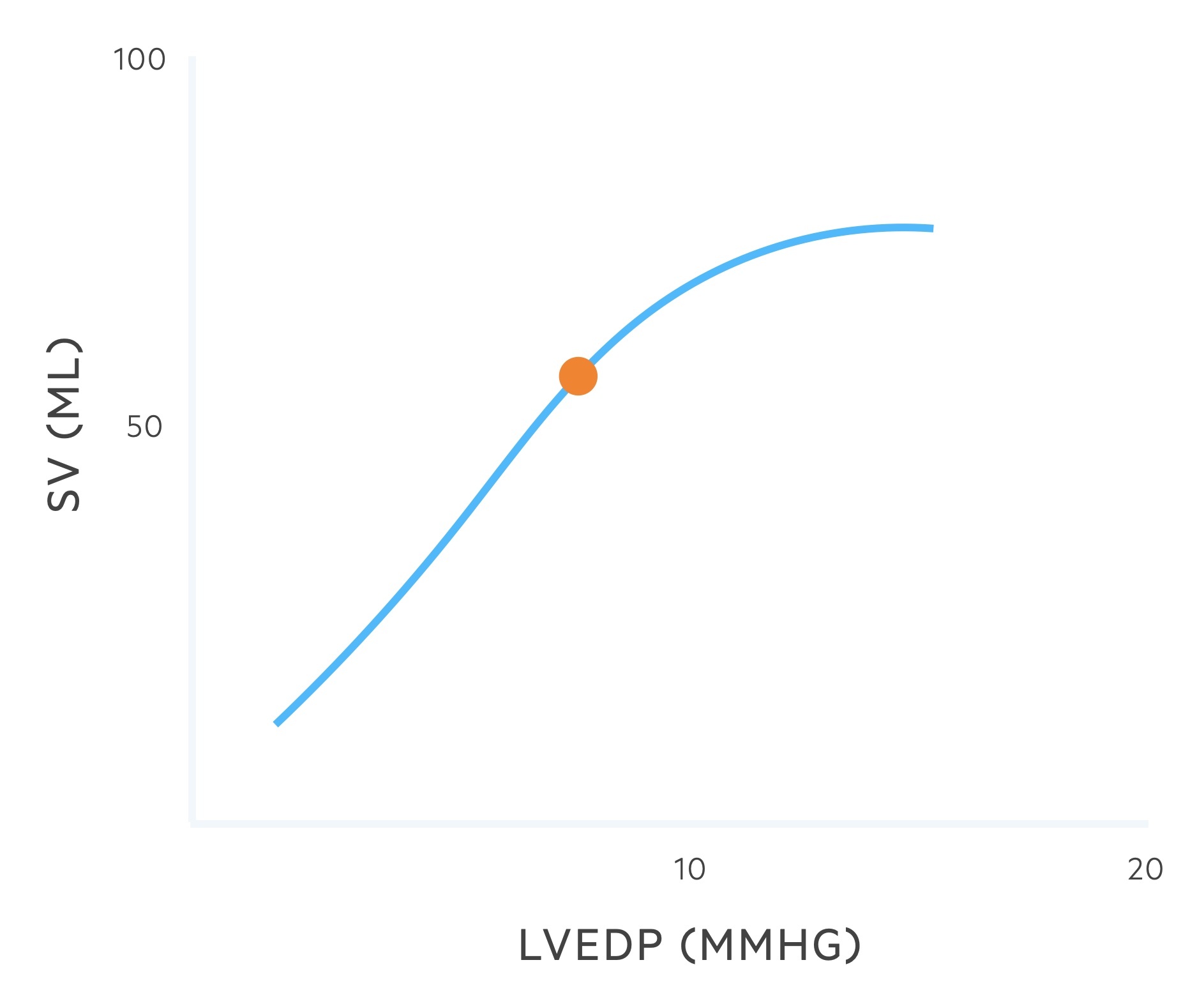
The Frank-Starling law describes the relationship of ventricular stretching (preload) & myocardial contractility. See Heart Failure notes for more detail.
Venous return (and so preload) is influenced by numerous factors:
- Skeletal muscle pump
- Respiratory suction
- Cardiac suction
- Sympathetic mediated vasoconstriction
- Blood volume
Blood pressure
Blood pressure = cardiac output x peripheral vascular resistance
Peripheral vascular resistance
Dependent upon two major variables: arteriolar radius and blood viscosity.
- Viscosity: primarily determined by the haematocrit i.e. the proportion of blood that is made up of red blood cells.
- Arteriolar radius:
- Intrinsic factors: These are local factors, the most important being changes to meet metabolic needs (such as O2). Other factors include temperature and the presence of histamines.
- Extrinsic factors: The most important is sympathetic controlled vasoconstriction. Other factors include ADH and angiotensin II.
Regulation of blood pressure
Numerous interconnected systems contribute to the regulation of blood pressure.
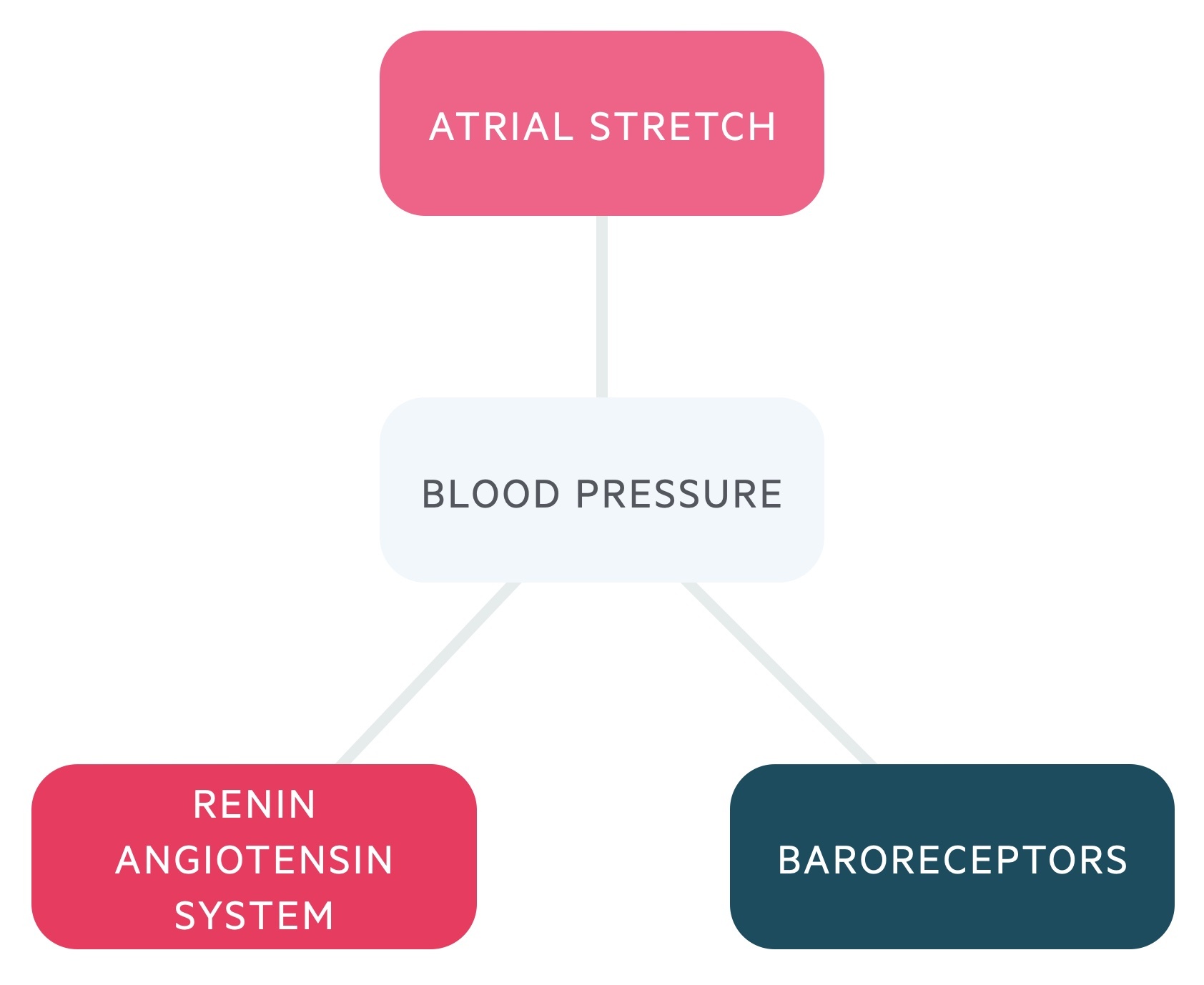
Baroreceptors allow the body to make rapid, short-term changes to blood pressure. Baroreceptors, a specialised mechanoreceptor, are located in the aortic arch and carotid sinus. These locations give vital information on blood pressure to the body and brain.
An increase in arterial pressures leads to an increase in baroreceptor firing. The cardiovascular control centre in the medulla may then augment the autonomic nervous system.


