Overview
The anti-hypertensives are an important & broad group of medications.
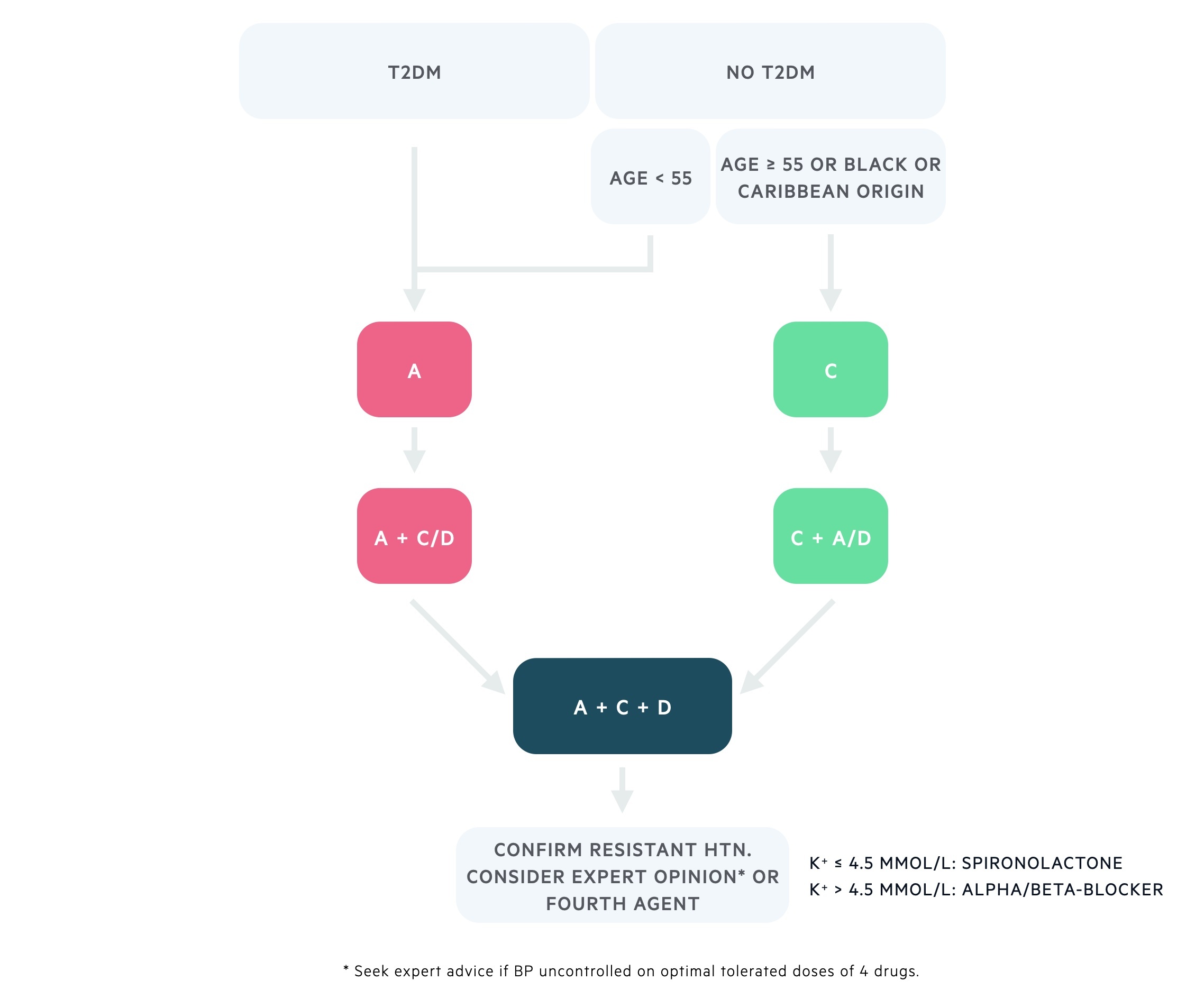
Hypertension is a very common condition that represents a significant source of morbidity and mortality. It is a major risk factor for MI, stroke and chronic kidney disease. Hypertension is managed in a step-wise fashion according to the NICE guidelines (see our Hypertension notes for more).
Several groups of drugs, by varying mechanisms, are used to reduce blood pressure.
Regulation
Blood pressure is maintained by a number of physiological reflexes that respond to acute and chronic changes.
Blood pressure = cardiac output x peripheral vascular resistance
Numerous interconnected systems contribute to the regulation of blood pressure. There are both immediate and long-term mechanisms, these include:
- Autonomic nervous system (ANS)
- Renin-angiotensin-aldosterone system (RAAS)
- Local chemical mediators
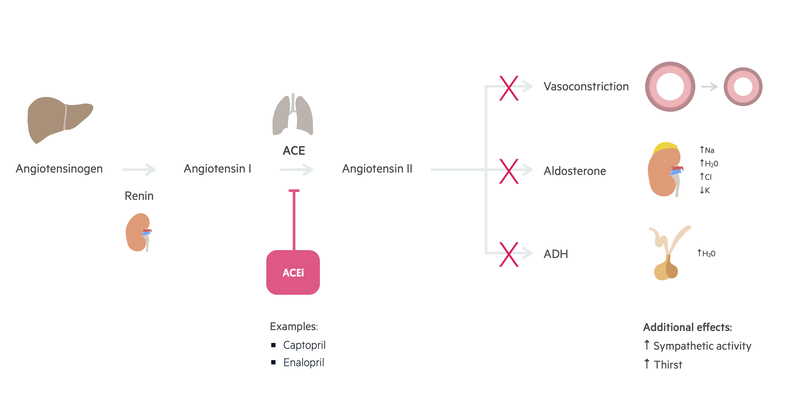
ACE inhibitors
Angiotensin-converting enzyme (ACE) inhibitors are a commonly used class of antihypertensives. They are also frequently utilised in heart failure and chronic kidney disease.
ACE inhibitors cause a reduction in circulating angiotensin II & aldosterone.
Examples: Ramipril, Lisinopril.
Mechanism of action
ACE inhibitors act by blocking the effect of ACE, causing a reduction in circulating angiotensin II. Reduction of angiotensin II has numerous effects:
- Reduced aldosterone secretion – involved in volume regulation via sodium and potassium excretion.
- Reduced ADH secretion – anti-diuretic hormone (ADH) acts on the kidneys to increase water reabsorption (independent of sodium).
- Reduced arterial vasoconstriction
- Reduced sympathetic activity
Adverse effects
A dry cough is a common side effect of ACE inhibitors. This is due to an increase in bradykinin within the lungs (ACE breaks down bradykinin).
Caution is also advised during intercurrent illnesses when using an ACE inhibitor. Their mechanism disrupts the kidneys autoregulation mechanisms and may prevent maintenance of adequate renal perfusion – resulting in an acute kidney injury (AKI). It is often advisable to stop ACE inhibitors during severe illness.
Other adverse effects include:
- Dry cough
- Headache
- Postural hypotension
- Rashes
- Angio-oedema
- Strongly teratogenic
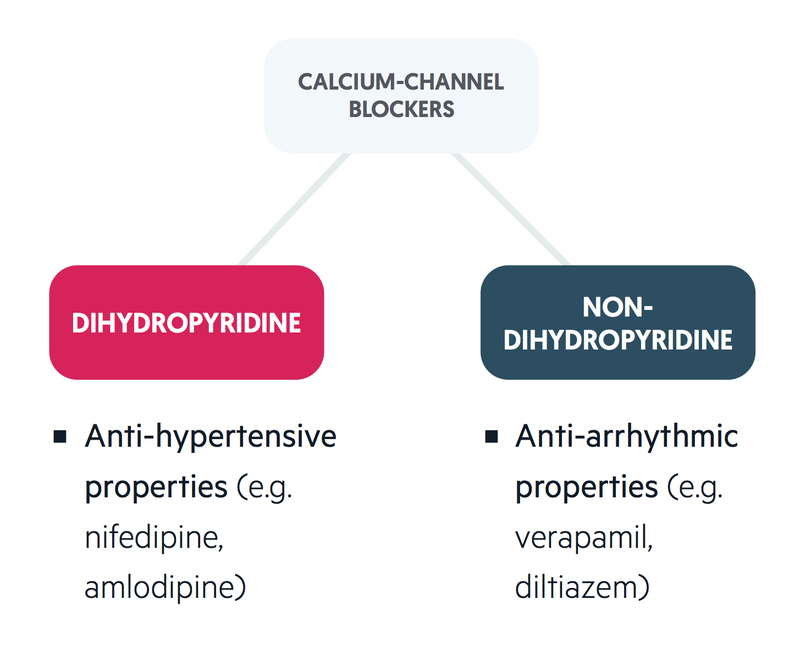
Calcium channel blockers
Calcium channel blockers (CCBs) are also a commonly used class of antihypertensives.
There are two main types of CCBs:
- Dihydropyridine: predominantly anti-hypertensive effects.
- Non-dihydropyridine: predominantly anti-arrhythmic effects.
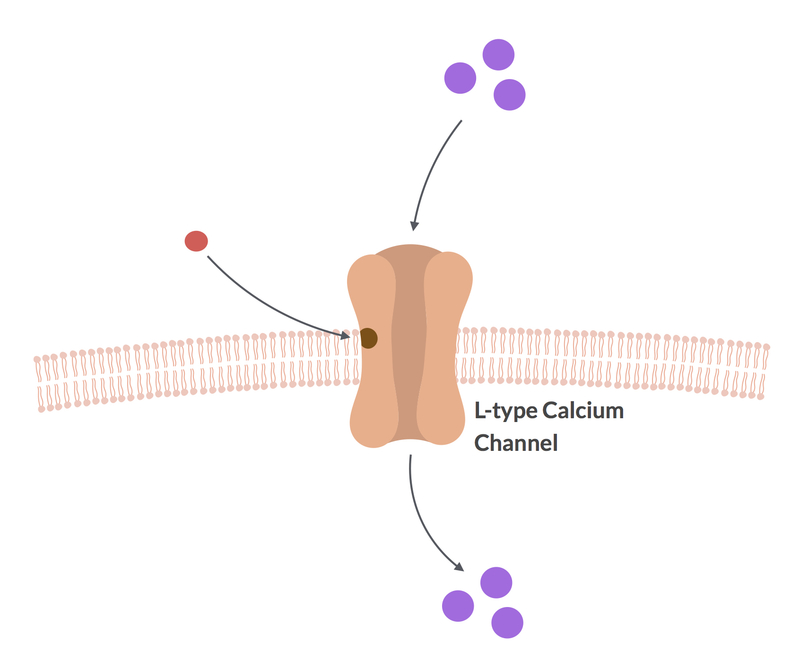
Dihydropyridine CCBs block the action of L-type calcium channels, which are found in vascular and cardiac tissue.
Examples: Amlodipine, Nifedipine.
Mechanism of action
CCBs block the action of voltage-gated L-type calcium channels, which are found in vascular and cardiac tissue. Within vascular smooth muscle, L-type channels permit the entry of calcium ions leading to contraction and subsequent vasoconstriction. Dihydropyridine CCBs inhibit this influx of calcium ions and induce vasodilatation, which reduces the peripheral vascular resistance.
Adverse effects
- Headache
- Flushing
- Dizziness
- Peripheral oedema
- Reduced cardiac contractility
- Constipation
Thiazide diuretics
The mechanism of the antihypertensive effects of thiazide diuretics are poorly understood.
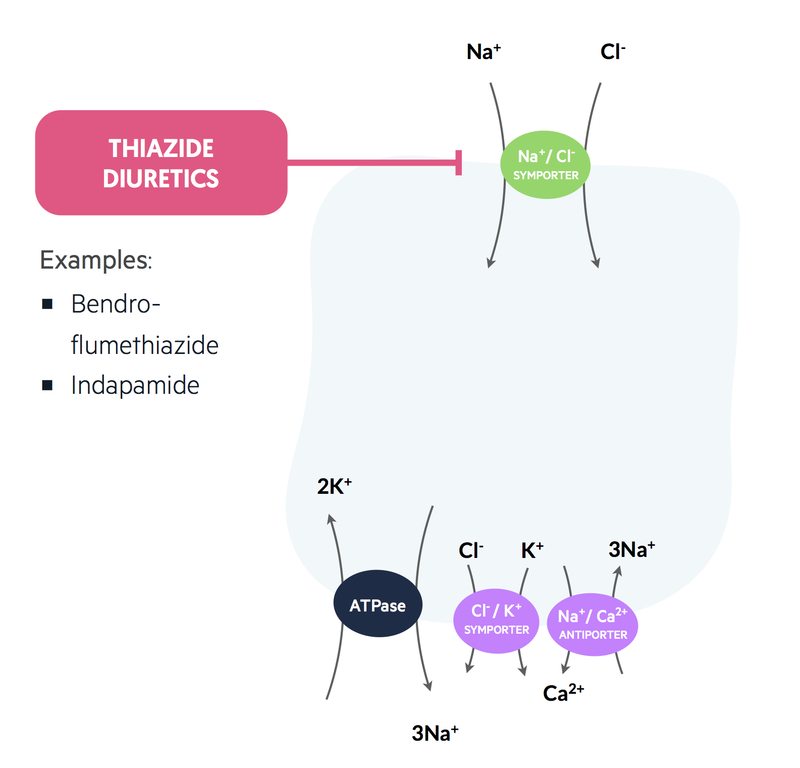
Examples: Bendroflumethiazide, Indapamide.
Mechanism of action
Thiazide diuretics act on the distal convoluted tubule (DCT) of the nephron where it inhibits the Na+/Cl– co-transporter. This prevents sodium and chloride entering the tubule cells and, therefore, water cannot follow.
This mechanism has an initial hypotensive effect, however, this is mostly abolished by the renin-angiotensin system (RAS). The long-term antihypertensive effects may be due to vasodilation of peripheral vasculature through a mechanism that is poorly understood.
Adverse effects
- Gout
- Impotence
- Hyperuricaemia (precipitating gout)
- Hypercalcaemia
- Hypokalaemia
- Hyponatraemia
- Hyperlipidaemia
- Urinary frequency
Alpha-1 blockers
Alpha-1 blockers act to blockade alpha-1 adrenoreceptors.
Examples: Doxazosin
Mechanism of action
Alpha-1 adrenoreceptors are found in most sympathetic tissues including vascular smooth muscle and have excitatory effects. Stimulation results in vasoconstriction.
Consequently, blockade of alpha-adrenoreceptors causes:
- Reduced arteriolar tone – lowering peripheral vascular resistance.
- Venous dilation – reducing venous return and cardiac output.
Adverse effects
- Postural hypotension
- Headaches
- Dizziness
- Nausea
- Rhinitis
- Urinary frequency
Beta-blockers
Beta-blockers act to reduce sympathetic activity
Examples: Propanolol, Atenolol.
Different agents may have variably selective action on beta-1 receptors (predominantly found in the heart) and beta-2 receptors (predominantly found in the lungs).
Mechanism of action
These drugs antagonise catecholamines at beta-adrenoceptors. The antihypertensive effect is mediated primarily by blockade of beta-1 adrenoreceptors. As such, they reduce the effect of the sympathetic nervous system on the heart. They, therefore, have both negative inotropic and negative chronotropic effects. That is they reduce the heart rate and the strength of contractions.
Beta-blockers cause a reduction in blood pressure through a number of mechanisms:
- Reduced cardiac output – through negative inotropic and negative chronotropic effects.
- Reduced renin release – blockage of the sympathetic triggered release.
- Vasodilation – due to blockade of beta-2 receptors in vascular smooth muscle (though the effect is thought to be minimal).
Adverse effects
- Postural hypotension
- Cold peripheries
- Headache
- Dizziness
- Insomnia, sleep disturbance
- Bradycardia
- AV nodal block (heart block)
- Bronchoconstriction (nonselective beta-blockers, a particular consideration in asthma and COPD)
- Hypoglycaemia (nonselective beta-blockers)
- Erectile dysfunction


