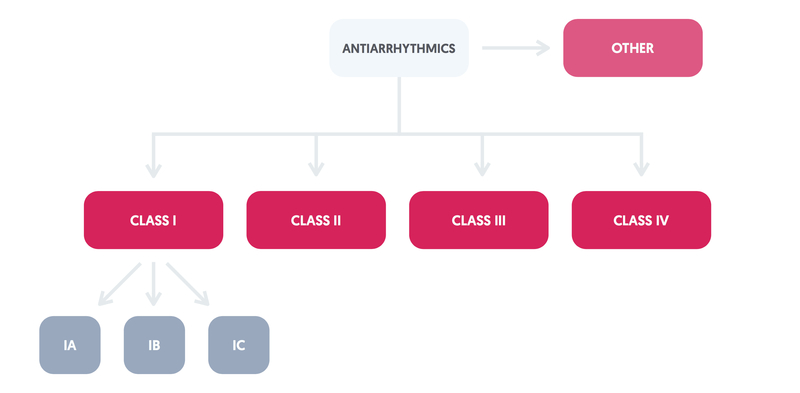
Vaughan-William’s classification
Anti-arrhythmics are drugs that modify cardiac conduction, they are used to treat arrhythmias and are classified according to the Vaughan-William’s system.
This classification divides these drugs into four classes according to their effects on cardiac action potential. Anti-arrhythmics have complex actions and classes may overlap.
It is important to note, that this classification system has become increasingly inadequate with improved understandings of drug mechanisms and development of new antiarrhythmics.
Arrhythmogenesis
To understand the action of the antiarrhythmics it helps to understand how arrhythmias may develop.
Arrhythmias are disorders of rate and rhythm of the heart, which arise due to either abnormal generation or conduction of electrical impulses.
Arrhythmogenesis may be due to increased automaticity, re-entry or triggered activity.
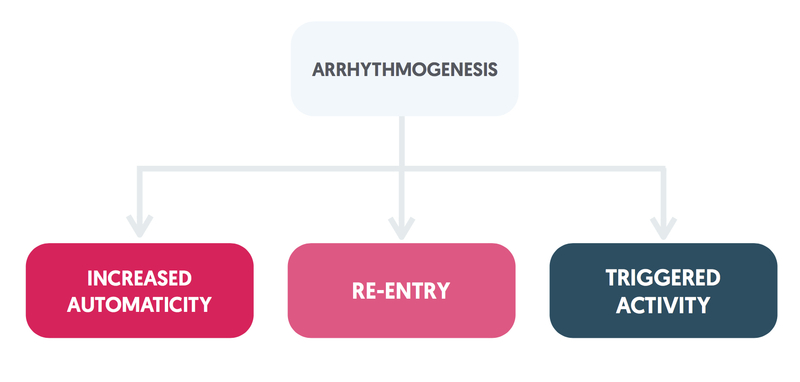
1. Increased automaticity
Occurs when tissue other than the SA node develops spontaneous depolarization that supersedes the SA node itself.
The origin may be:
- Conduction pathway – i.e. specialised autorhythmic cells.
- Contractile tissue – contractile cells may gain autorhythmic function for various reasons, e.g. ischaemia.
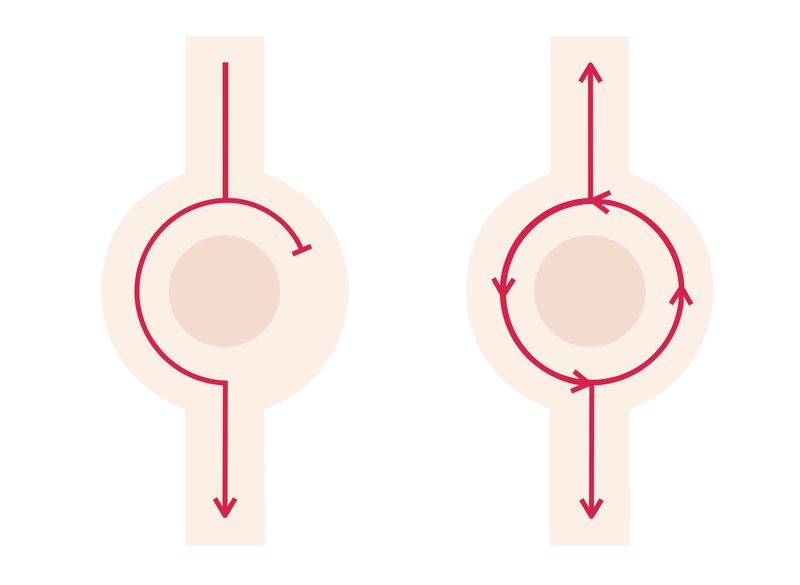
2. Re-entry
Begins when an electrical impulse reaches a branch in which one pathway is refractory (i.e it is not yet repolarised and as such cannot depolarise). The impulse simply passes down the conducting pathway and may meet the distal part of the refractory tissue once it has repolarised. The impulse may then be transmitted retrogradely through the this tissue.
A circuit is established. These circuits termed re-entry circuits may act as a pacemaker and trigger aberrant rhythms.
Re-entry is thought to be the cause of most clinically relevant arrhythmias.
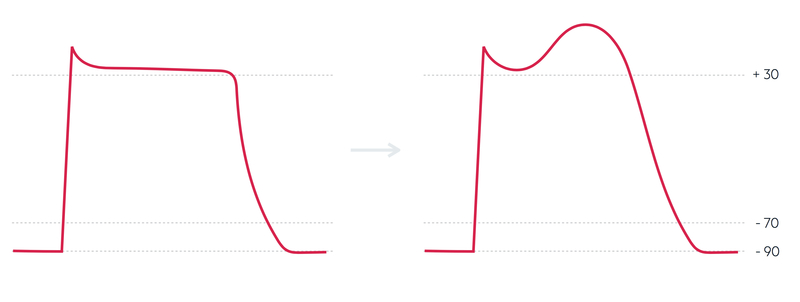
3. Triggered activity
Damage to the myocardium may lead to oscillations of membrane potentials at the end of the action potential, termed afterdepolarisations.
These afterdepolarisations may occur during (early) or following (delayed) repolarisation.
Digoxin toxicity results in arrhythmias due to this mechanism.
Pro-arrhythmic effects
It is important to recognise that the majority of anti-arrhythmic drugs have pro-arrhythmic effects.
Class IA antiarrhythmics and Sotalol may cause prolonged QT with an increased risk of polymorphic ventricular tachycardia (torsades des pointes).
The Cardiac Arrhythmia Suppression Trial (CAST) looked at Class IC antiarrhythmics. It discovered that in the post-myocardial infarction setting, there was increased mortality compared to placebo, potentially due to increased proarrhythmic effects. As such, these drugs are not used in patients with coronary artery disease.
Class I
Membrane depressants which block sodium channels; the class itself is split into three subtypes (IA-IC).
Class I antiarrhythmics slow depolarisation and with it conduction. These drugs act to reduce sodium entry through inhibition of fast sodium channels. The subtypes have variable effects on cardiac action potential.
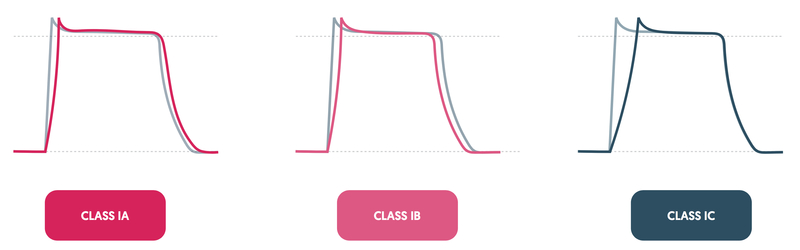
1. Class IA
- Phase 0: Depress
- Action potential: increases the duration of the action potential through inhibition of potassium channels.
- Examples: Quinidine, Procainamide, Disopyramide.
- Rarely used in the UK due to adverse effects.
2. Class IB
- Phase 0: Depress
- Action potential: decreases the duration of the action potential
- Examples: Lidocaine, Phenytoin.
3. Class IC
- Phase 0: Markedly depress
- Action potential: no effect
- Examples: Flecainide.
Adverse effects:
- Nausea & vomiting
- Negative inotropic effect
- Proarrhythmic effects
- CNS toxicity (Class IB and IC in particular)
- SLE-like syndrome (Procainamide)
- Cinchonism (condition caused by Quinidine overdose)
Class II
Beta blockers which act to reduce sympathetic activity.
Class II antiarrhythmics are antagonists of catecholamines at beta-adrenoceptors. They possess both negative inotropic and negative chronotropic properties.
They act on the AV node to reduce conduction and have variable selective action on beta-1 receptors (predominantly found in the heart) and beta-2 receptors (predominantly found in the lungs).
Examples: Propranolol, Bisoprolol.
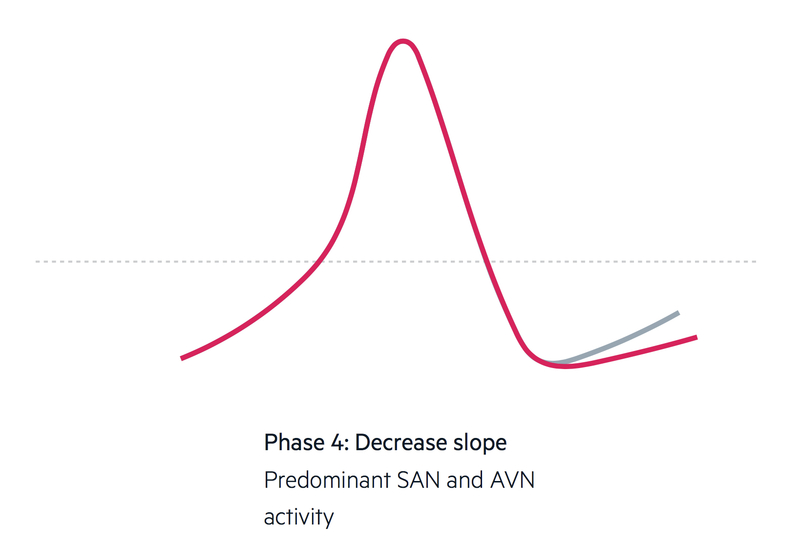
Mechanism of action
Antagonists of catecholamines at beta-adrenoceptors, possessing both negative inotropic and negative chronotropic effects; that is they reduce heart rate and the strength of contractions.
They act on the SA node to reduce the rate of spontaneous depolarisation (and so reducing the heart rate) by decreasing the slope of phase 4. In essence, slowing the spontaneous depolarisation of the pacemaker potential. They also act on the AV node to reduce conduction.
Adverse effects
- Postural hypotension
- Bradycardia
- AV nodal block (heart block)
- Bronchoconstriction (a particular consideration in severe asthma and COPD)
- Hypoglycaemia
- Erectile dysfunction
- Insomnia, sleep disturbance
Class III
A mixed category of drugs which prolong action potential, typically by blocking potassium channels.
Class III is a mixed category composed of drugs that prolong cardiac action potential, typically via blocking potassium channels.
Examples: Amiodarone, Sotalol.
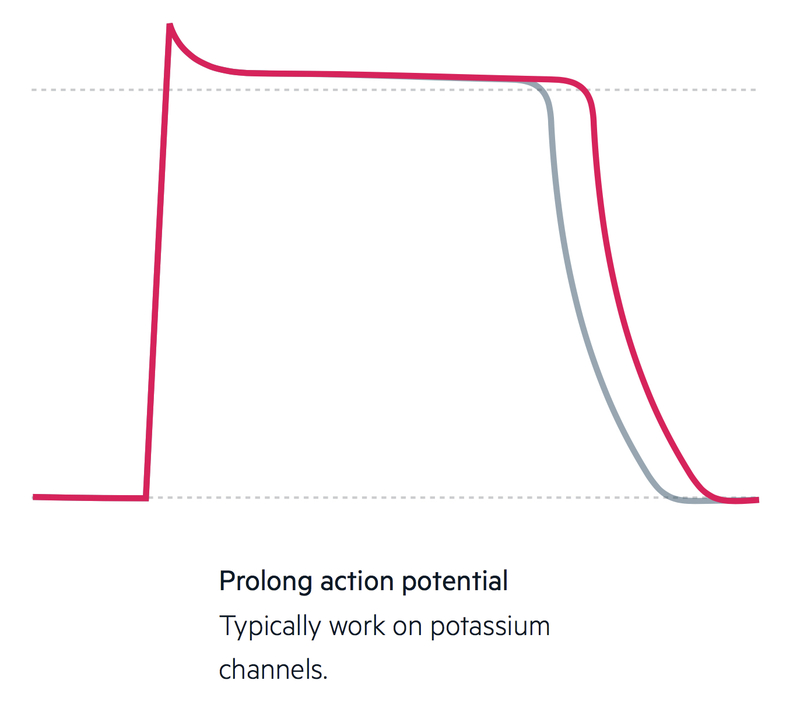
Mechanism of action
Block potassium channels, which are responsible for the completion of repolarisation (phase 3) in contractile cells. Blockade leads to an extension of the refractory period, through the prolongation of phase 2.
Adverse effects
- Amiodarone:
- Nausea
- Constipation
- Thyroid dysfunction (see our Hyperthyroidism and Hypothyroidism notes)
- Peripheral neuropathy
- Photosensitivity
- Lung fibrosis
- Proarrhythmic effects
- Hepatitis / cirrhosis
- Potentiates the effects of both digoxin and warfarin.
- Sotalol:
- see class II
Class IV
Non-dihydropyridine CCBs that act to reduce conduction at the AV node.
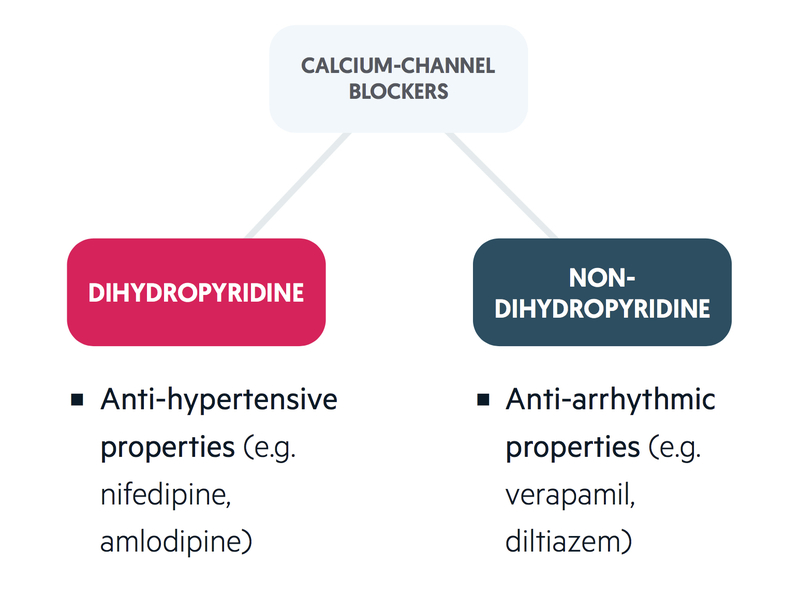
There are two types of calcium channel blocker (CCB):
- Dihydropyridines
- Non-dihydropyridines (itself divided into two categories).
It is the non-dihydropyridines which are more cardioselective and exhibit anti-arrhythmic effects.
Examples: Verapamil, Diltiazem.
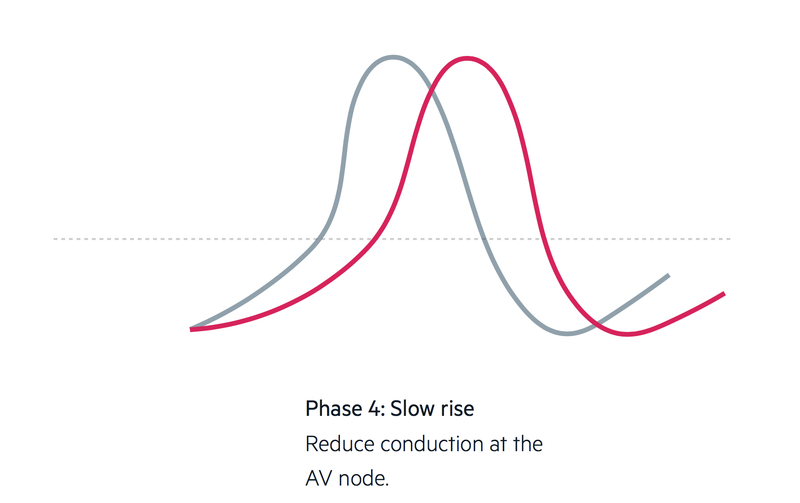
Mechanism of action
Non-dihydropyridines CCBs block L-type calcium channels. In autorhythmic cells, these channels bring the pacemaker potential past the threshold and cause spontaneous depolarisation (phase 4 and phase 0). L-type channels are more important in the completion of phase 4 in the AV node than in the SA node (here, depolarisation is more reliant on T-type calcium channels and funny channels).
Similar to beta blockers, non-dihydropyridine CCBs are both negative inotropes and negative chronotropes.
Adverse effects
- Bradycardia
- AV nodal block (heart block)
- Negative inotropic effect
- Constipation
- Gum hyperplasia
- Headaches, flushing, peripheral oedema – features associated with dihydropyridines (less common with non-dihydropyridines).
Other agents
A number of antiarrhythmics do no fit in the Vaughan-Williams classification.
1. Digoxin
Digoxin is a cardiac glycoside derived from the foxglove plant. It inhibits a Na+/ K+ -ATPase pump on cardiomyocytes. This pump acts to take sodium out of the cell and pump potassium back, in a ratio of 3:2. This helps drive calcium out of the cell via an exchanger.
This reduction in extracellular calcium results in an increase in intracellular calcium levels. As such, the contraction is more forceful (digoxin is a positive inotrope).
Primarily excreted by the kidneys, care is needed in patients with renal impairment. Digoxin may cause ECG changes including ST depression and T-wave changes. Digoxin toxicity may cause PR prolongation and lead to arrhythmias. In addition, hypokalaemia potentiates the effects of digoxin.
Adverse events are common due to its narrow therapeutic window, these include:
- Nausea and vomiting
- Visual disturbances (yellow halos, changes to colour perception – see van Gogh’s ‘Starry night’)
- Insomnia and sleep disturbance
- Proarrhythmic effects
- Gynaecomastia (disputed)
2. Adenosine
Adenosine, a purine nucleoside, acts on the SA node to reduce heart rate and the AV node to slow conduction. It is used primarily to treat supraventricular tachycardias, particularly those with an AV nodal re-entry circuit. It is rapidly metabolised with a half-life of less than 10 seconds.
Adverse effects:
- Sense of impending doom
- Bradycardia, AV block
- Flushing
- Headache
- Bronchospasm (avoid use in asthmatics)
3. Atropine
Atropine is a muscarinic antagonist that can be derived from the deadly nightshade plant. Atropine inhibits vagal activity alleviating parasympathetic depression of SA node activity, and as such the heart rate increases. It can be used to treat sinus bradycardia and AV block.
Adverse effects:
- Nausea
- Blurred vision
- Dilated pupils, photophobia
- Dry mouth
4. Magnesium sulfate
The antiarrhythmic mechanism is poorly understood. Used in the treatment of polymorphic ventricular tachycardia (torsades des pointes) and digoxin toxicity dysrhythmias (although is contraindicated in AV block or bradycardia).

