Overview
Prescribing intravenous fluids is one of the cornerstone tasks of junior doctors & prescribers.
Many patients who are admitted to hospital require intravenous fluids. The task of prescribing intravenous fluids typically falls under the realm of the junior doctor. Becoming proficient at prescribing fluids is one of the key skills during the first year of clinical practice.
The indication for fluids can be:
- Shock (inadequate tissue perfusion)
- Excess fluid losses (e.g. diarrhoea)
- Inadequate intake (e.g. nil by mouth)
- Replacing electrolytes (e.g. potassium)
The National Institute of Clinical Excellence (NICE) produced guidelines on the administration of intravenous fluids in both adults and children. However, it is difficult to learn how to exactly prescribe fluids from reading alone. This is because prescribing fluids is a very practical skill that takes into account multiple patient factors including co-morbidities, electrolyte abnormalities, and current medical issues.
We outline the tools you need to help you prescribe intravenous fluids, but this does not replace experience. Don’t worry! With practice and experience, everyone gets better!
Fluid balance
The human body is predominantly made up of water that is distributed into different compartments.
In the human body, water accounts for 40-70% of body weight. This percentage is variable because it depends on age (higher in children, lower in the elderly), sex, and tissue composition. This is then distributed into different compartments.
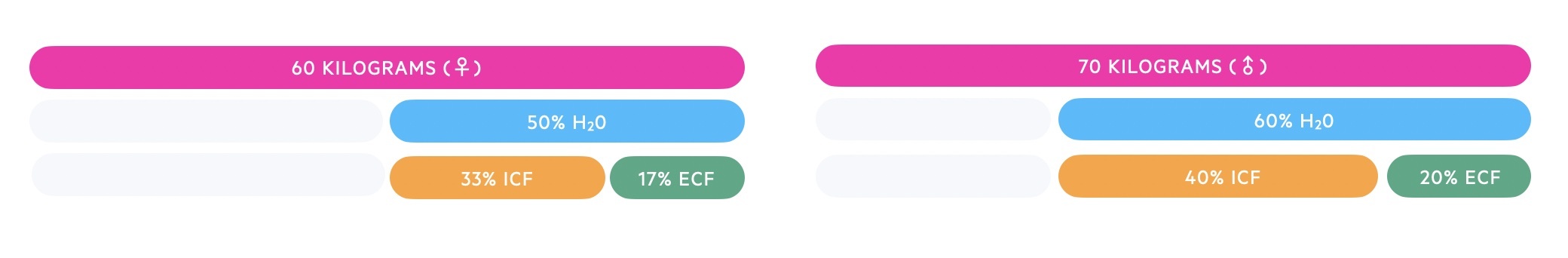
Total body water
In adult women, around 50% of body weight is made up of water and in adult men, it is 60%. The slightly lower percentage in women is because they tend to have a higher fat percentage and fatty tissue has a lower percentage of water compared to lean tissue.
This total water is distributed into two main compartments:
- Intracellular fluid (ICF): fluid within cells
- Extracellular fluid (ECF): fluid that surrounds cells
Intracellular fluid
This is the total fluid located within all our cells. It makes up two-thirds of total body water (TBW). In other words, 66% of the total amount of water within the body.
Extracellular fluid
This accounts for the remaining one-third of TBW. This third is further divided into two main compartments:
- Interstitial fluids: fluid that surrounds cells
- Plasma: the fluid component of blood
Numbers vary, but approximately 1/5th – 1/3rd of ECF is located within the plasma, and 2/3rd – 4/5th of ECF is located within the interstitial fluid.
A small proportion of ECF is located within the lymphatic system and transcellular fluid, but these are relatively minor compartments. Transcellular fluid refers to small, specialised fluid volumes, which are secreted by specific cells into body cavities (e.g. pleural or pericardial fluid).
Worked example
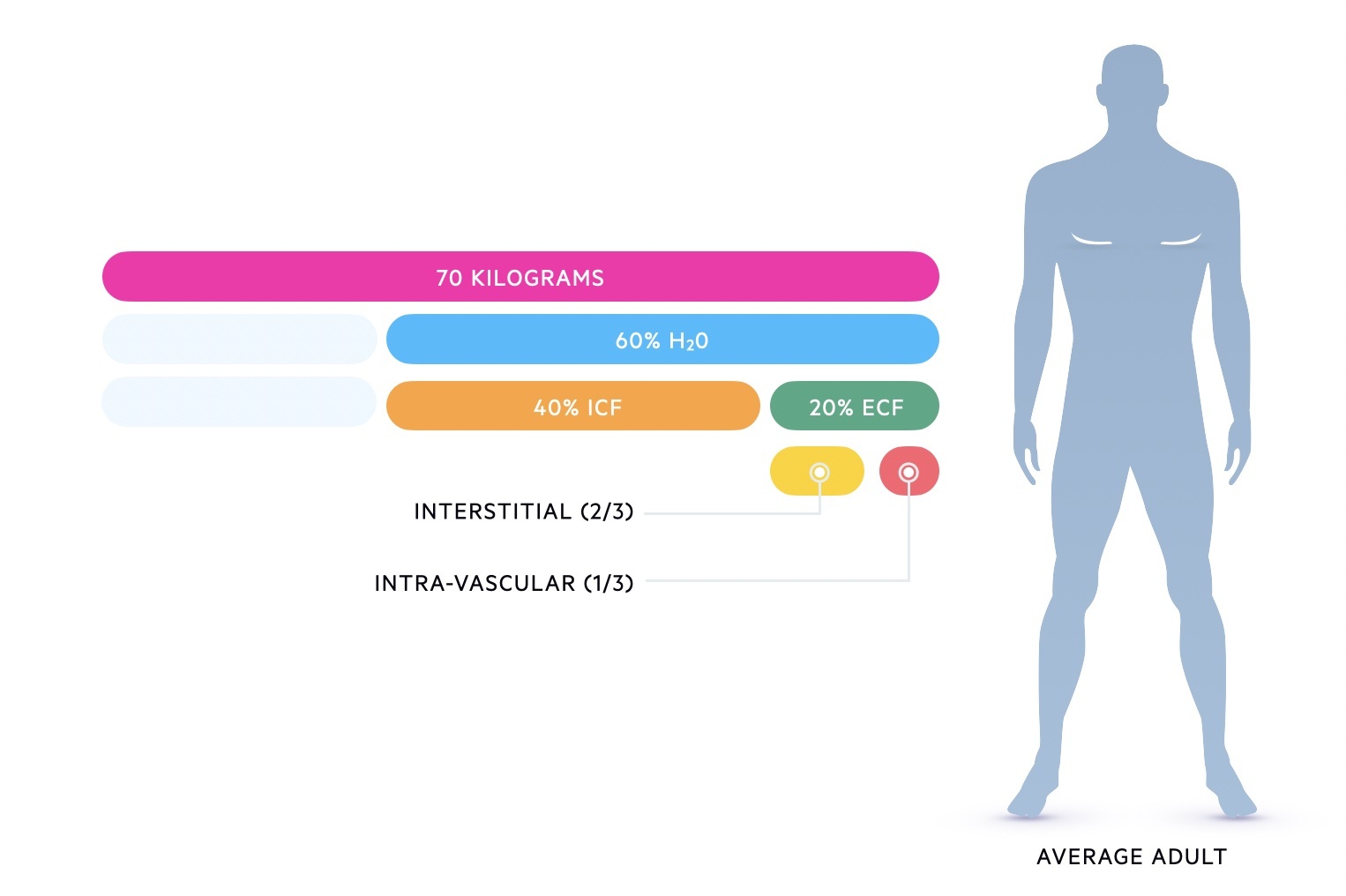
The distribution of fluid in a 70 kg male (60-40-20 rule):
- Total body water is 42 L (60% of body weight)
- Intracellular fluid is 28 L (40% of body weight)
- Extracellular fluid is 14 L (20% of body weight)
- Interstitial fluid is ~9-11 L (66-80% of ECF)
- Plasma fluid is ~3-5 L (20-33% of ECF)
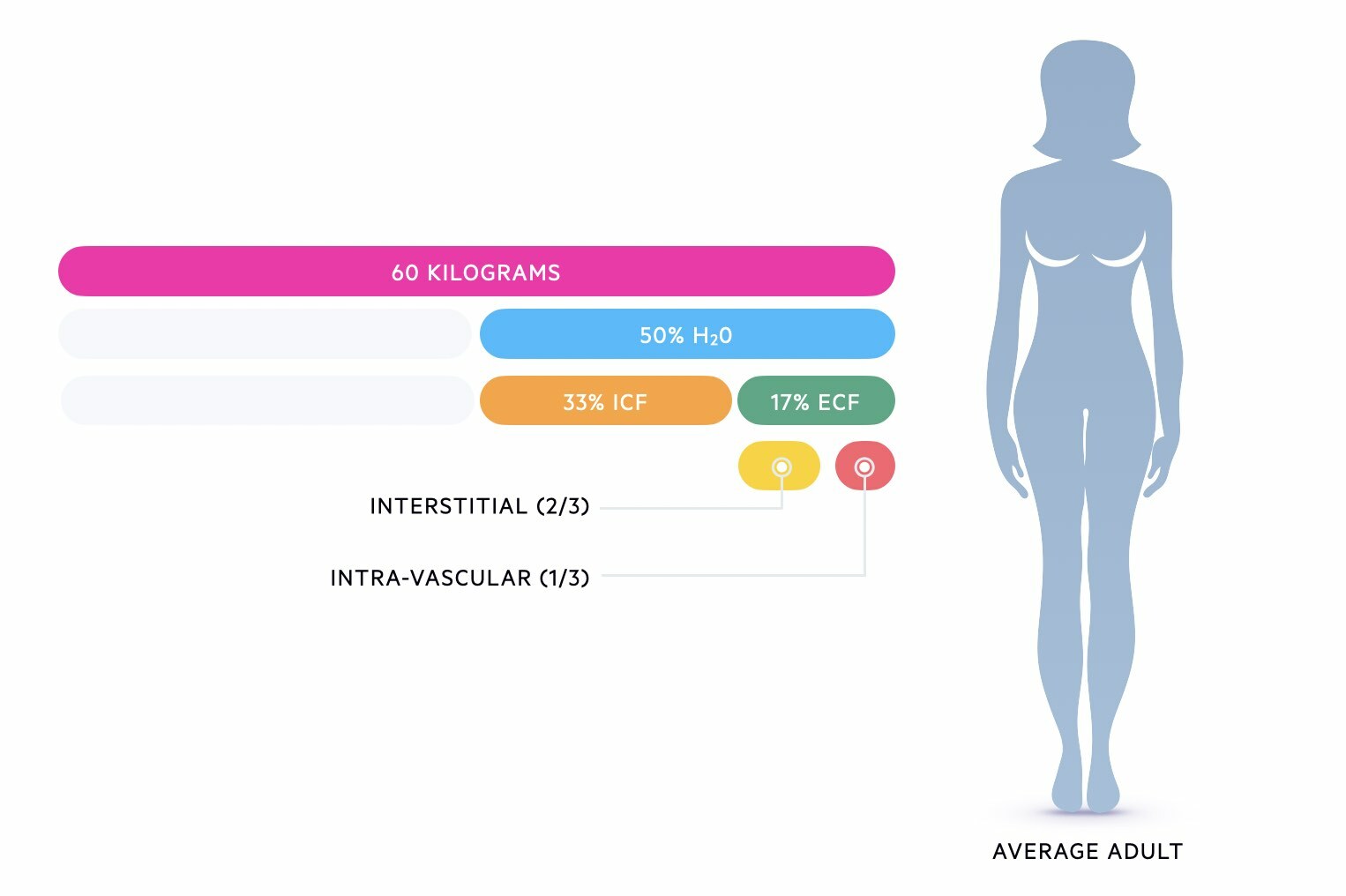
The distribution of fluid in a 60 kg female:
- Total body water is 30 L (50% of body weight)
- Intracellular fluid is 19.8 L (33% of body weight)
- Extracellular fluid is 10.2 L (17% of body weight)
- Interstitial fluid is ~7-8 L (66-80% of ECF)
- Plasma fluid is ~2-3 L (20-33% of ECF)
Types of fluids
Intravenous fluids can be broadly divided into colloids and crystalloids.
There are two main types of intravenous fluid solutions:
- Crystalloids: solutions with small molecules. Mainly consist of electrolytes and sterile water
- Colloids: solutions with larger molecules (e.g. albumin). They may be human-derived or semi-synthetic
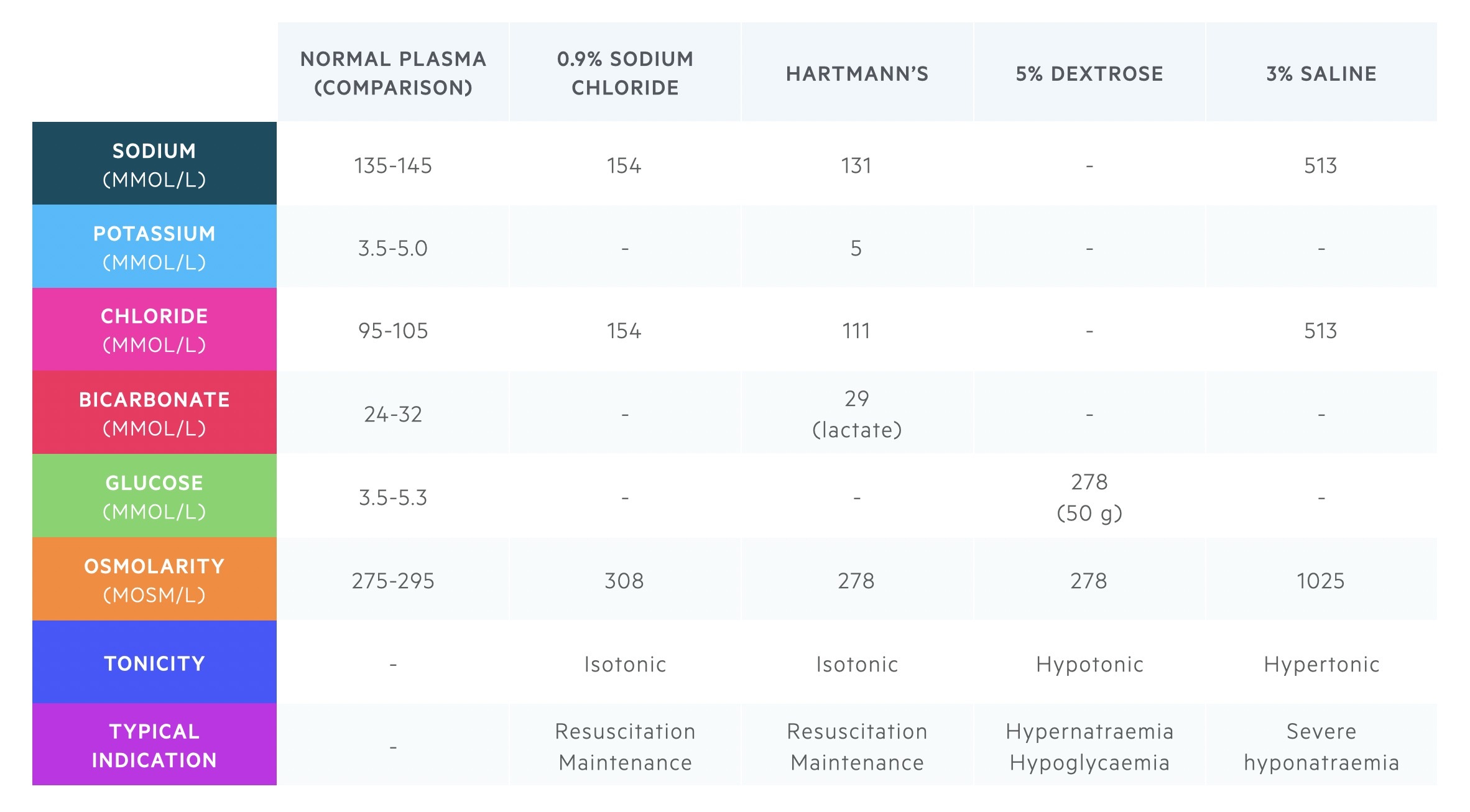
Crystalloids
Crystalloids are solutions that contain water-soluble electrolytes, sterile water, or other small molecules. They are the predominant fluid used in clinical practice. This is because of their low cost, safety profile, and efficacy.
Crystalloids may be defined as hypo-, iso-, or hypertonic with respect to blood plasma:
- Hypotonic (e.g. 5% dextrose): contain a lower concentration of dissolved solutes than plasma. Therefore, these fluids move freely by osmosis throughout the extracellular and intracellular space. They are not useful as resuscitation fluids.
- Isotonic (e.g. 0.9% sodium chloride): contain a similar concentration of dissolved solutes to plasma. Therefore, these fluids remain within the extracellular compartments. These form the cornerstone of fluid therapy
- Hypertonic (e.g. 3% sodium chloride): contain a higher concentration of dissolved solutes than plasma. Therefore, these fluids cause a movement of water by osmosis into the intravascular space. Can markedly derange electrolytes. Used with caution.
A crystalloid may be referred to as ‘balanced’ if it contains a similar electrolyte composition to plasma. Examples of balanced crystalloids include Hartmann’s solution or Plasma-Lyte.
The table below summarises the main crystalloids used in clinical practice.
Colloids
Colloids are solutions that contain large macromolecules, which can be human-derived or semisynthetic.
- Human derived colloids (e.g. Human albumin solution, packed red cells, fresh frozen plasma (FFP)): These usually have very specific indications (e.g. red cells for bleeding).
- Semi-synthetic (e.g. Gelatins or hydroxyethyl starch): These are not commonly used due to a number of side-effects and non-superiority to crystalloids.
Semi-synthetic colloids are proposed to remain in the intravascular space for longer because the larger molecules are unable to pass through semipermeable membranes and thus exert osmotic pressure. This leads to quick restoration of plasma volume and thus blood pressure. However, they are associated with a high incidence of anaphylaxis, impairment of coagulation, and renal toxicity. In the UK, they are rarely used in hospitals.
Daily requirement
When working out maintenance fluid, it is crucial to know daily requirements for water and electrolytes.
Understanding a patients’ daily requirements is important for the prescription of routine maintenance fluids. These requirements will form the basic prescription for administering fluids.
- Water: 25-30 ml/kg/day
- Sodium: ~ 1 mmol/kg/day
- Potassium: ~ 1 mmol/kg/day
- Chloride: ~ 1 mmol/kg/day
- Glucose: ~ 50-100 g/day (glucose 5% contains 5g/100 ml)
In a 52 kg patient, this would equate to:
- Water: 1.3-1.6 L per day
- Sodium: ~ 50 mmol per day
- Potassium: ~ 50 mmol per day
- Chloride: ~ 50 mmol per day
- Glucose: ~ 50 g per day
An appropriate prescription might be 1 L of 0.9% sodium chloride with 40 mmol potassium chloride and 0.5 L of 5% dextrose per day. Isotonic crystalloids (e.g. Hartmann’s, sodium chloride) are used much more commonly than hypotonic crystalloids like 5% dextrose. However, in this example, there is clearly way too much sodium and chloride for daily needs. Therefore, an alternative prescription may be 5% dextrose with 40 mmol potassium chloride and 0.5 L of 0.9% sodium chloride.
Clinical assessment
The clinical assessment is critical to determine a patients fluid needs.
The clinical assessment is at the pinnacle of fluid prescribing. Through assessing the patient, you can determine any factors that may influence your fluid prescription. These can include:
- Fluid balance or status (i.e. overloaded or dehydrated)
- Water and electrolyte losses (e.g. vomiting, diarrhoea)
- Co-morbidities (e.g. heart failure)
Fluid balance
An accurate fluid balance assessment is key.
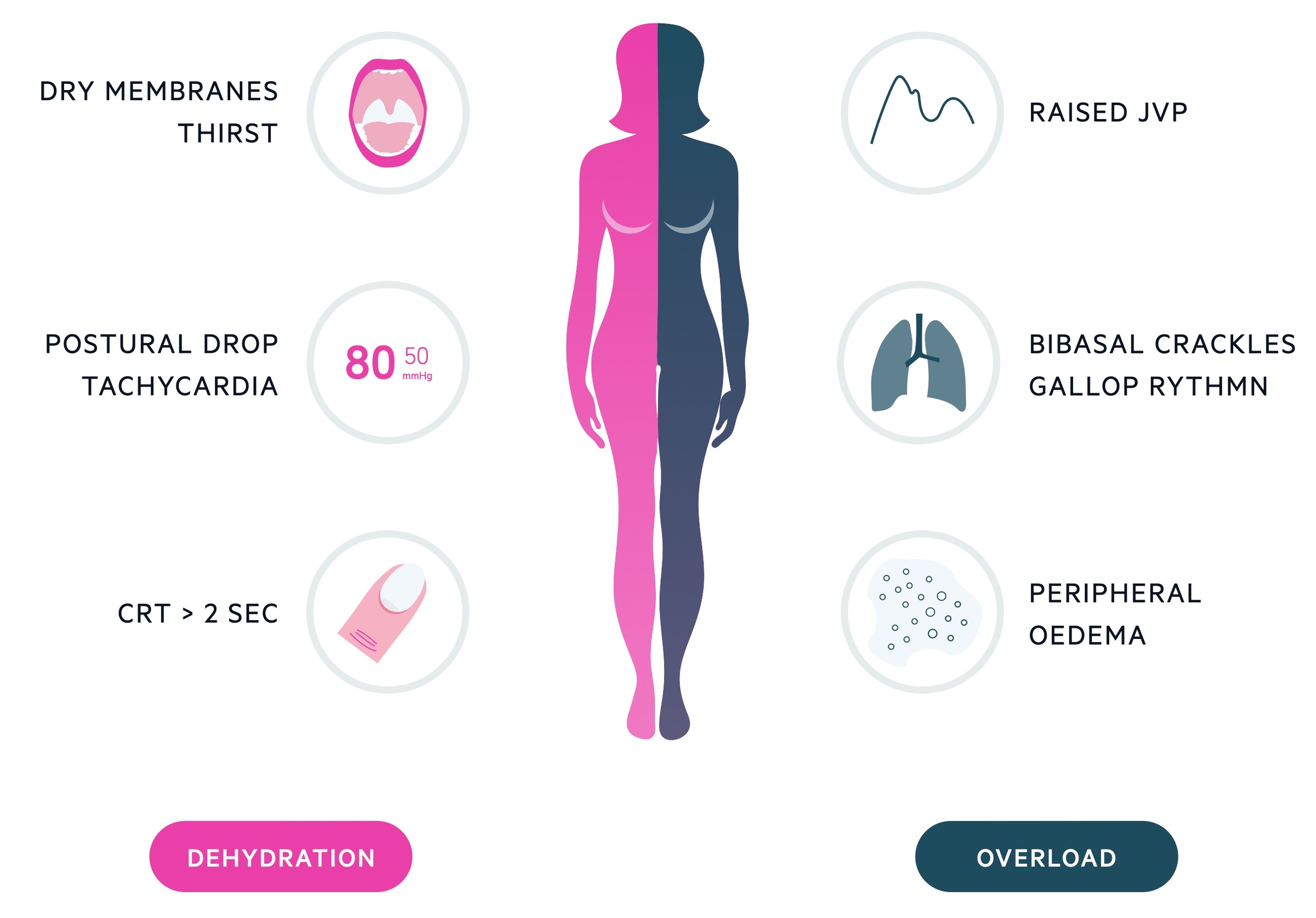
You should look for signs of dehydration or fluid overload by performing a clinical examination. Also note any outputs (urinary, diarrhoea, drain output) and review what has been going in and going out over the last 24 hours.
TIP: a urinary output that is reducing is suggestive of renal hypoperfusion. This is commonly due to hypovolaemia and is a good sign of dehydration.
Features of fluid overload
- Ankle swelling
- Dyspnoea
- Orthopnoea: breathlessness lying flat
- Paroxysmal nocturnal dyspnoea: waking in the night with shortness of breath
- Raised JVP
- Ascites
- Pleural effusions
These features suggest there is too much fluid and further prescriptions of intravenous fluids is inappropriate.
Features of dehydration
- Reduced capillary refill time
- Dry mucous membranes
- Reduced skin turgor
- Thirst
- Dizziness
- Reduced urine output
- Orthostatic hypotension
These features suggest the patient is dehydrated and needs additional fluids. If these cannot be met orally, or the patient is unstable (i.e. abnormal observations, deteriorating), then they will need intravenous fluids.
Water and electrolyte losses
It is important to note any additional fluid and electrolyte losses from the body.
Ongoing vomiting, recurrent fevers, diarrhoea or polyuria all need to be accounted for when prescribing intravenous fluids. For example, it is estimated that fluids needs can increase by 12.5% with each degree above 37.0º. These additional losses should be taken into account in addition to a patients basic daily requirements.
Additionally, different fluids have different compositions of electrolytes. For example, diarrhoea is associated with a large loss of potassium that needs to be replaced in addition to the ‘daily requirement’.
Bloods tests should be reviewed to help determine electrolytes and renal function. At a minimum, patients should have a ‘renal profile’ also known as ‘urea & electrolytes’ completed. This gives sodium, potassium and creatinine.
Co-morbidities
It is important to assess a patients co-morbidities prior to the prescription of fluids. Prescribing too much fluid to a patient with significant co-morbidities such as heart failure or to a frail elderly patient can precipitant iatrogenic fluid overload. In these patients, if fluid is needed then smaller volume prescriptions with frequent reassessment is key.
TIP: prescribing fluids in some patients is really difficult because of complex fluid needs, co-morbidities, or high outputs (e.g. high output stoma). Don’t be afraid to seek senior help!
Prescribing basics
It is important to have a simple, systematic approach to prescribing fluids in all patients.
Here are some simple steps to consider when prescribing fluids.
Consider the patient
How old is the patient? Be careful in patients who are old or frail – risk of fluid overload
How much does the patient weigh? This will help you work out the routine maintenance requirements
What are the patients’ co-morbidities? Be careful in patients with heart failure – risk of fluid overload
Consider the reason for fluids
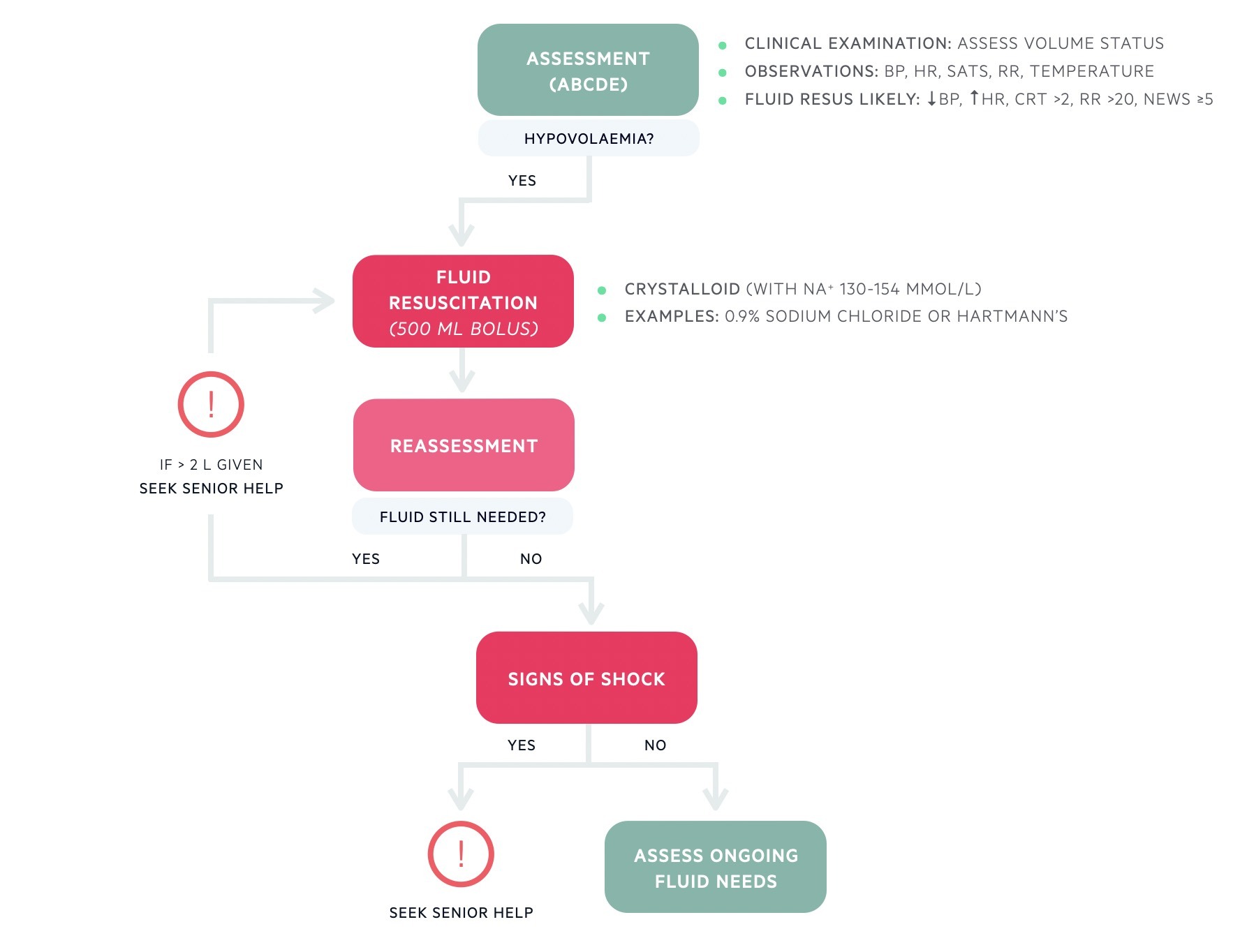
NICE created a helpful algorithm for the prescription of intravenous fluids. It broadly divides patients into those needing resuscitation fluid, those needing routine maintenance, and those with more complex needs that it terms ‘replacement and redistribution’.
- Resuscitation: fluid needed urgently to correct hypovolaemia
- Maintenance: fluid needed to meet daily requirements of water and electrolytes
- Complex fluids: prescription of fluid in patients with difficult to estimate requirements due to pre-existing losses or electrolyte abnormalities, ongoing losses or complex current issues (e.g. heart failure)
We have created simplified versions of the NICE algorithms that are shown below.
Consider the type of fluid
The majority of prescriptions will be crystalloids (e.g. Hartmann’s, Plasma-Lyte, 0.9% sodium chloride).
Remember, balanced crystalloids (e.g. Hartmann’s) have a fixed amount of other electrolytes. Normal saline (i.e. 0.9% sodium chloride) and dextrose solutions can come with different premixed concentrations of potassium chloride (e.g. 20 mmol or 40 mmol). Potassium should never be manually added to a bag of fluids.
If given peripherally, the concentration of intravenous potassium chloride should not exceed 40 mmol/L. Higher concentrations in a lower volume (e.g. 10-20 mmol in 100 mL normal saline) may be given in critical care units via a central line. The rate of administration should not normally exceed 10 mmol/hour. Higher infusions rates may be given in critical care areas with cardiac monitoring.
Consider the rate of fluid administration
The rate of infusion depends on the indication. There can be no ‘one size fits all’ and it is highly dependent on the patient, co-morbidities, and current clinical status. Here are some general principles:
- Resuscitation fluid: bolus (250-500 mL) over 15-30 minutes
- Dehydrated: 4-6 hourly
- Maintenance fluid: 8-12 hourly
- Fixed indications: e.g. diabetic ketoacidosis
- Frail/elderly or at risk of overload: 12 hourly (frequently reassess)
Consider electrolytes
Electrolyte replacement is really common and can be completed orally or intravenously. Potassium can be easily given as a pre-mixed solution with dextrose or sodium chloride.
Other electrolytes need to be replaced separately. These include:
- Phosphate: phosphate polyfusor (comes as a separate infusion)
- Magnesium: magnesium sulphate (usually mixed in sodium chloride)
- Calcium: calcium gluconate (given neat or mixed with 5% dextrose)
Review and reassess
It is essential to continually review and reassess patients following prescriptions of intravenous fluids. This is to assess the response to fluids with any change in their clinical status. Reassessment involves clinical assessment (e.g. fluid balance), monitoring (e.g. urinary output, blood pressure), and laboratory analysis (e.g. changes in electrolytes).
Resuscitation fluid
This involves the administration of urgent fluids to treat haemodynamic instability.
Resuscitation is the process of administering urgent intravenous fluids to treat haemodynamic instability. We outline the key principles for the administration of resuscitation fluids as outlined by NICE.
1. Urgent assessment
Assess the patient as with any acutely unwell patient with an ‘ABCDE’ approach. As part of this assessment determine their fluid balance. Features that suggest need for urgent resuscitation fluid include:
- Hypotension (< 90 mmHg)
- Tachycardia (> 90 bpm)
- Tachypnoea (RR > 30)
- Capillary refill time > 2 seconds
- High early warning score (NEWS ≥5)
2. Fluid resuscitation
If the patient is suspected to be hypovolaemic give a bolus of fluid. This means giving 500 mL of fluid over 15-30 minutes. Smaller volumes (e.g. 250 mL) may be given in patients at risk of fluid overload (e.g. heart failure).
It is important to give a crystalloid with sodium content between 130-154 mmol/L. In practice, this means giving either:
- Sodium chloride 0.9%, OR
- Balanced crystalloid (e.g. Hartmann’s, Plasma-Lyte)
3. Reassessment
Following a fluid bolus, it is important to assess the response based on clinical assessment and observations. If the patient is still hypovolaemic further fluid boluses can be given.
It is important to know when to seek senior help:
- Signs of shock
- > 2 litres given as fluid boluses
Once the patient has been stabilised, you can move on to determine their ongoing fluid requirements.
Maintenance fluid
The involves the administration of fluid to match a patients basic requirements.
Prescribing maintenance fluids involves generating a fluid prescription to meet a patients’ basic daily requirements. It is important to assess the patient to help determine:
- Any hypovolaemia? These patients need initial resuscitation fluid
- Any complex fluid/electrolyte requirements? These patients need a more thorough assessment with adjustment of the fluid prescription to account for any additional input, output, and electrolyte needs
- Can they meet intake orally or enterally? If yes, patients do not need intravenous fluids and should maintain both fluid and nutrition orally or enterally (e.g. nasogastric or nasojejunal tube).
If the patient does need intravenous fluids (e.g. by mouth status) and they do not have complex fluid needs, a basic prescription should ensure they are meeting their daily requirements:
- Water: 25-30 ml/kg/day
- Sodium: ~ 1 mmol/kg/day
- Potassium: ~ 1 mmol/kg/day
- Chloride: ~ 1 mmol/kg/day
- Glucose: ~ 50-100 g/day (glucose 5% contains 5g/100 ml)
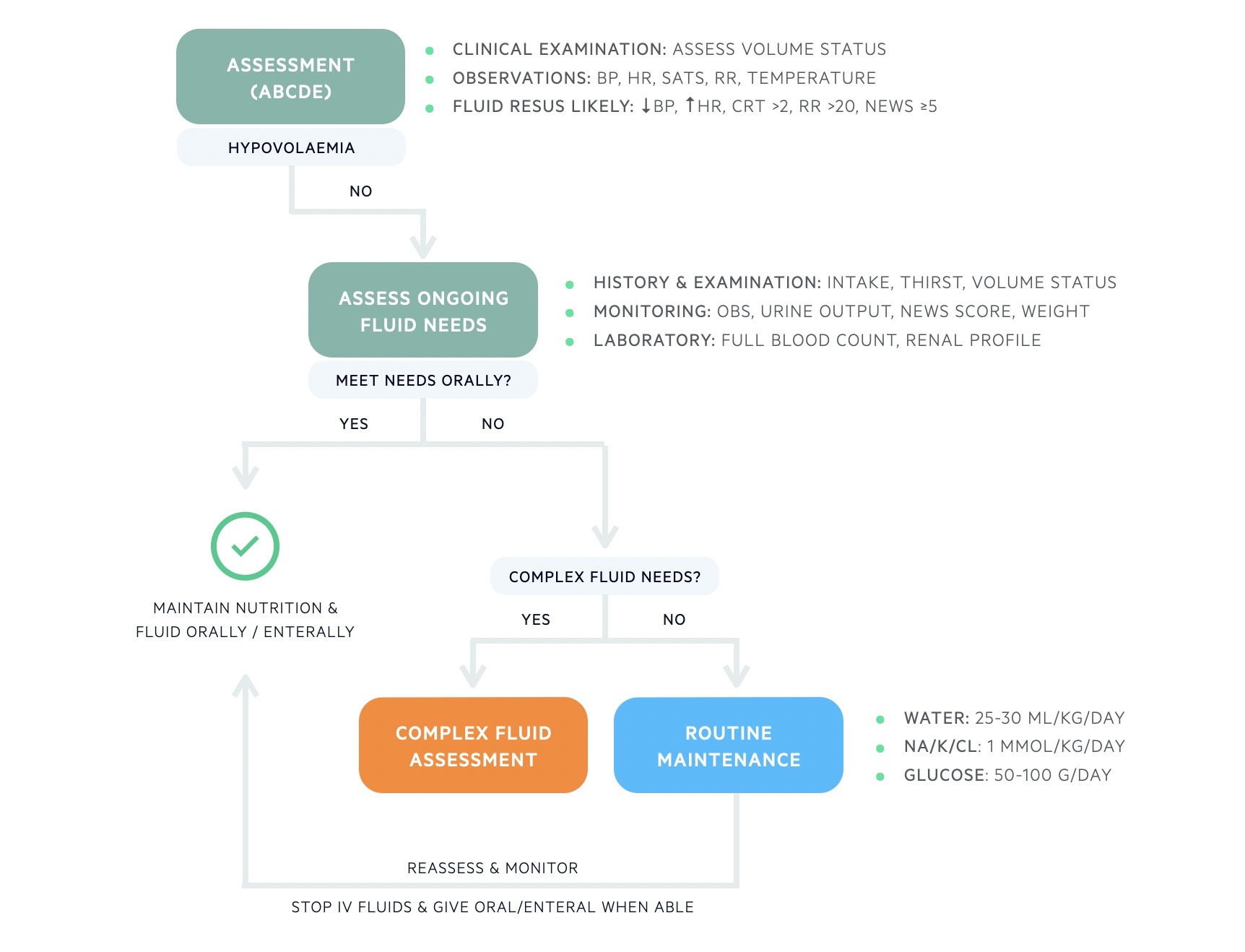
Complex fluids
The involves the adjustment of maintenance intravenous fluids to account for the clinical status of the patient.
There are many factors to account for when prescribing intravenous fluids. These can broadly be grouped into three categories:
- Existing fluid or electrolyte deficits
- Ongoing fluid or electrolyte losses
- Problems with redistribution of fluid or complex issues
The NICE guideline of intravenous fluid prescribing describes this as ‘replacement and redistribution’.
When prescribing ongoing intravenous fluids these additional factors need to be taken into account and then the routine maintenance prescription adjusted. For example, if a patient is already dehydrated and has a > 2 litre stoma output per day, they will require more fluid than just 25-30 ml/kg/day to ensure euvolaemia (i.e. normal fluid balance).
Determining complex fluid needs is the hardest part of prescribing intravenous fluids and comes with clinical experience. There is no one right answer for every case and it can be very subjective. This type of skill will come with practice!

Worked examples
We give a few scenarios of prescribing fluid in clinical practice, but make sure you practice lots on the wards!
Case 1 – resuscitation
A 64-year-old man is admitted to the accident and emergency resuscitation bay with fever and tachycardia. On examination, he appears flushed and hot peripherally. He has a bounding pulse at 112 bpm. Chest is clear to auscultation and heart sound are normal. The JVP cannot be observed. He has dry mucous membranes. He is treated for suspected urosepsis. You have been asked to prescribe fluids.
What is your assessment of this patient?
‘This patient is unwell with signs of dehydration and hypovolaemia secondary to sepsis’
What type of intravenous fluid does this patient need?
‘This patient needs urgent resuscitation fluid’
What type of fluid would you choose?
‘A crystalloid with sodium content 130-154 mmol/L such as 0.9% normal saline or Hartmann’s’
How much fluid would you give?
‘I would give a 500 mL bolus and then reassess’
Case 2 – routine maintenance
A 37-year-old is admitted under the general surgeons for an elective hernia repair. He has no significant co-morbidities. He weighs 70 kg. He is made nil by mouth and you have been asked to prescribe him fluids for the next 24 hours.
What is your assessment of this patient?
‘This patient is well and awaiting elective surgery. He has no abnormal losses or co-morbidities to suggest complex fluid requirements.’
What type of intravenous fluid does this patient need?
‘This patient needs routine maintenance fluid’
How would you choose what fluid to give?
‘This patient needs fluids to meet his basic daily requirement, which would be 1.75-2.1 L of water per day (25-30 ml/kg/day) with 70 mmol of potassium/sodium/chloride (1 mmol/kg/day).’
Which fluids would you give?
‘I would give 1 L of a balanced crystalloid and 1 L of 0.9% sodium chloride with 40 mmol/L of potassium chloride over 24 hours. This slightly underestimates the patient’s potassium but would be reasonable with monitoring the U&Es. If the patient is to be nil by mouth for several days, you may consider replacing one of these isotonic crystalloids with 5% dextrose to provide 100 g of glucose per day.’
Case 3 – replacement and redistribution
An 82-year-old is admitted under the gastroenterology team with diarrhoea. She has a background of ulcerative colitis and is currently opening her bowels 10-12 times per day. On examination, she has dry mucous membranes and appears dehydrated. Observation show HR 110 bpm, BP 110/86 mmHg. On her blood tests, she has evidence of an acute kidney injury (creatinine 211 umol/L) and hypokalaemia (K+ 2.8 mmol/L). She is given 1000 mL of 0.9% normal saline as resuscitation fluids and you have been asked to prescribe ongoing fluids for the next 24 hours. The patient weighs 50 kg.
What is your assessment of this patient?
‘This patient is unwell with a flare of ulcerative colitis. She is dehydrated based on her clinical assessment and laboratory investigations. She has already been given some resuscitation fluid. She has complex needs due to pre-existing dehydration, hypokalaemia, and acute kidney injury’.
What type of intravenous fluid does this patient need?
‘This patient needs assessment of their complex fluid requirements. Due to dehydration and acute kidney injury they will need extra intravenous fluids in addition to their routine maintenance. Due to the hypokalaemia, they will need additional potassium replacement.’
How would you choose what fluid to give?
‘This patient’s basic fluid requirement each day is 1.25-1.5 L of water (25-30 ml/kg/day) with 50 mmol of potassium/sodium/chloride (1 mmol/kg/day). They are already hypokalaemic (2.8 mmol/L) so need extra potassium supplementation as a pre-mixed solution with sodium chloride. They are already dehydrated and have acute kidney injury so will need extra water (e.g. at least 3 litres over the next 24 hours).’
Which fluids would you give?
‘I would give 1 L of 0.9% sodium chloride with 40 mmol/L of potassium chloride over 4-6 hours. I would then reassess and consider taking a repeat U&E blood test. I would then prescribe a further 1 L of 0.9% sodium chloride with 40 mmol of potassium over 6 hours followed by a balance crystalloid over 6 hours. This also depends on what she can tolerate orally.’
The importance here is about reassessment. If there were signs of fluid overload or worsening losses, we could alter the fluid prescription accordingly.

