Overview
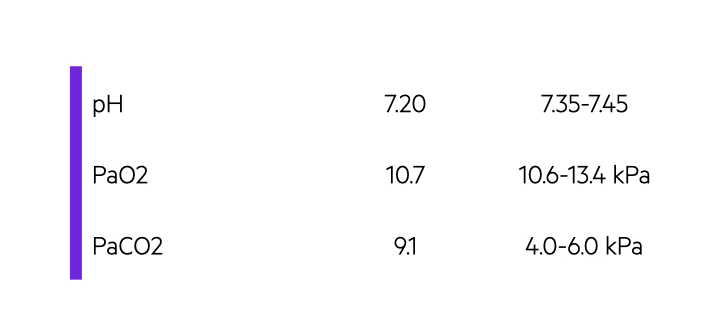
Respiratory acidosis is characterised by a pH < 7.35 and raised partial pressure of arterial carbon dioxide (>6 kPa).
Respiratory acidosis primarily occurs as a result of inefficient clearance of carbon dioxide from the lungs. It may be acute or chronic. It is characterised by acidosis (pH < 7.35) and a high PaCO2 (elevated above the upper limit of the reference range). This is commonly 6 kPa.
The increase in carbon dioxide may occur due to several mechanisms:
- Abnormal alveolar ventilation (lungs unable to clear carbon dioxide)
- Increased carbon dioxide production (systemic illnesses increase levels and ‘overwhelm’ lungs)
- Increased carbon dioxide intake (e.g. rebreathing gas containing carbon dioxide or absorption due to laparoscopic surgery)
Abnormal ventilation is commonly implicated in respiratory acidosis. It impairs the ability of the alveoli to effectively complete gas exchange and get rid of carbon dioxide. This may occur acutely or cause a more chronic picture.
Abnormal ventilation
Respiratory acidosis commonly occurs as a result of abnormal ventilation, which impairs carbon dioxide clearance.
There are several causes of abnormal ventilation problems leading to respiratory acidosis:
- Primary lung disease
- Chest wall abnormalities (i.e. impaired parenchymal expansion)
- Neuromuscular disorders
- Central nervous system depression (e.g. low consciousness)
- Airway obstruction (e.g. asthma – sign of ‘near fatal’ asthma, laryngospasm)
Primary lung disease
Diseases that effect the lung parenchyma or the vasculature can impair ventilation and thus carbon dioxide excretion. Commonly implicated conditions include chronic obstructive pulmonary disease (COPD), pulmonary fibrosis or pulmonary hypertension.
It may cause patients to present acutely with respiratory acidosis that may require non-invasive ventilation. Alternatively, to can cause chronic respiratory acidosis with evidence of marked metabolic compensation (i.e. significantly elevated bicarbonate levels).
Chest wall abnormalities
Any condition which restricts normal movement of the chest wall can increase the risk of respiratory acidosis. These conditions reduce the total lung volume and impact on parenchymal expansion. This reduces the area available for ventilation to clear carbon dioxide.
Important causes:
- Pleural disease (e.g. effusion, pneumothorax)
- Obesity
- Skeletal abnormalities (e.g. kyphosis, scoliosis)
Neuromuscular disorders
Many neuromuscular disorders can impair the muscles of respiration leading to poor ventilation and respiratory acidosis.
Major causes:
- Transient dysfunction (e.g. electrolyte disturbances like hypokalaemia)
- Neurological disorders (e.g. motor neurone disease, Guillain-Barre syndrome, myasthenia gravis, high cord lesions)
- Toxins (e.g. organophosphate ingestion, tetanus, and botulism)
- Myopathies (e.g. Duchenne’s muscular dystrophy)
Central nervous system depression
Any cause of cerebral depression can lead to alveolar hypoventilation, accumulation of carbon dioxide and subsequent respiratory acidosis. Classic examples include medications (e.g. morphine), head trauma, systemic illness, infections, or stroke.
Importantly, hypercapnia (high PaCO2) itself is a major cause of drowsiness, confusion and ultimately low consciousness. Therefore, development of hypercapnia and respiratory acidosis exacerbates the respiratory depression.
Acute respiratory acidosis
In respiratory acidosis, it’s important to assess the clinical severity and determine the chronicity.
Acute respiratory acidosis can present with significant hypoxaemia, electrolyte disturbances, cardiovascular instability, loss of consciousness and ultimately cardiac arrest.
It is usually indicated by an acute insult (e.g. opiate overdose, or acute exacerbation of COPD) with a new respiratory acidosis and no evidence of chronic compensation (e.g. normal bicarbonate). Acute respiratory acidosis can be a life-threatening event and may be associated with respiratory failure (Pa02 < 8 kPa).
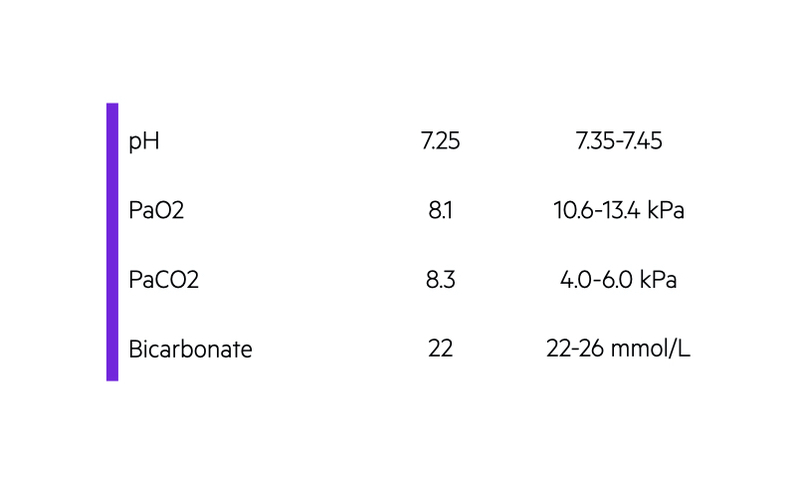
Acute respiratory acidosis may be associated with type 2 respiratory failure (T2RF). This describes hypoxaemia (Pa02 < 8 kPa) alongside hypercapnia (PaCO2 > 6 kPa). It takes the kidneys time to compensate for respiratory acidosis (> 24 hours to several days for peak effect). Therefore, patients usually require urgent treatment with invasive or non-invasive ventilation depending on severity, underlying cause and co-morbidities. If normal alveolar ventilation can be restored, it usually leads to a rapid fall in PaCO2 and improvement in acidosis.
Common examples of acute respiratory acidosis:
- Acute exacerbation of COPD
- Drug and alcohol use (e.g. benzodiazepine, opiates)
- Pneumonia
- Obesity hypoventilation syndrome
Often, patients already have a known diagnosis of COPD or chronic neurological condition (e.g. myasthenia gravis), which makes the diagnosis easier. Further investigations and treatment depends on the underlying cause.
Chronic respiratory acidosis
Chronic respiratory acidosis is typically seen in patients with long-standing COPD and marked metabolic compensation.
There may be evidence of chronic respiratory acidosis on the blood gas, which is demonstrated by a significant elevated bicarbonate level, often in the 30s. Chronic respiratory acidosis may be fully compensated with evidence of a normal pH, elevated PaCO2 and significantly elevated bicarbonate level
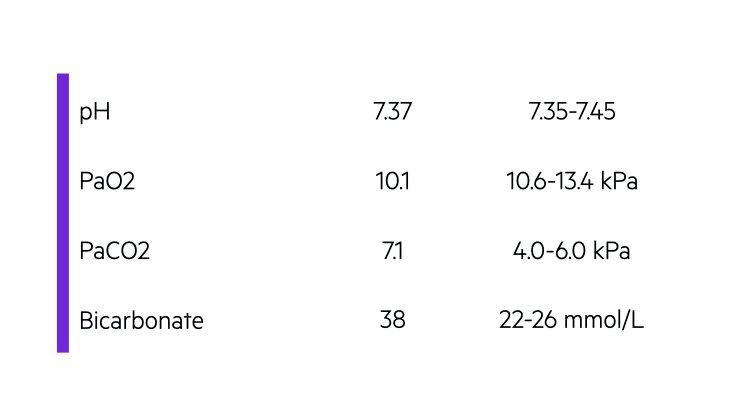
Common causes of chronic respiratory acidosis include:
- COPD
- Chronic neurological disorders (e.g. motor neuron disease)
- Chronic neuromuscular disorders (e.g. myopathies)
- Obesity hypoventilation syndrome
Patients with chronic respiratory acidosis usually have evidence of chronic T2RF and may require long-term oxygen therapy and/or long-term non-invasive ventilation.

