Key facts
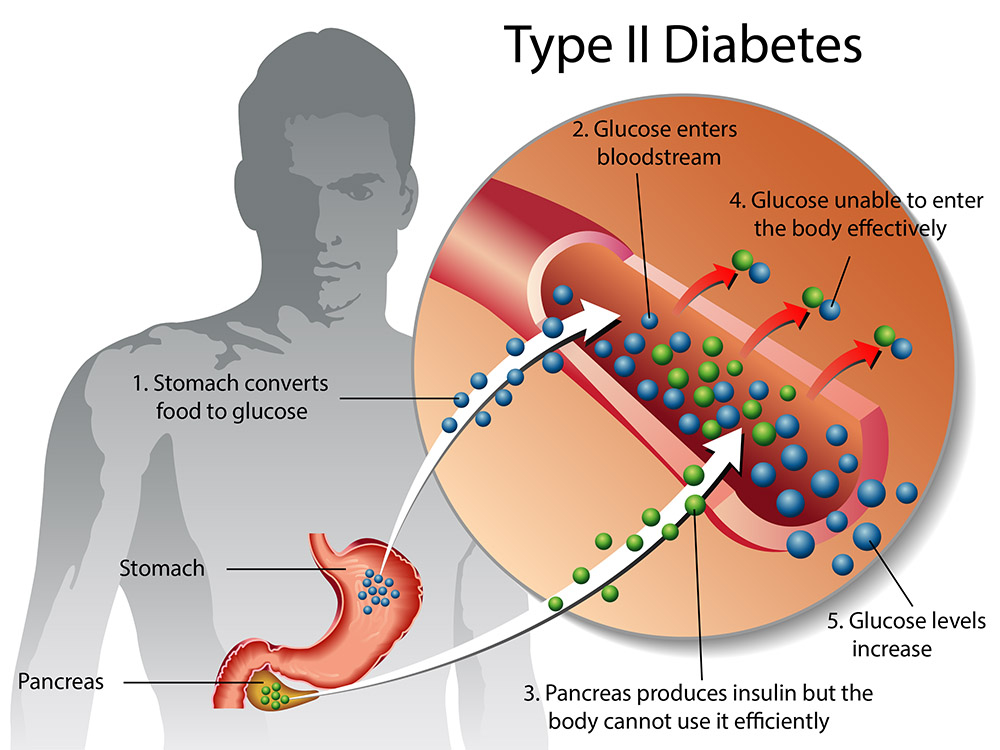
- Type 2 diabetes develops when the body does not make enough insulin or it does not respond to it effectively.
- You need insulin to process the glucose in your food to give you energy.
- Symptoms include feeling tired, hungry or thirsty, and passing more urine.
- Lack of physical activity, being overweight and a poor diet increase the risk of type 2 diabetes.
- Keeping active, with a healthy diet and weight, can help prevent or delay it.
What is type 2 diabetes?
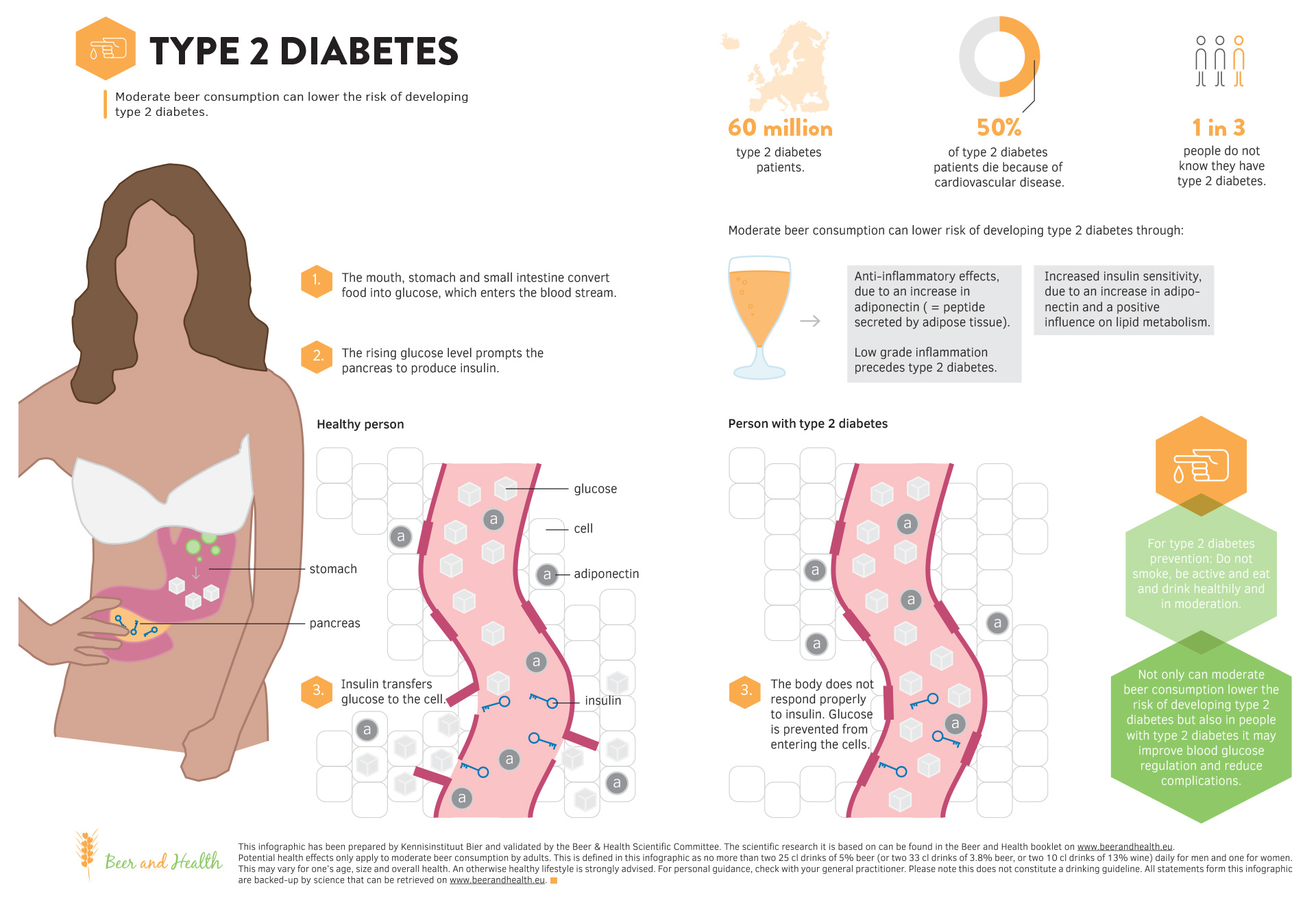
Type 2 diabetes develops when the body does not use insulin efficiently and gradually loses the ability to make enough insulin. Insulin is a hormone that controls the amount of glucose in the blood. Insulin helps glucose produced by the digestion of carbohydrates move from the blood into the body’s cells where it can be used for energy.
In type 2 diabetes, the body’s cells do not respond effectively to insulin. This is known as insulin resistance. it causes glucose to stay in the blood, leading to a higher than normal level of glucose in the blood (known as hyperglycaemia).
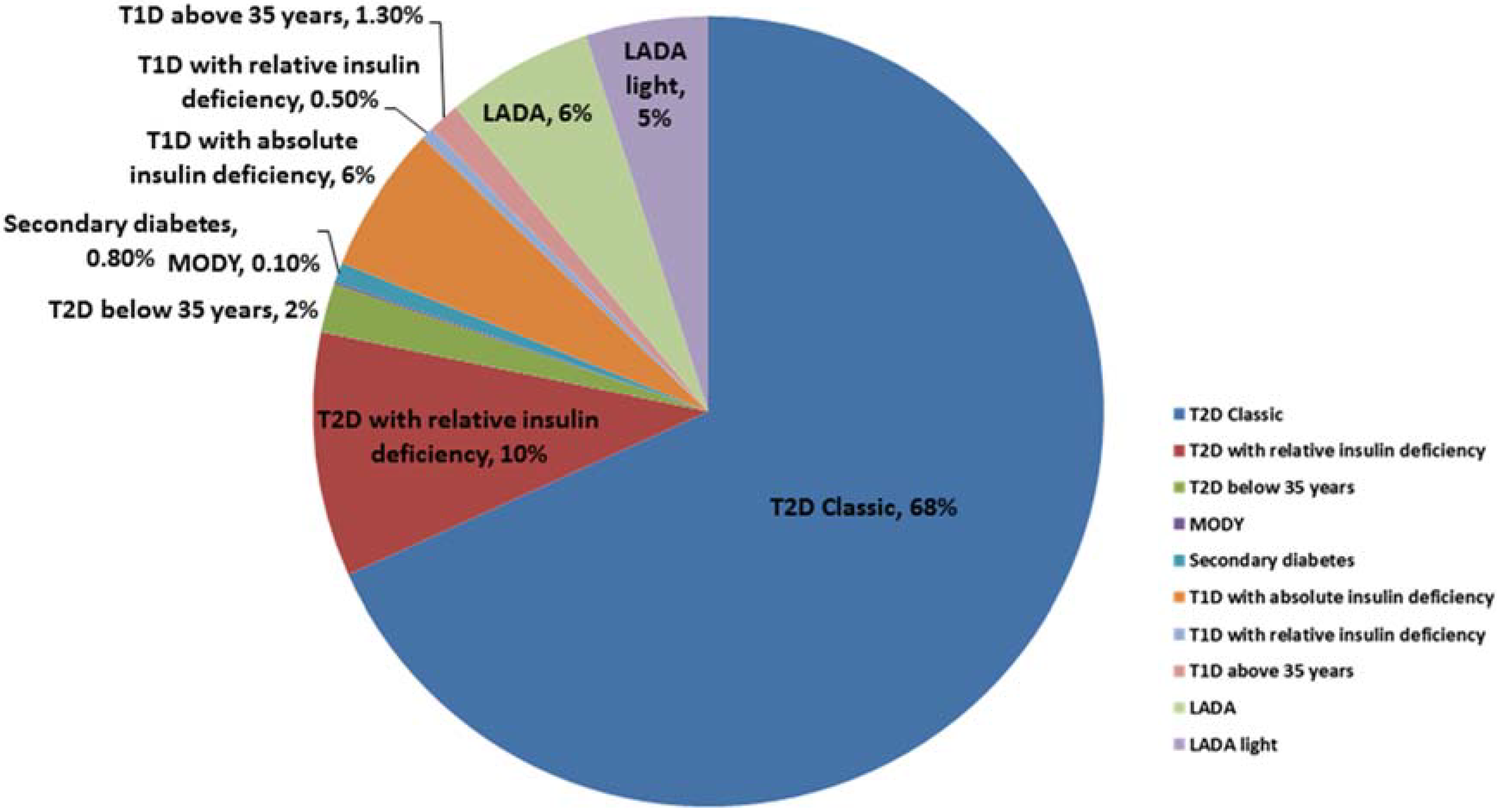
What is the difference between type 1 and type 2 diabetes?
In type 1 diabetes, people produce little or no insulin, as the insulin-producing cells have been destroyed by the body’s immune system. Type 1 diabetes is an auto-immune disease.
In type 2 diabetes, the body may make enough insulin early in the disease, but doesn’t respond to it effectively. As type 2 diabetes progresses, the pancreas gradually loses the ability to produce enough insulin. Type 2 diabetes is associated with inherited factors and lifestyle risk factors such as being overweight or obese, poor diet, and insufficient physical activity.
What is pre-diabetes?
Pre-diabetes means your blood sugar levels are higher than normal, but not high enough to meet a diagnosis of type 2 diabetes. Without lifestyle changes, a person with pre-diabetes is at high risk of going on to develop type 2 diabetes.
What are the first symptoms of type 2 diabetes?
Many people with type 2 diabetes do not experience any symptoms at first and it may go undiagnosed for years. If they do have symptoms, these may include:
- being very thirsty
- passing more urine
- feeling tired
- feeling hungry
- having cuts that heal slowly
Over time, diabetes can lead to complications, which can then cause other symptoms.
Blood glucose testing is important for detecting pre-diabetes and type 2 diabetes before complications arise.
What causes type 2 diabetes?
The exact cause of type 2 diabetes is not known. However, risk factors for developing type 2 diabetes include:
- family history of type 2 diabetes
- being overweight or obese, especially with excess weight around the waist
- a low level of physical activity
- poor diet
- being over 55 years of age
- for women — having had gestational diabetes
- for women — having polycystic ovarian syndrome
- for women — having had a baby weighing over 4.5kg
Certain groups of people are more likely to get type 2 diabetes, including:
- Aboriginal and Torres Strait Islander people
- people with Pacific Islander, Southern European or Asian backgrounds
How is type 2 diabetes diagnosed?
If your doctor suspects you have diabetes, you will probably need to have a blood test to assess your glucose level. It is important for diabetes to be diagnosed early, whether it’s type 1 or type 2 diabetes. That way, it can be better controlled and complications can be avoided or minimised.
During a test, blood is taken from a vein and sent to a pathology lab. The tests that can be done include:
- a fasting blood glucose test — fasting is required for at least 8 hours, which may mean not eating or drinking (except water) overnight
- an oral glucose tolerance test (OGTT) — after fasting for 8 hours, you have a blood glucose test, then you drink a sugary drink and then have another blood test done 1 and then 2 hours later
- HbA1c — this blood test shows your average blood glucose levels over a period of time — it does not involve fasting beforehand
How is type 2 diabetes managed?
Type 2 diabetes is managed by lifestyle changes first, but often medicines will be needed as well. It also involves learning to control and monitor your diabetes with the help of your doctor.
Lifestyle changes for type 2 diabetes
Following a healthy lifestyle is very important in managing type 2 diabetes, and can reduce or delay the need for medications and help prevent complications. The recommendations are:
- follow a healthy diet
- be physically active
- lose weight if you are overweight or obese
- quit smoking
- limit alcohol consumption
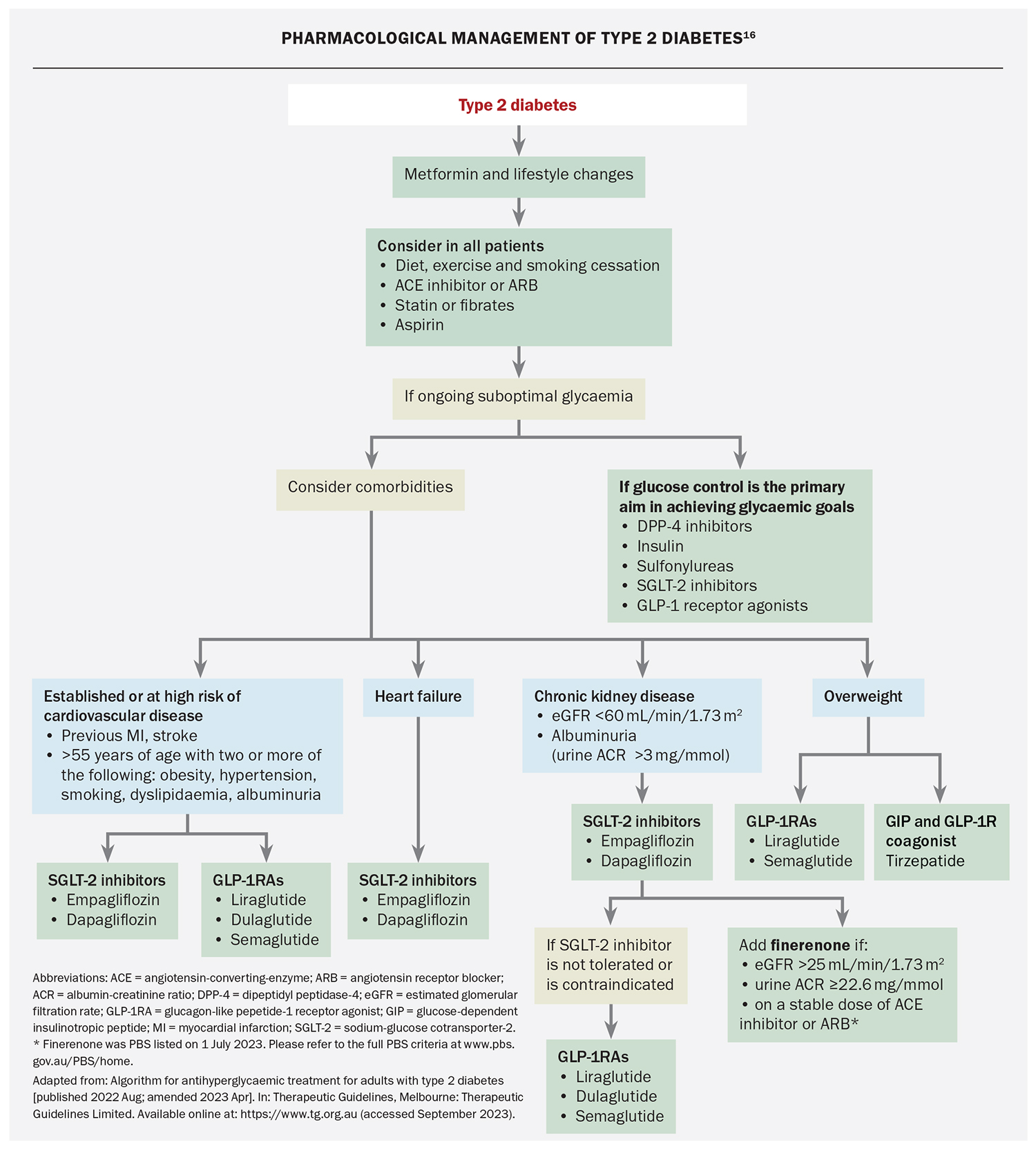
Medicines for type 2 diabetes
There are many types of diabetes medications and they work in different ways to control blood glucose. If you have diabetes, over time it can change, meaning your medications may need to change too. For example, you may need more than one medication to control your blood glucose levels. Some people with type 2 diabetes may eventually need insulin to manage their condition.
If you are living with type 2 diabetes you can join the National Diabetes Services Scheme (NDSS) for free to access a range of resources, support services and subsidised diabetes products. Visit Diabetes Australia for information and resources.
Healthy eating for type 2 diabetes
A dietitian or your doctor will be able to advise you on what to eat to meet your nutritional needs and control your blood sugar. Your doctor should be able to refer you to a registered dietitian for personalised advice.
Eating healthy foods with a low glycaemic index (GI) can help to optimise your blood sugar levels. This includes wholegrain breads, minimally processed breakfast cereals like rolled or steel cut oats, legumes, fruit, pasta and dairy products.
Avoid high-carbohydrate, low-nutrient foods such as cakes, lollies and soft drinks, and eat a diet low in saturated fat.
You should eat at regular times of the day and may also need snacks. Try to match the amount of food you eat with the amount of activity you do, so that you don’t put on weight.
If you are overweight or obese, losing even 5-10 per cent of your body weight can significantly improve blood sugar control.
Can type 2 diabetes be cured?
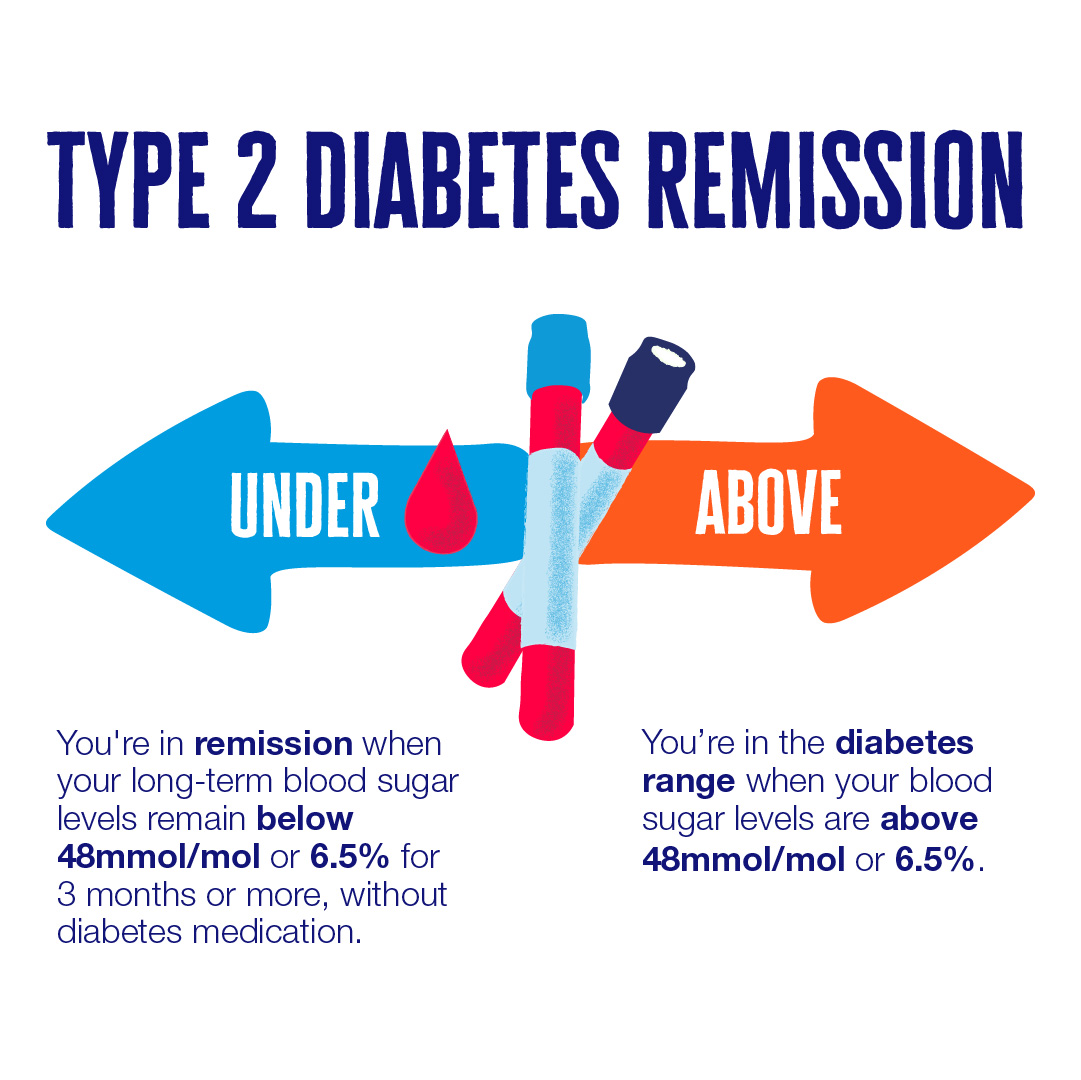
Type 2 diabetes cannot be cured, but people with the condition may be able to manage their type 2 diabetes through lifestyle changes and, if needed, diabetes medications to control blood sugar levels.
It’s also emerging that some people who are overweight or obese can put their type 2 diabetes into remission by losing a substantial amount of weight, especially early in their diagnosis. Their blood sugar measurements return to healthy levels below the diabetes range. It’s not a permanent solution, and diabetes could come back, so it needs to be maintained. However, many people were still in remission 2 years later. This should only be tried under the supervision of your doctor.
When should I see my doctor?
If you have any of the symptoms above, you should make an appointment with your doctor to discuss them since they might indicate undiagnosed type 2 diabetes.
Your doctor will look at your symptoms, review any risk factors you have for type 2 diabetes and they will recommend you be tested if needed.
Even if you don’t have symptoms, all Australians should be screened for type 2 diabetes, every 3 years, starting at 40 years of age. Aboriginal and Torres Strait Islander peoples should start screening at age 18. Your GP should carry out this screening. It may involve reviewing your risk factors only, or you may need a blood test
Can type 2 diabetes be prevented?
Unlike type 1 diabetes, type 2 diabetes can be prevented or delayed by:
- maintaining or achieving a healthy weight
- regular physical activity
- eating healthily
What are the complications of type 2 diabetes?
Treating type 2 diabetes is important to prevent long-term complications, such as:
- heart disease
- kidney disease
- stroke
- eye complications
- foot problems
- nerve problems