What is a percutaneous coronary intervention?
A percutaneous coronary intervention (PCI) is used to treat the symptoms of coronary artery disease, which is narrowing of the coronary arteries (blood vessels that supply your heart muscle with oxygen).
A PCI is a procedure to widen or unblock an artery using a small inflatable balloon. A stent (metal mesh tube) is usually used to hold the artery open.
What are the benefits of a PCI?
Having a PCI should improve the flow of blood without you having to have open heart surgery.
You should get less pain. A PCI may also improve your breathing if blocked or narrowed arteries are causing you to be short of breath.
Sometimes a PCI can be used to treat an artery during or soon after a heart attack. In this case, you may live longer after a PCI and it may reduce the risk of you having another heart attack.
Are there any alternatives to a PCI?
For some people it may be possible to have a coronary bypass operation.
Coronary artery disease can be treated using medication to relieve the symptoms and to help prevent the disease from getting worse.
What will happen if I decide not to have a PCI?
Your angina may stay stable and controlled for many years. You will need to continue with medication.
Without a PCI, you may get more symptoms of angina. If you have recently had a heart attack or unstable angina (acute coronary syndrome) there may be a higher risk of you having another heart attack if you do not have a PCI.
What does the procedure involve?
A PCI usually takes 30 minutes to 2 hours.
Your cardiologist will use antiseptic to clean the area where the sheath (a small plastic tube) will be inserted and most of your body will be covered with a sterile sheet.
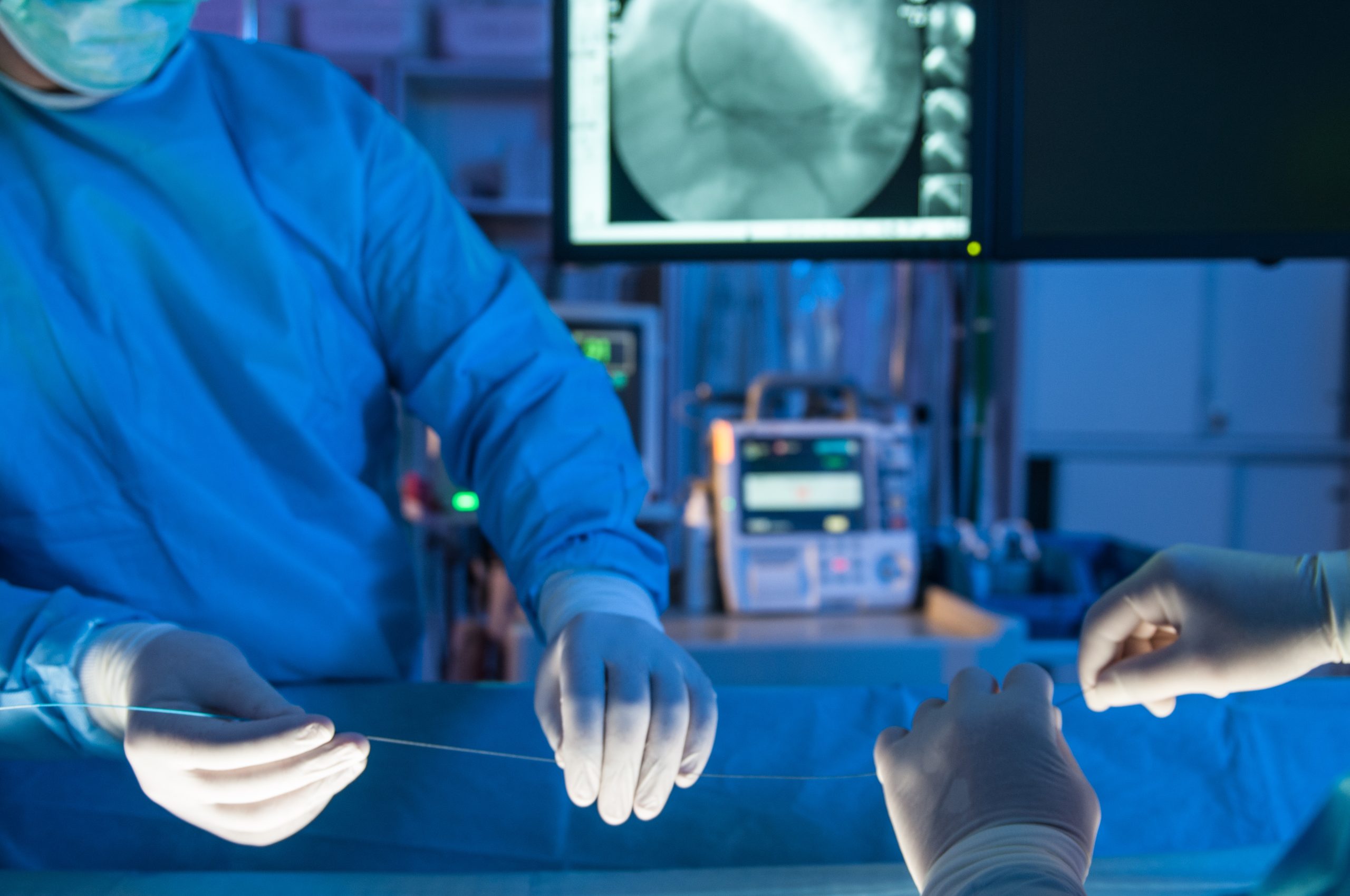
When your cardiologist is satisfied that the sheath is in the right position, they will insert a catheter (long, narrow plastic tube) through the sheath and into your artery.
Your cardiologist will inject dye into the catheter so they can take x-rays to find out exactly where your coronary arteries have narrowed.
Your cardiologist will pass a fine wire down the catheter and through the narrowed part of the artery. They will pass a small tube, with a small inflatable balloon at the end, over the wire and across the narrowed part of the artery. They will inflate the balloon to widen the artery.
In most cases they will also expand a stent inside the artery to hold it open.
Your cardiologist will remove the wire, balloon and catheter. They will remove the sheath when your blood has thickened.
What complications can happen?
Complications during or soon after the procedure
- bruising
- infection
- infection of the stent
- bleeding after the procedure
- developing a collection of blood
- false aneurysm or arteriovenous fistula
- change in heart rhythm
- kidney damage
- allergic reaction to the equipment, materials, medication or dye
- radiation exposure
- blood clot
- lost stent
- blood leaking into the sac that surrounds your heart
- drop in blood pressure
- heart attack
- radial artery spasm
- stroke
Late complications
- stent restenosis, where the artery narrows again
- stent thrombosis, where a blood clot forms in the stent
How soon will I recover?
You should be able to go home the same day or the day after.
Do not have a hot bath for 2 to 3 days. It is important not to do strenuous exercise for about a week.
If you had a stent inserted, you will be on extra blood-thinning medication such as clopidogrel or ticagrelor, so you will be at a higher risk of bleeding.
Regular exercise should improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
If you have high blood pressure or high cholesterol, you will usually need to continue with most of the medication you were on before the procedure.


