Key facts
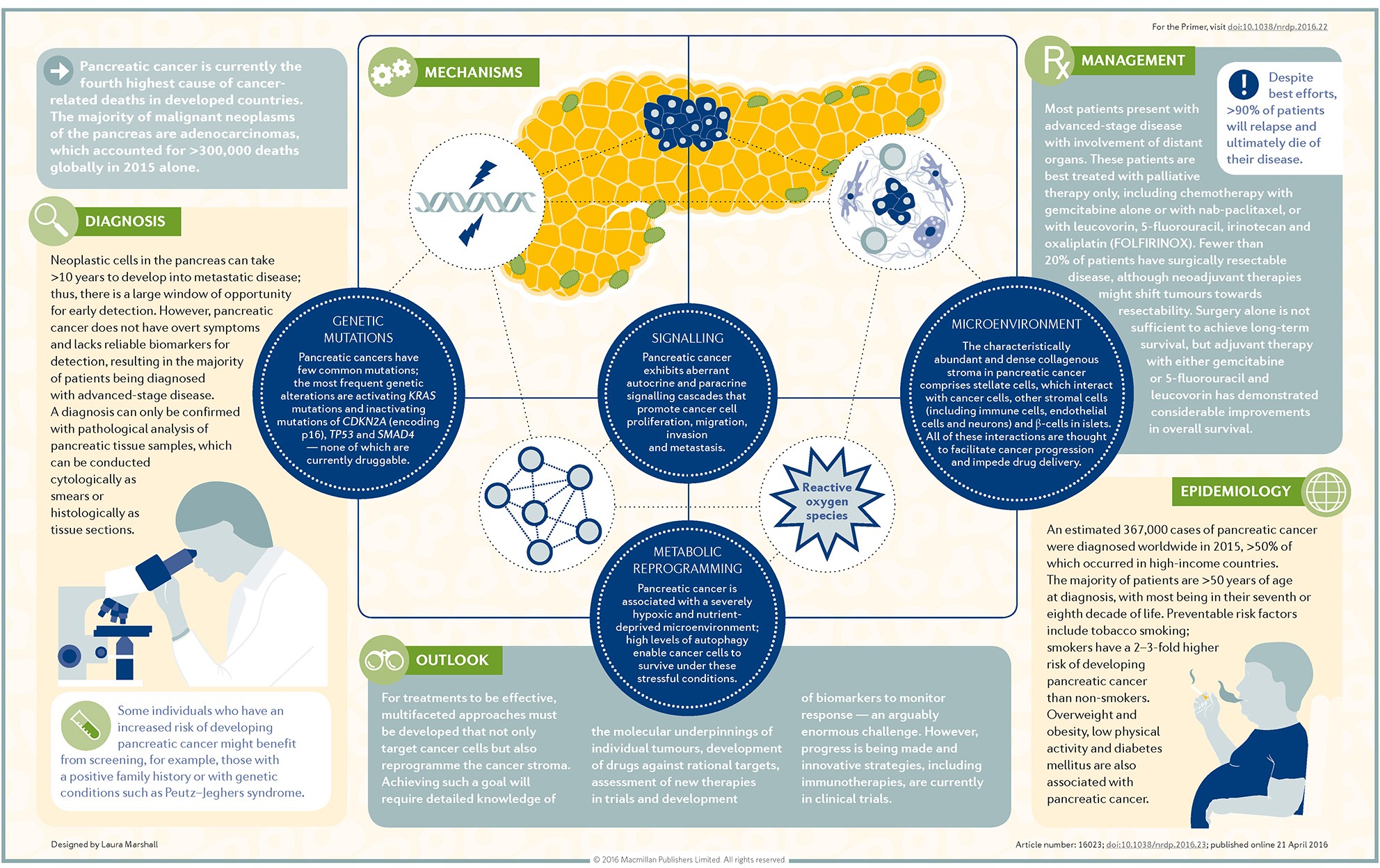
- Pancreatic cancer occurs when abnormal cells in the pancreas grow in an uncontrolled way.
- There are often no symptoms when pancreatic cancer first develops.
- Symptoms that may develop include nausea, abdominal pain, yellow skin and eyes, loss of appetite and unexplained weight loss.
- Depending on the stage of your cancer, you may be offered medicines, chemotherapy, radiation therapy, palliative care, or a combination of these.
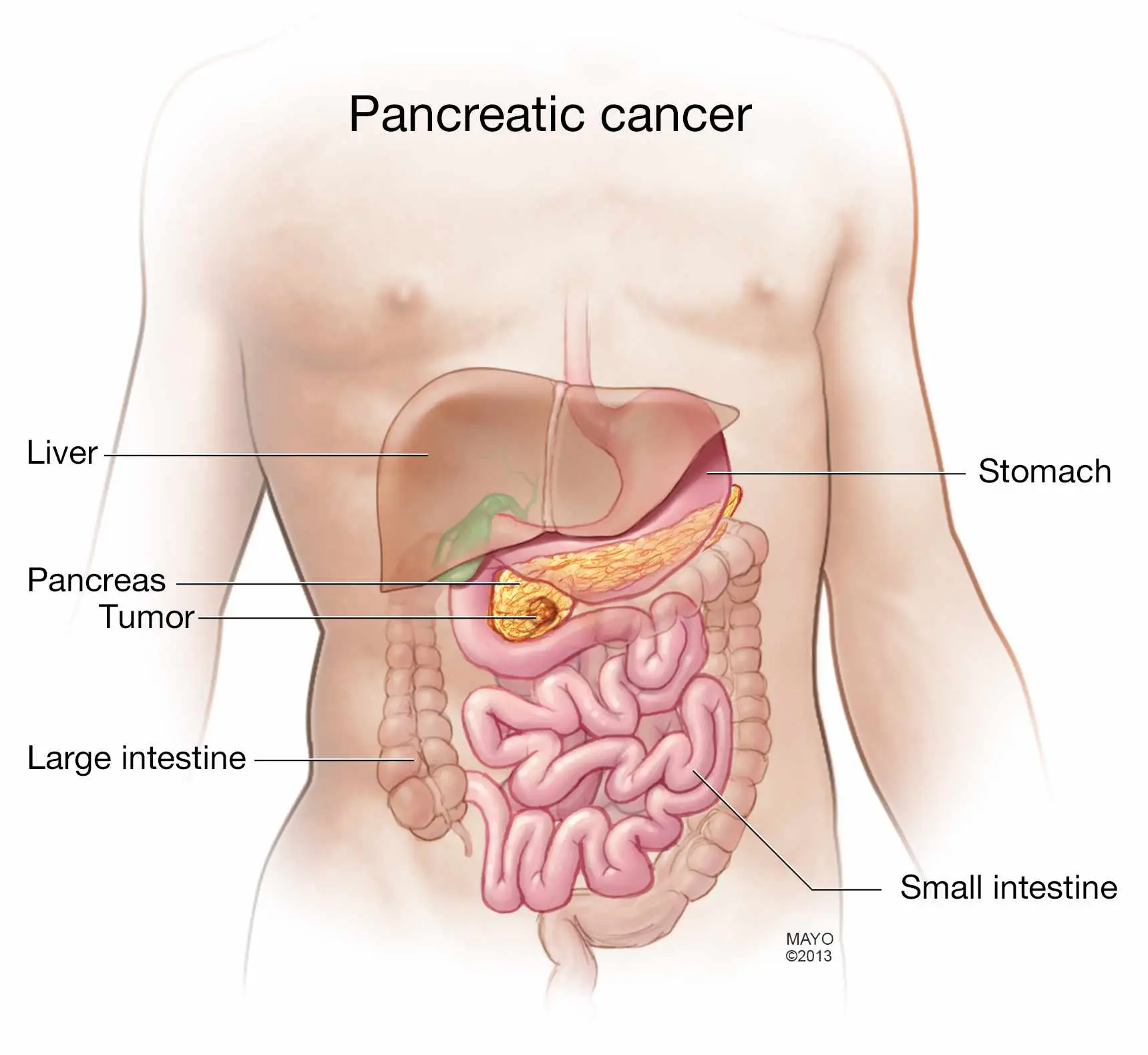
What is pancreatic cancer?
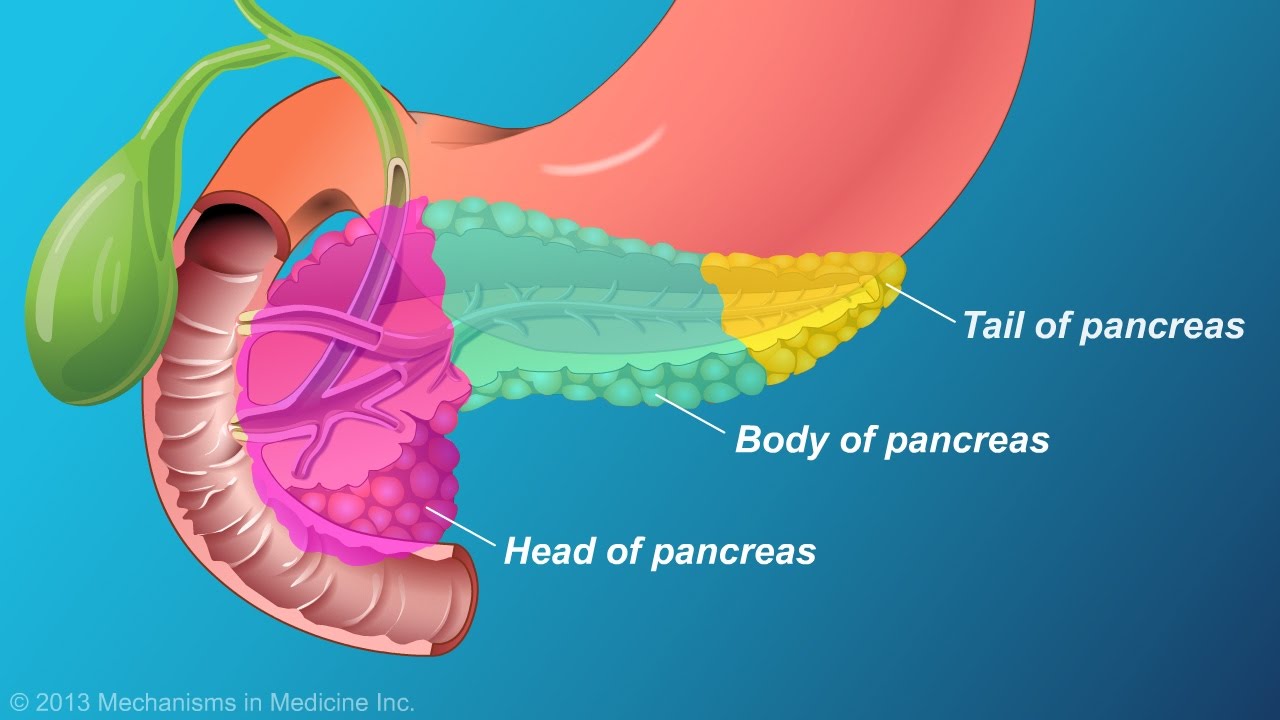
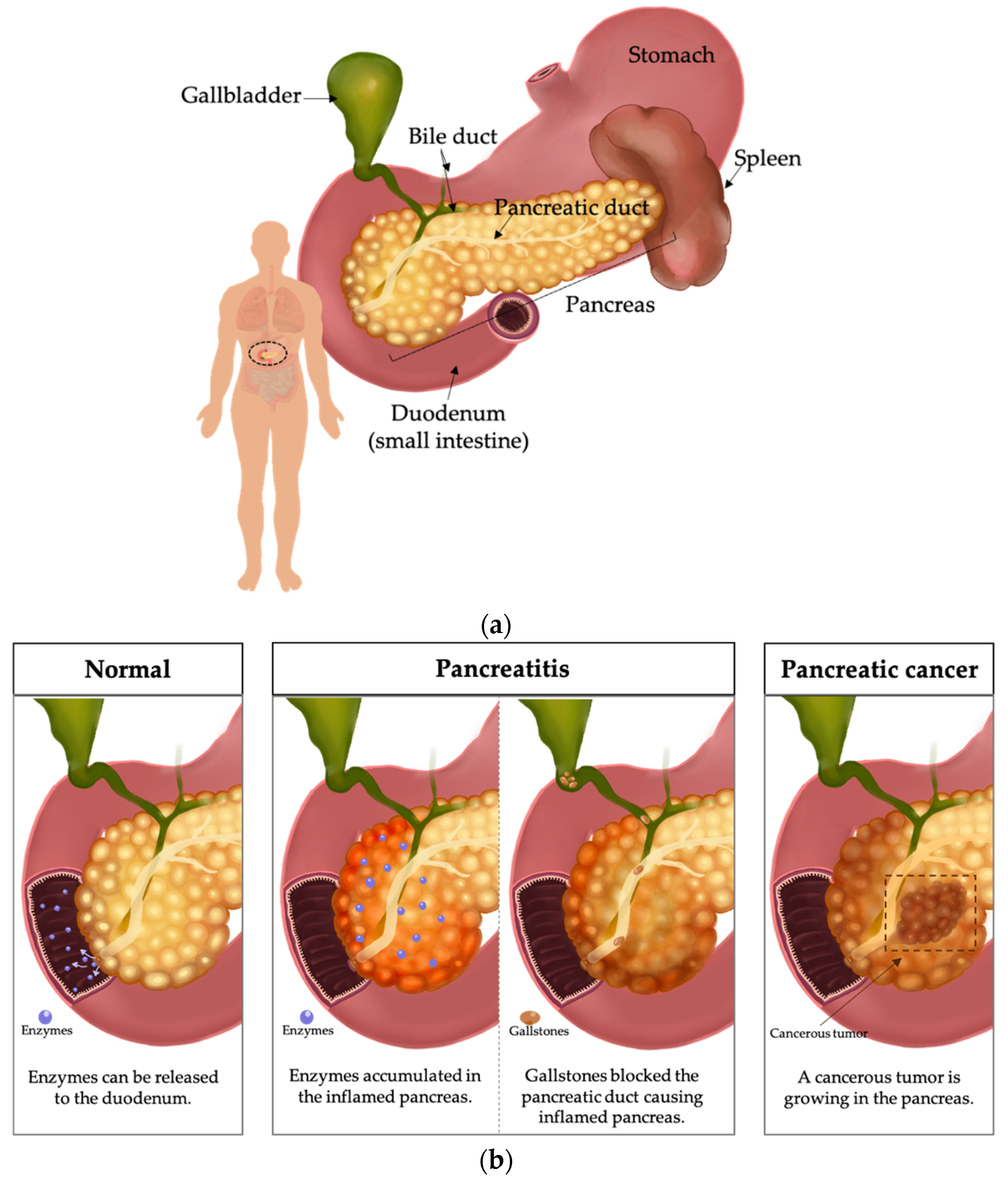
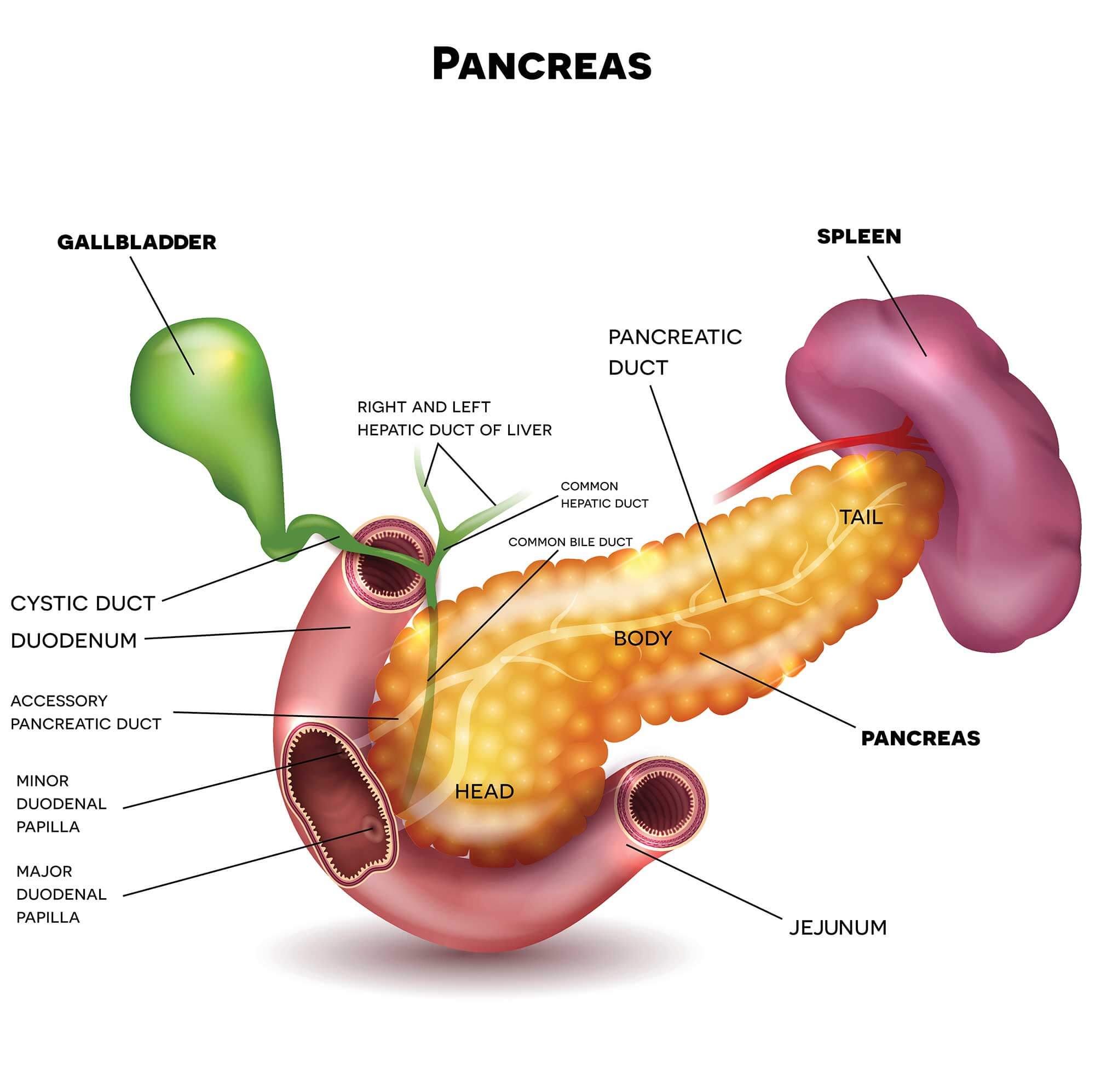
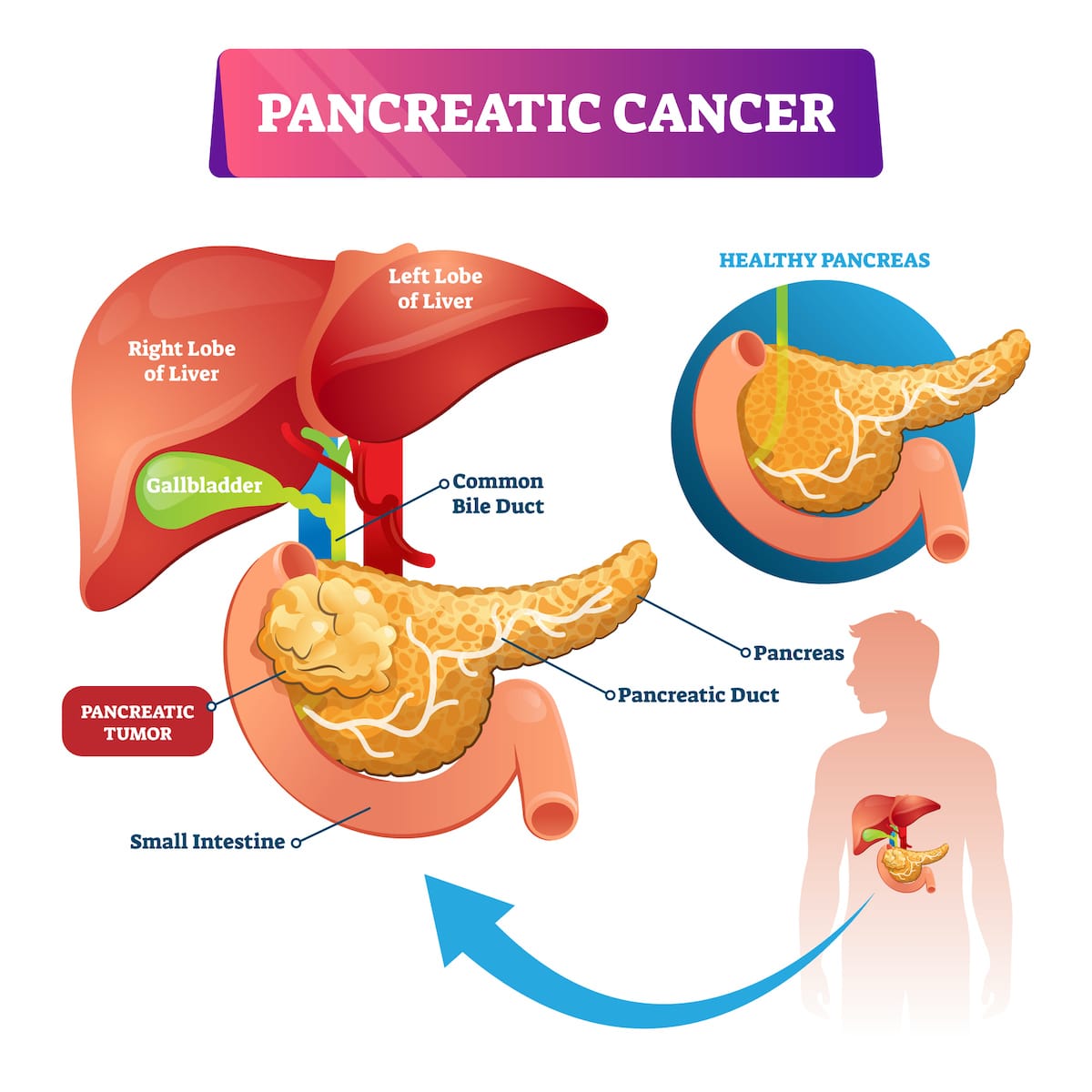
Pancreatic cancer is a cancer of the pancreas. The pancreas is an organ located in the abdomen, near the stomach and small bowel (small intestine). It is a gland, which means that it is an organ that releases chemicals to help the body work.
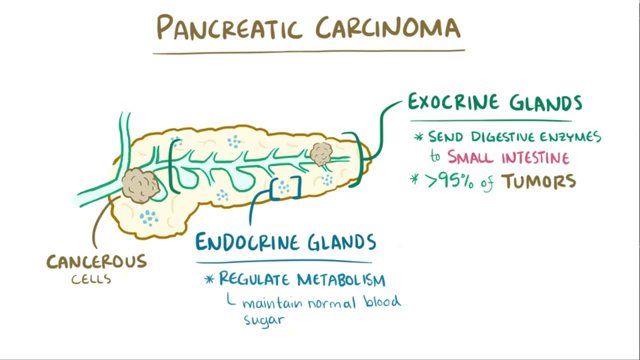
The pancreas releases natural chemicals called enzymes into the small bowel that help digest food. It also releases hormones, including insulin, into the blood stream, to help convert food into energy.
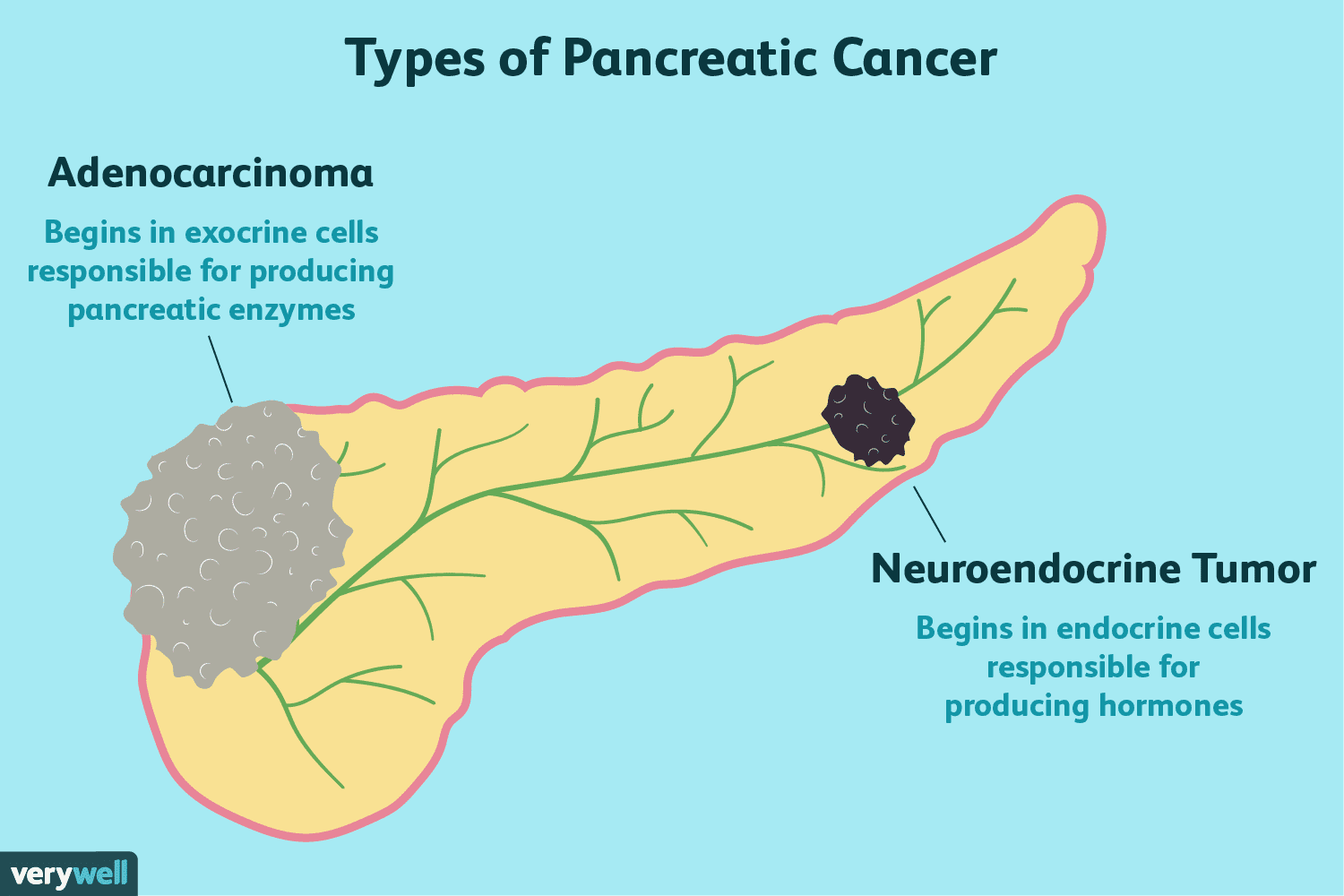
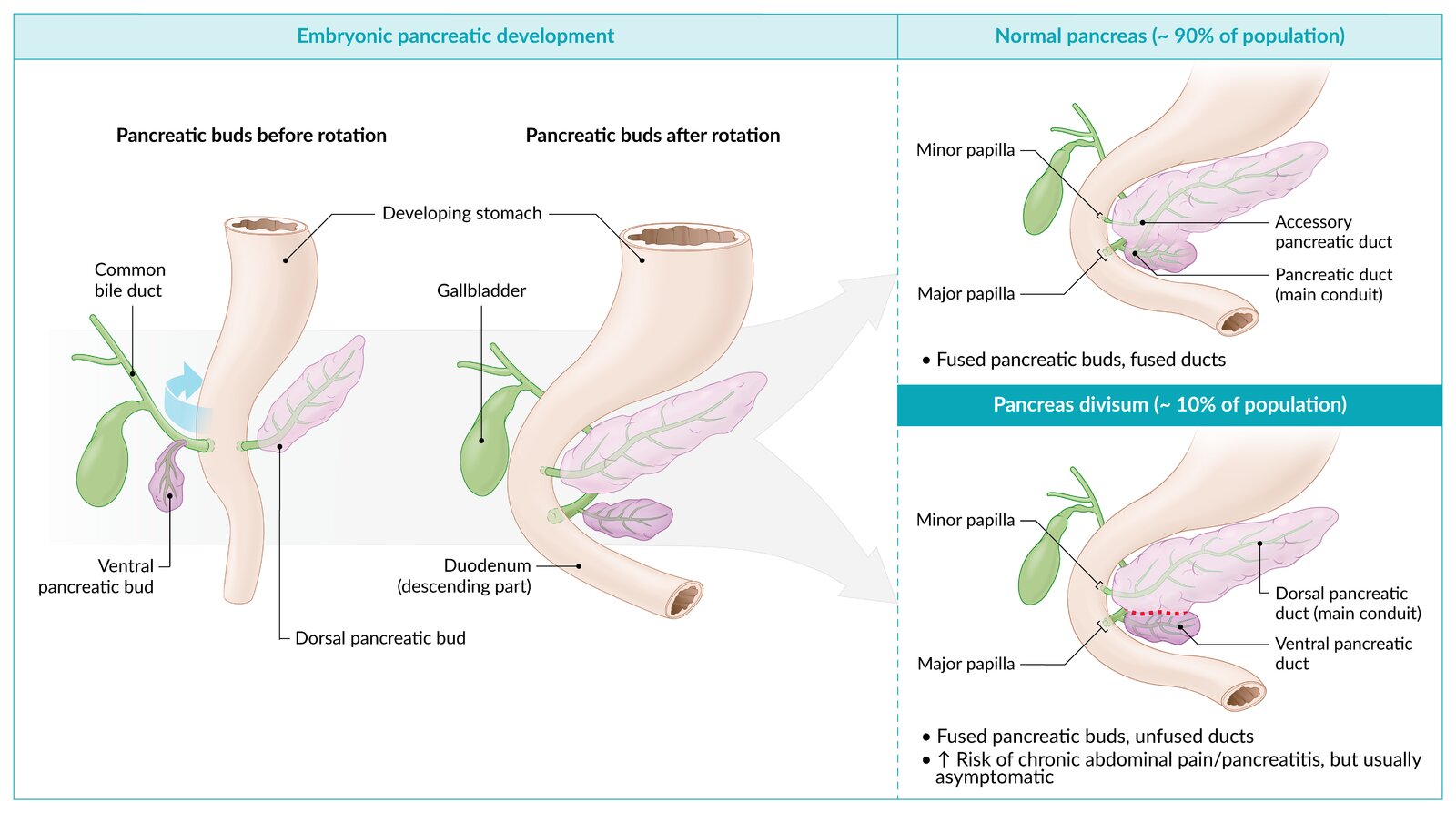
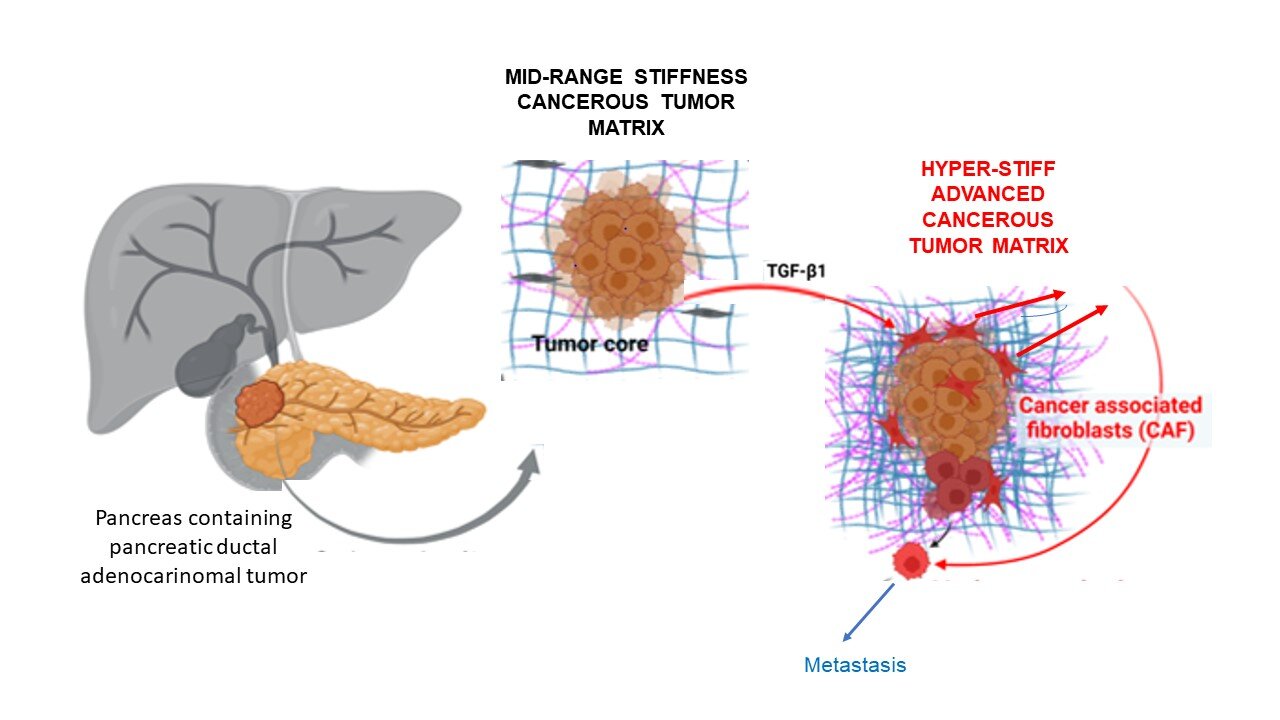
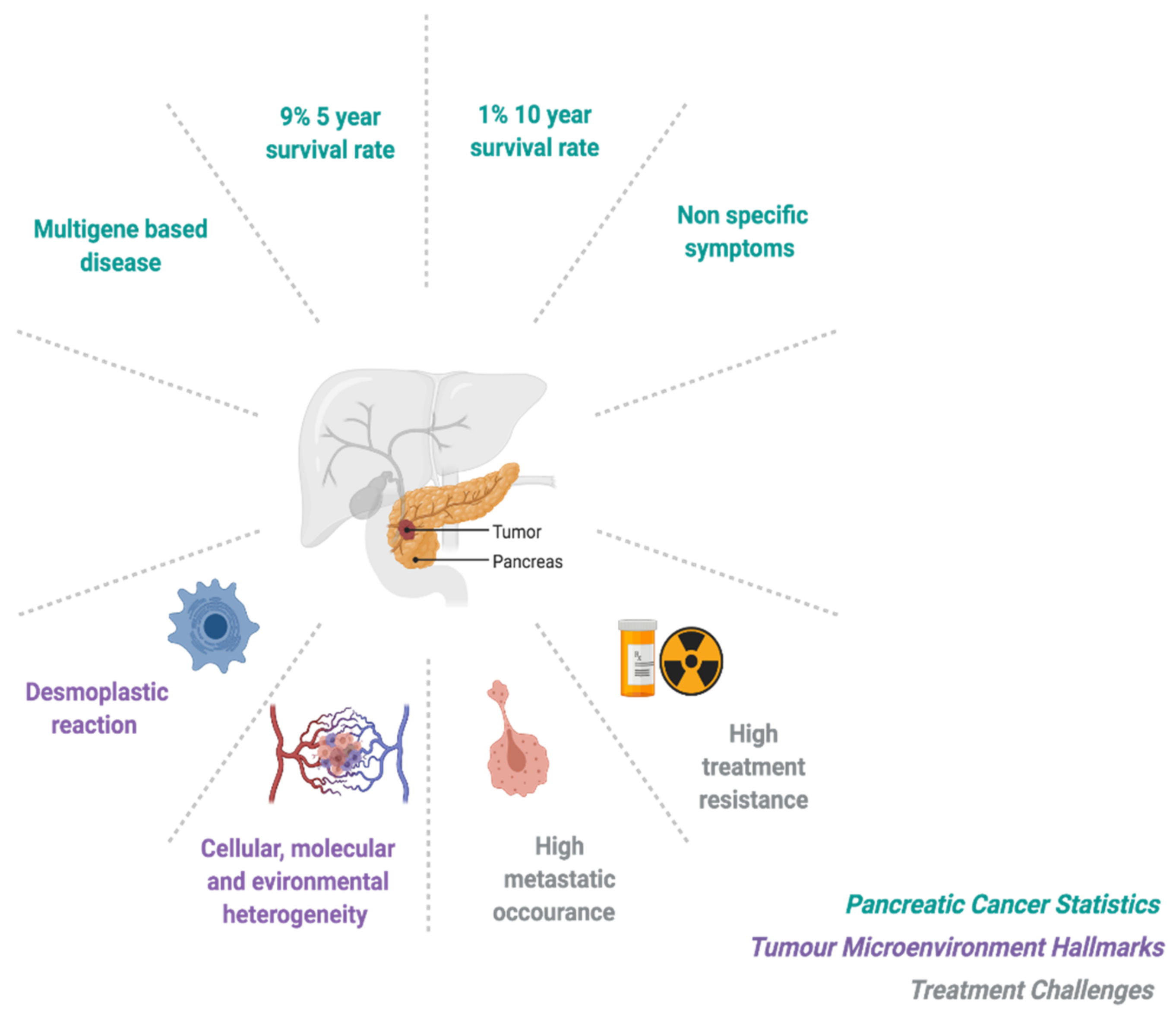
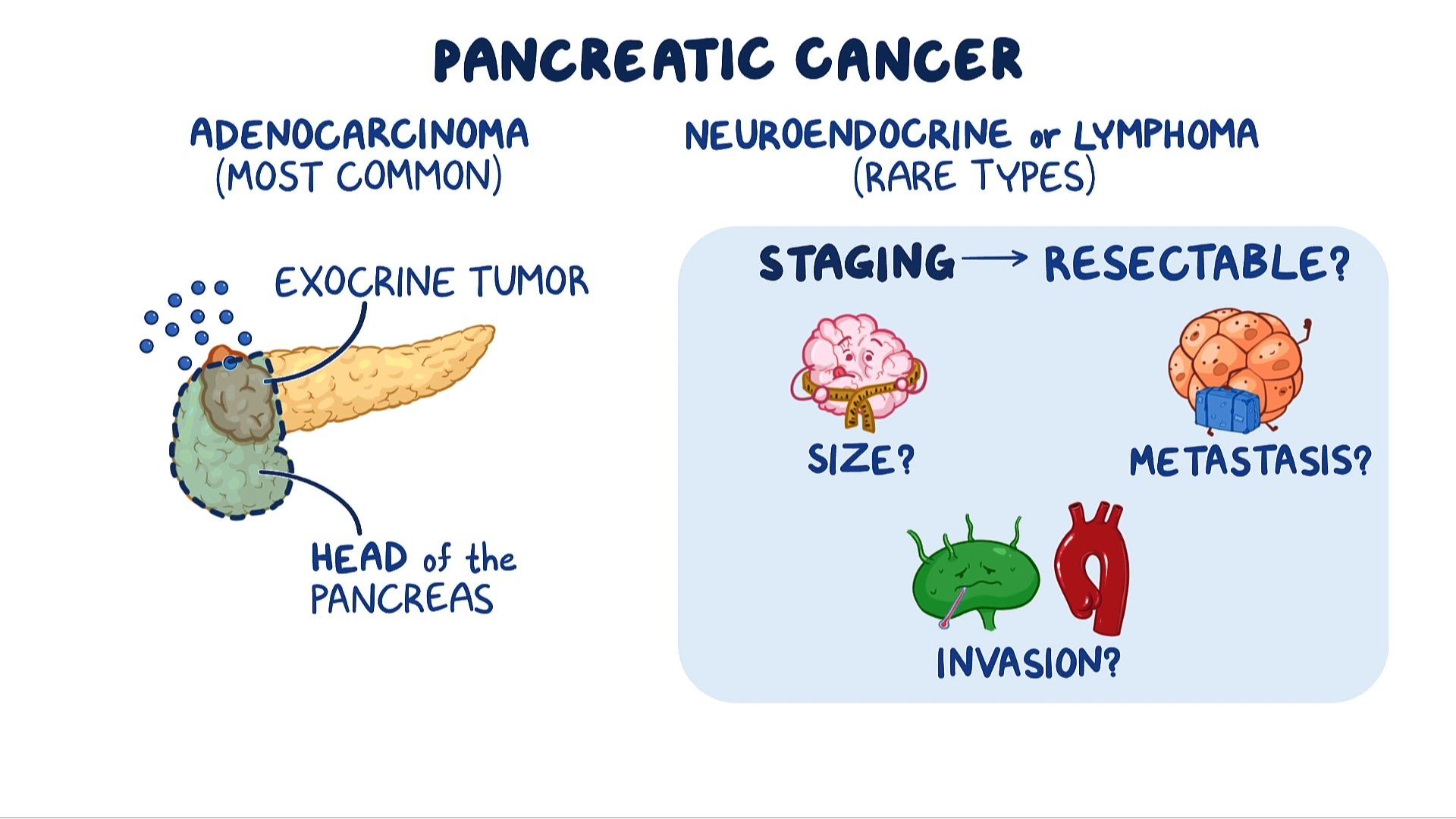
Cancer occurs when cells in the pancreas grow in an uncontrolled way. Most pancreatic cancers start in the cells of ducts of the pancreas (called exocrine pancreatic cancer). Cancer can also start in the hormone-producing cells of the pancreas (called pancreatic neuroendocrine tumours).
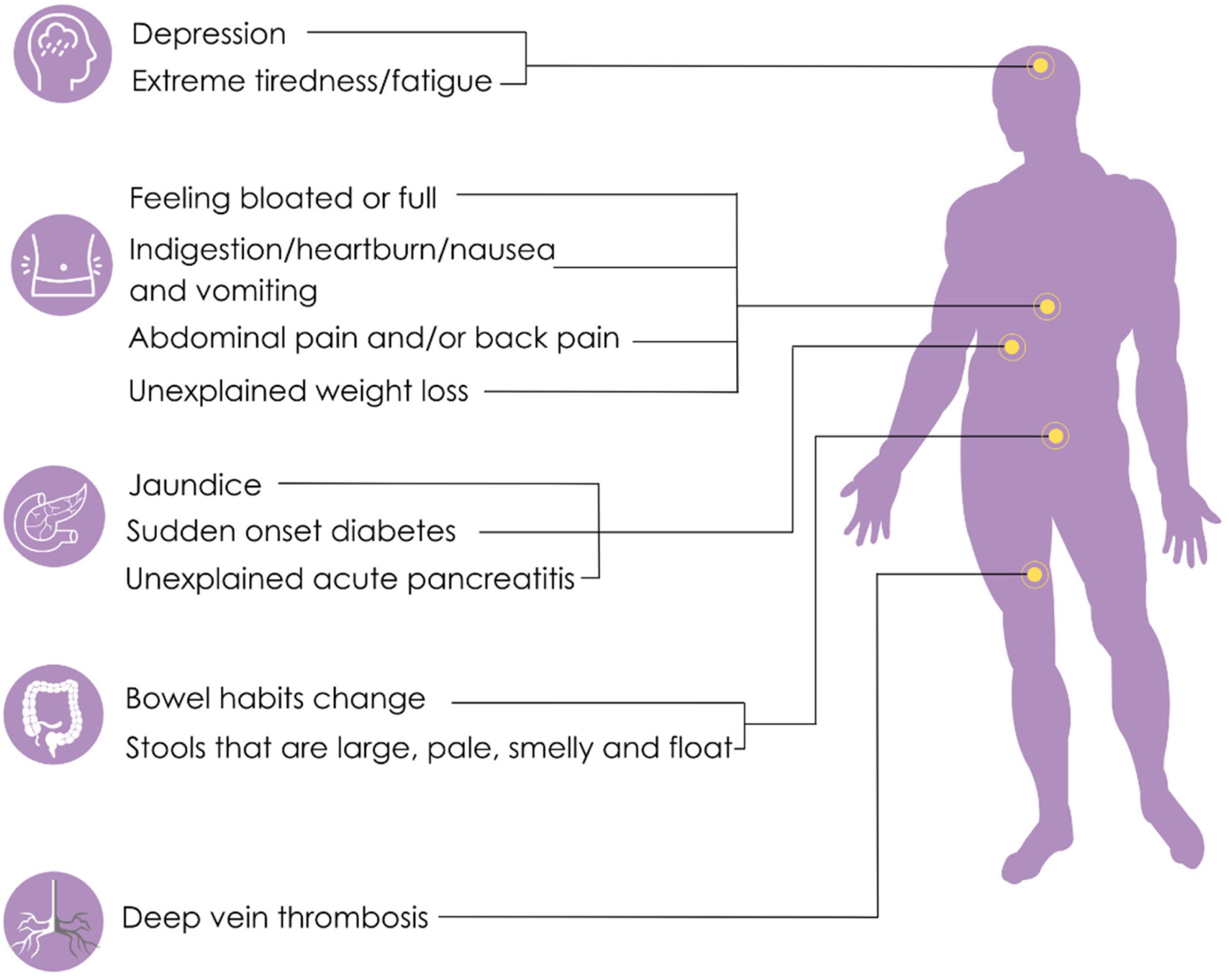
What are the symptoms of pancreatic cancer?
If you have early-stage pancreatic cancer you may not have any symptoms at all. You might not have any symptoms until the cancer grows or spreads to affect other organs.
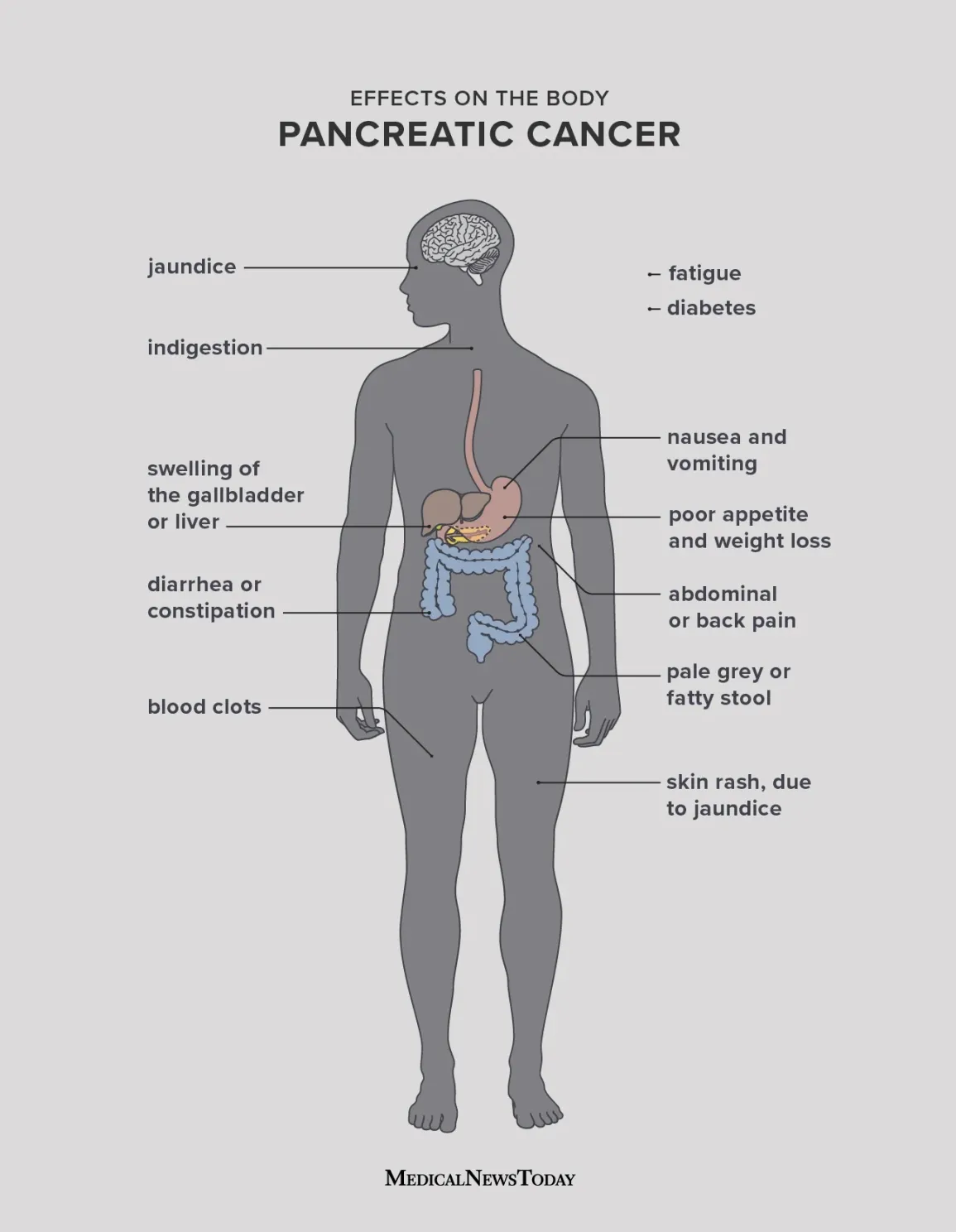
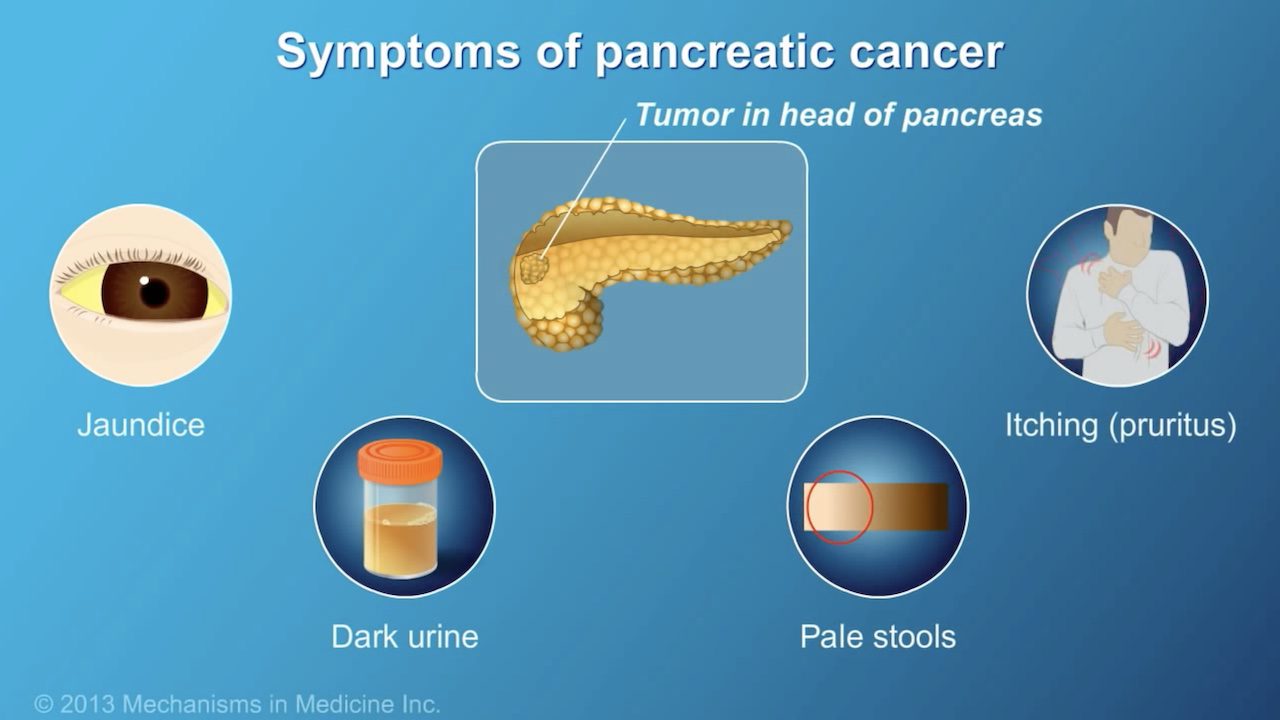
Possible signs and symptoms of pancreatic cancer include:
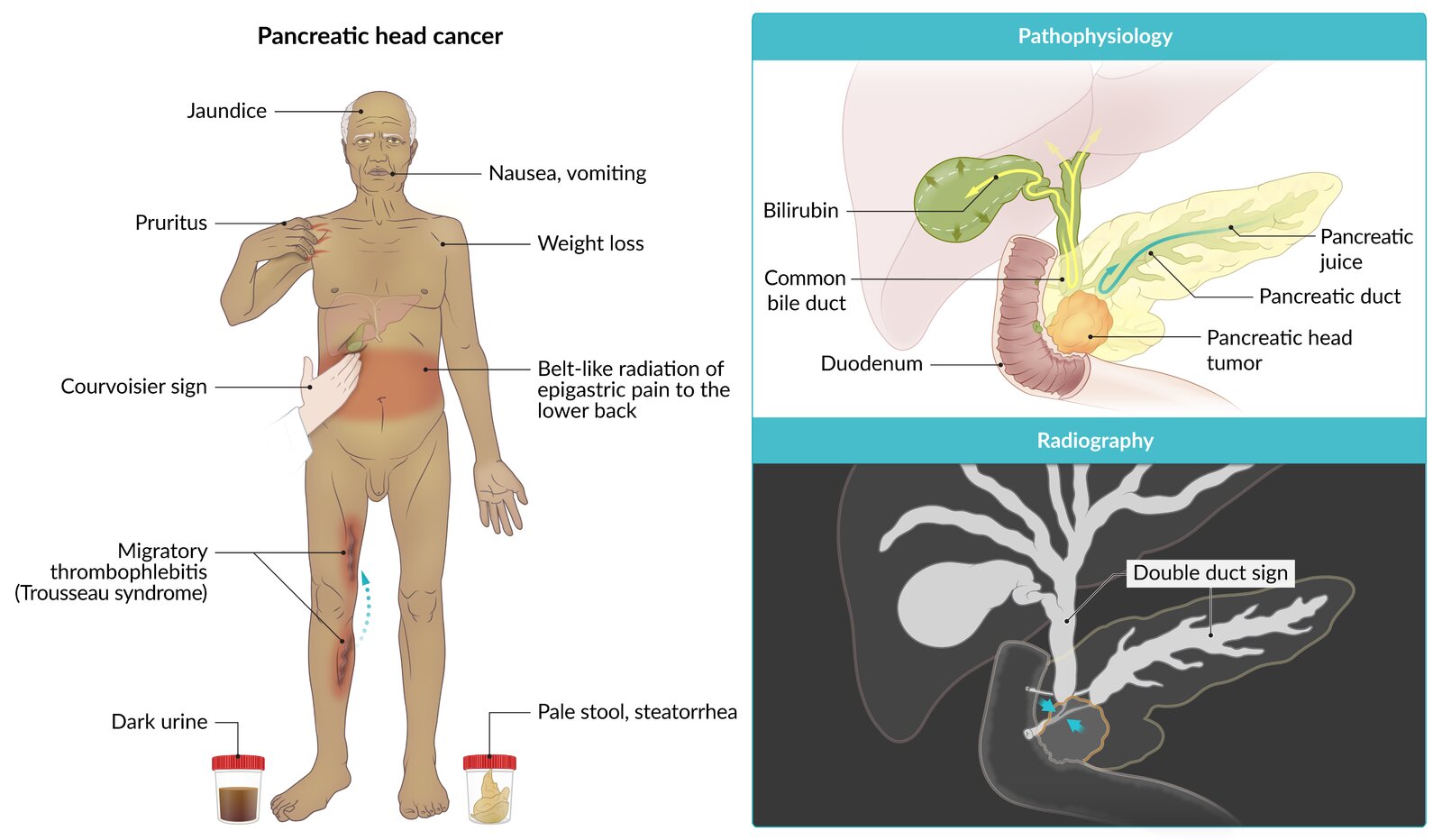
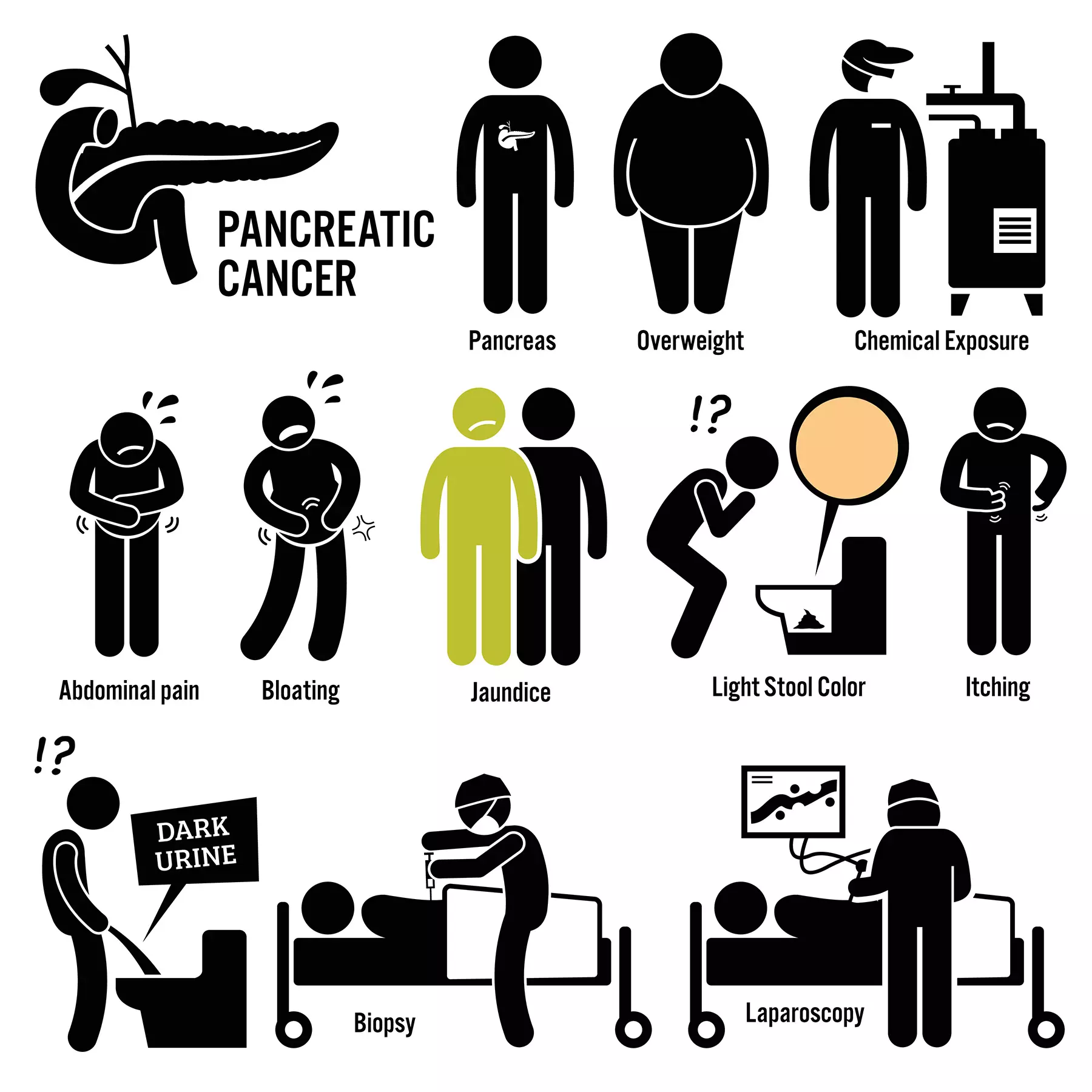
- yellow skin and eyes (jaundice) or dark urine
- loss of appetite
- nausea and vomiting
- changed bowel motions (poo), such as diarrhoea or severe constipation
- pale, greasy poo
- pain in the upper abdomen — you may feel this pain in your back or side or back
Other non-specific cancer symptoms may include:
- fatigue
- unexplained weight loss
What causes pancreatic cancer?
The cause of pancreatic cancer isn’t known, but there are some things that make you more likely to get pancreatic cancer.
Factors that increase your risk include:
- smoking
- obesity
- older age — most people who get pancreatic cancer are older than 60 years old
- long term type 2 diabetes
- excessive alcohol use
- a family history of pancreatic cancer, ovarian cancer or colon cancer and some genetic conditions
- frequent exposure to some chemicals
Some less common medical conditions can also increase your risk:
- chronic (long term) inflammation of the pancreas (pancreatitis)
- certain types of cysts in the pancreas
- stomach infections caused by the bacteria Helicobacter pylori
Research regarding the impact of diet on pancreatic cancer suggests that large amounts of red and processed meats may increase in risk of pancreatic cancer. A diet that includes a greater proportion of fruit and vegetables may decrease the risk.
Smoking and pancreatic cancer
Smoking or chewing tobacco makes you twice as likely to develop pancreatic cancer than non-smokers.
Learn more about quitting smoking.
When should I see my doctor?
You should see your doctor promptly if you have unexplained weight loss, severe abdominal pain, jaundice, or other symptoms such as those listed above that worry you.
There are many medical conditions and illnesses that can cause these symptoms, so having these symptoms does not always mean you have cancer. Your doctor can discuss your symptoms along with your medical history and advise if any special tests are necessary.
How is pancreatic cancer diagnosed?
Your doctor may use a range of tests and techniques to diagnose the cause of your symptoms, such as asking about your symptoms, examining you and referring you for blood tests.
They may then recommend other tests to check if you have pancreatic cancer and if any cancer has spread.
These tests may include:
- a CT scan (computed tomography)
- an MRI (magnetic resonance imaging)
- an ultrasound (including an ultrasound passed through the mouth on the end of a long tube, called an endoscopic ultrasound)
- cholangiopancreatography — a test that uses x-x-rays or MRI to look at the pancreatic ducts and bile ducts
- a PET scan (positron emission tomography) which can show where a cancer has spread
Your doctor may also recommend a biopsy. This involves taking a sample of tissue from your pancreas for testing in a lab. A biopsy can help identify if you have cancer and, depending on the type of biopsy, can check how far it’s spread.
There are different ways your doctor might take a biopsy:
- They may insert a needle into the tissue through the abdominal to take a sample — this is called fine-needle aspiration or needle biopsy. This is done using a form of imaging to guide them.
- They may insert a camera-tipped tube through the mouth down the gut to collect images from the area (endoscopy).
- They may use a form of keyhole surgery known as laparoscopy, which involves making small incisions (cuts) in the abdomen to collect samples and examine the area.
If pancreatic cancer is likely and it seems the tumour could be removed, your doctor may recommend surgery without a biopsy.
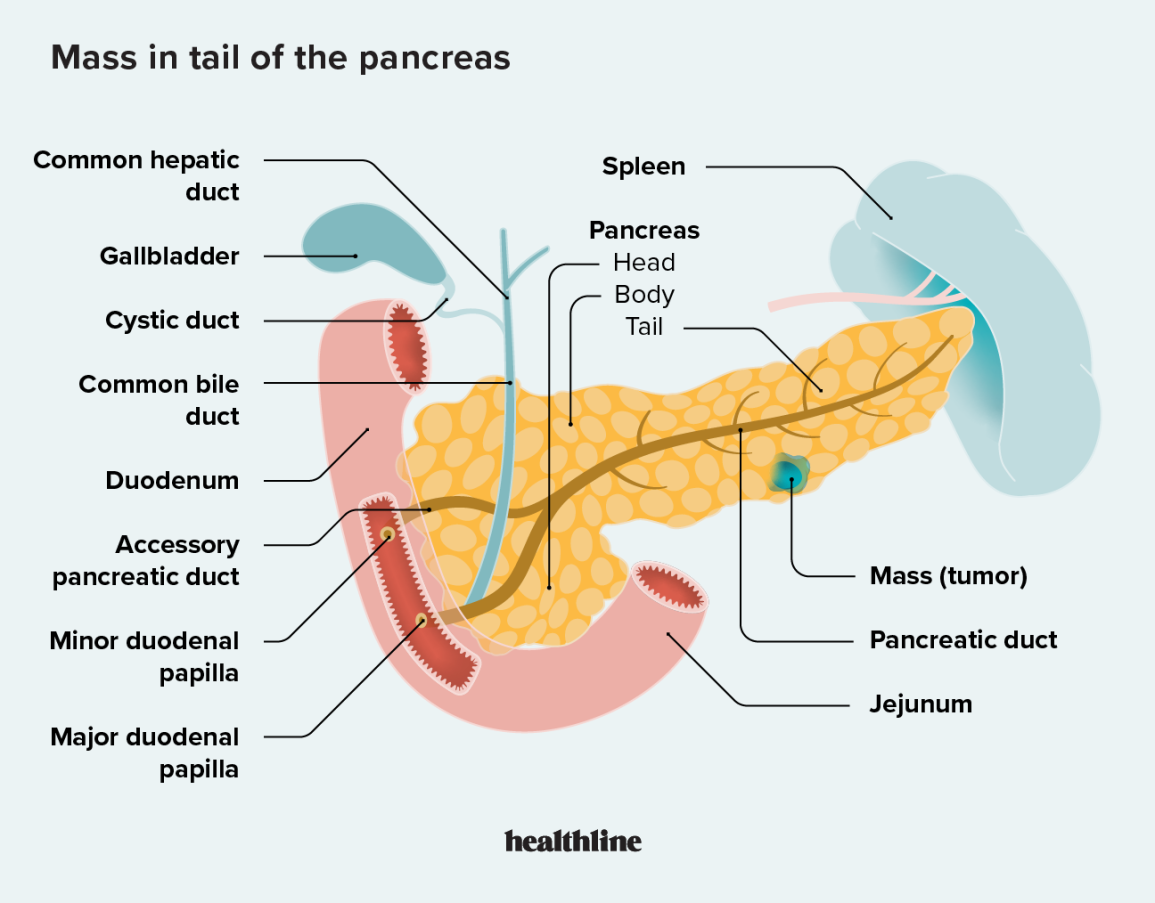
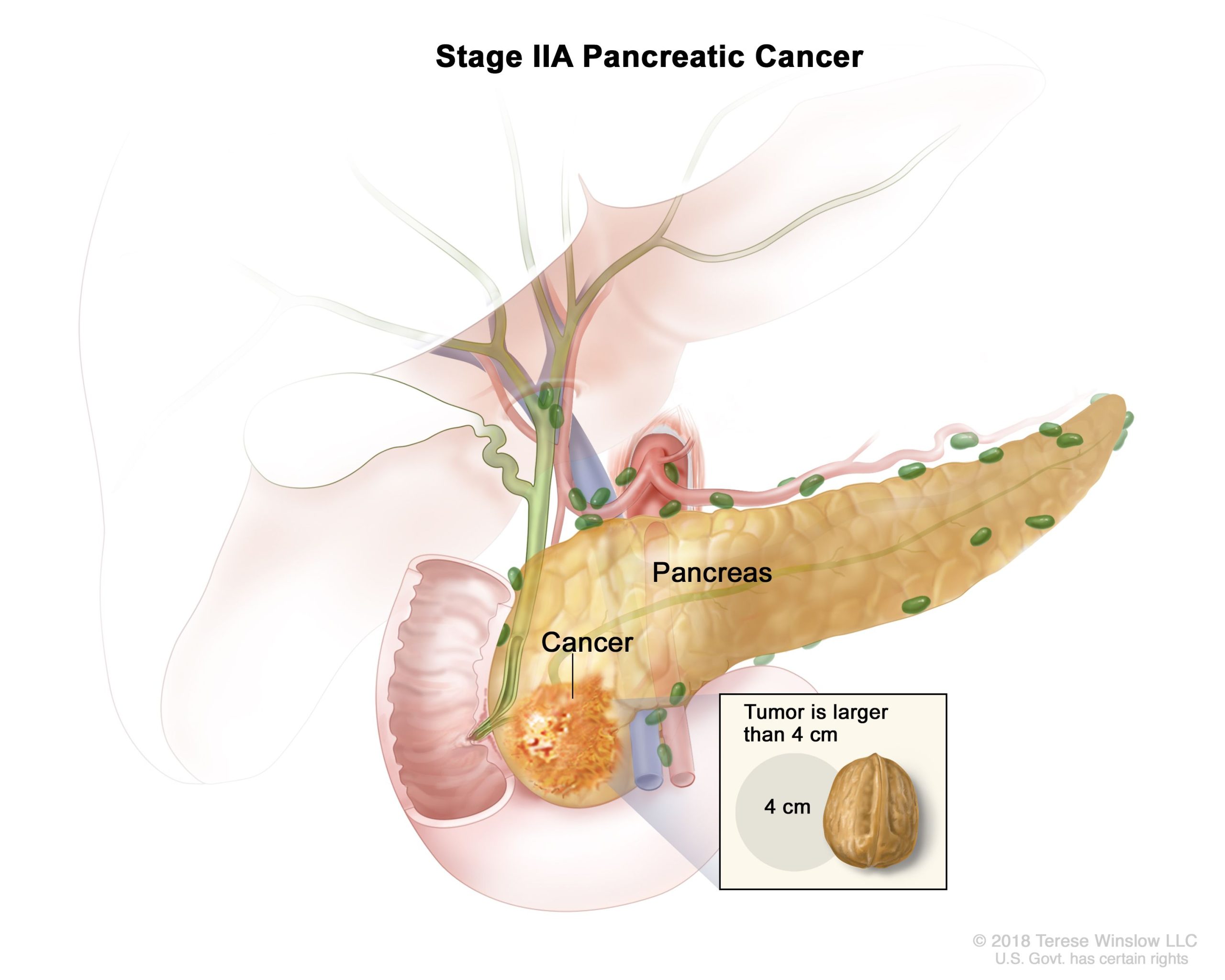
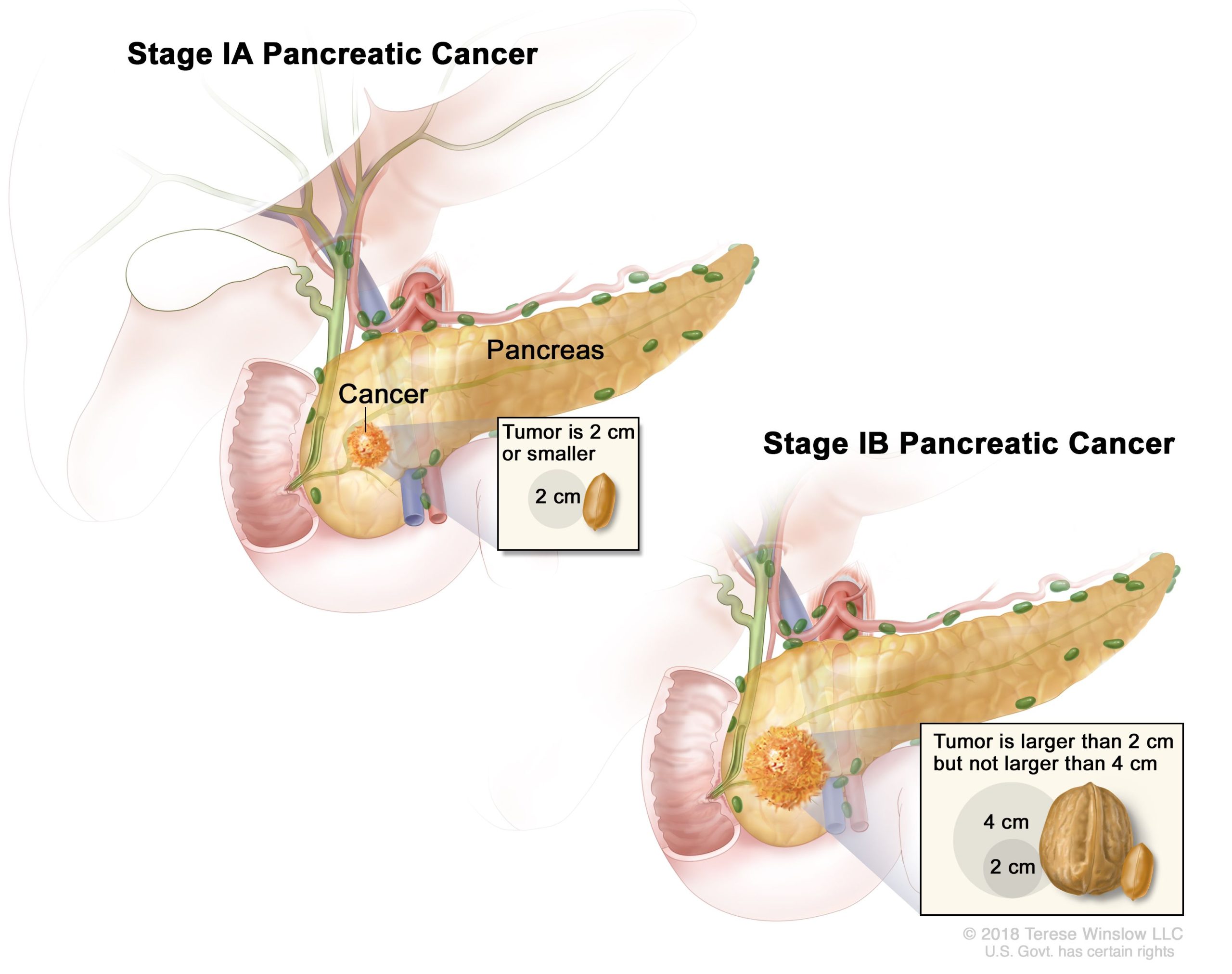
If you are diagnosed with pancreatic cancer, you will probably be given an indication of the stage of the cancer. These stages describe how far the cancer has spread:
- stage I — the cancer is small and only in the pancreas
- stage II —a large cancer in the pancreas and there may be spread to nearby lymph nodes
- stage III — wider spread into major nearby blood vessels or nerves but no metastasis (spread to other organs)
- stage IV —spread to other organs such as the liver, lungs or lining of the abdomen
How is pancreatic cancer treated?
Treatment will depend on the size of the cancer and if it has spread (its stage). It will also depend on where the cancer is, your age, your health and your personal preference.
Treatment options may include one or more of:
- surgery
- endoscopic treatment
- chemotherapy
- radiotherapy
Your doctor may recommend palliative care options to reduce your symptoms and improve your quality of life instead of attempting to remove the tumour.
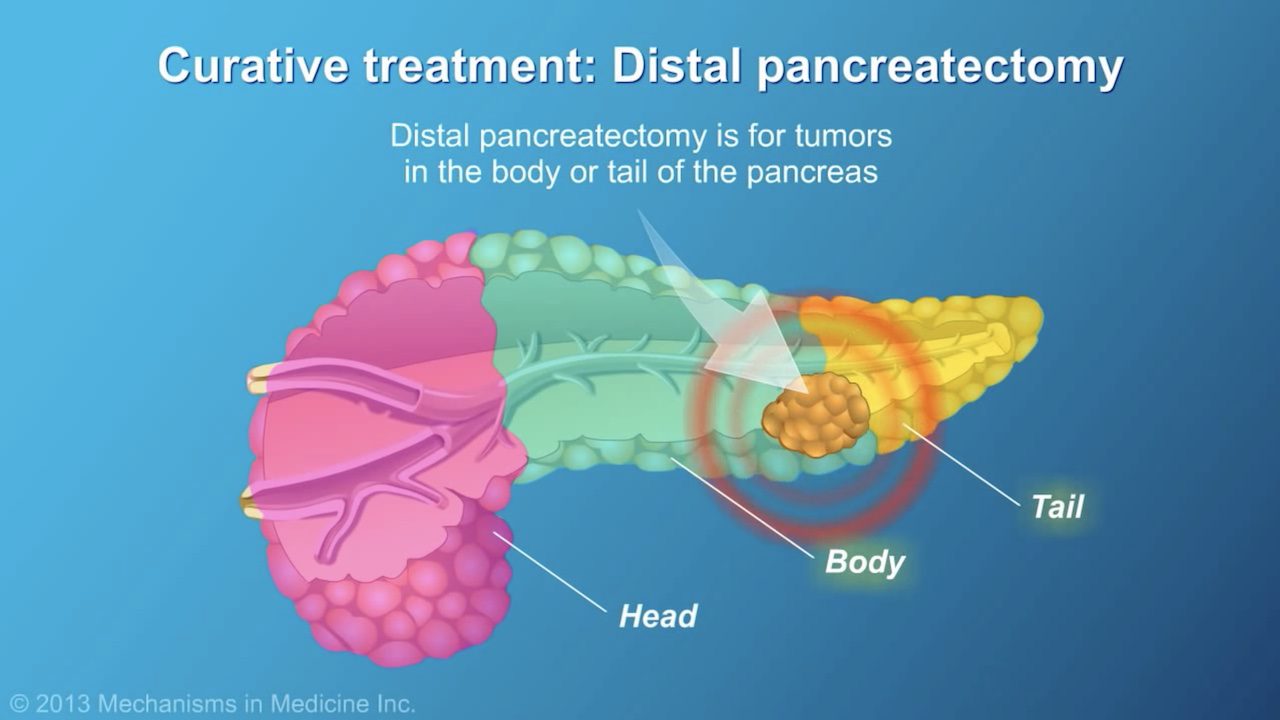
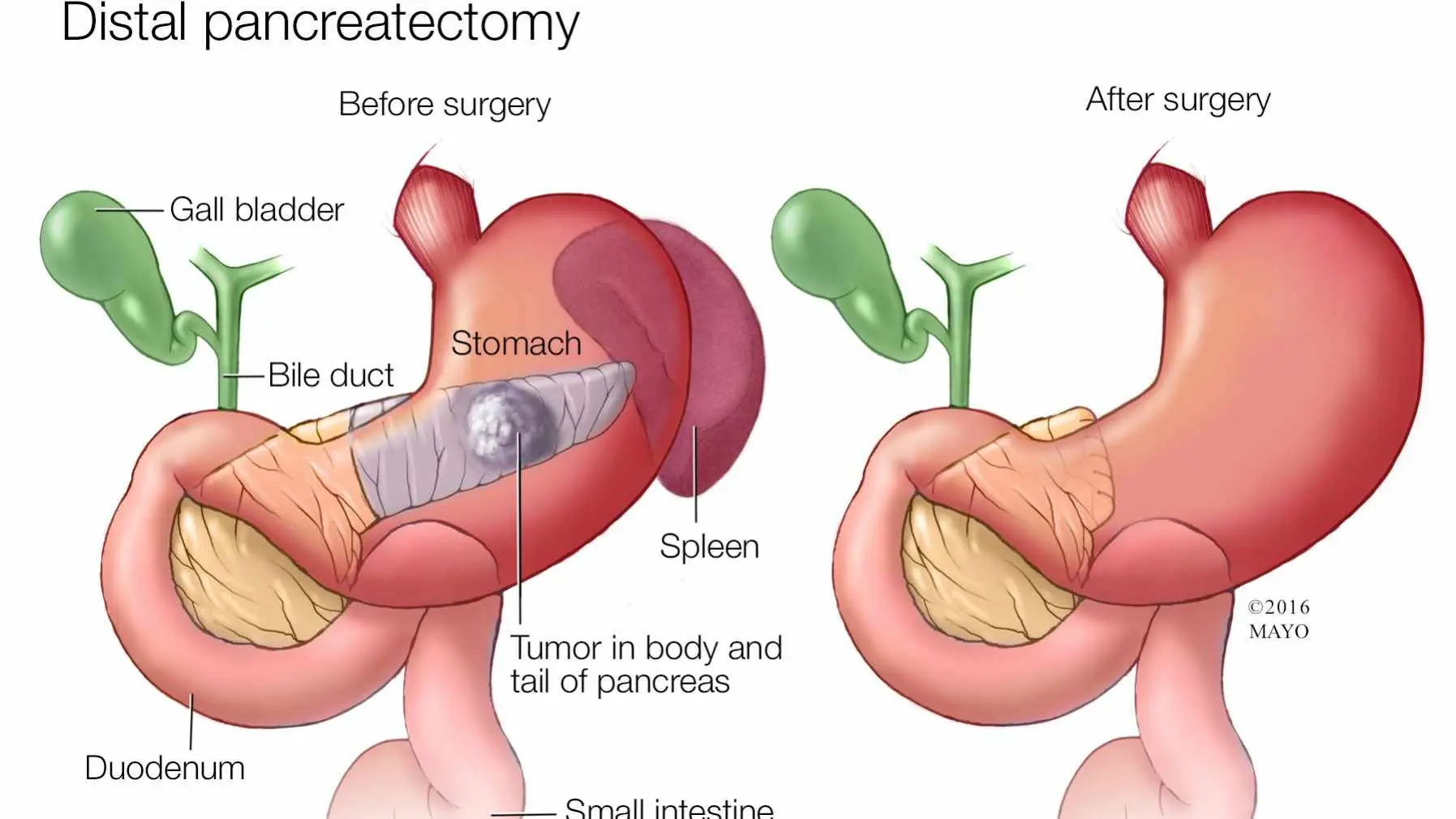
Surgery
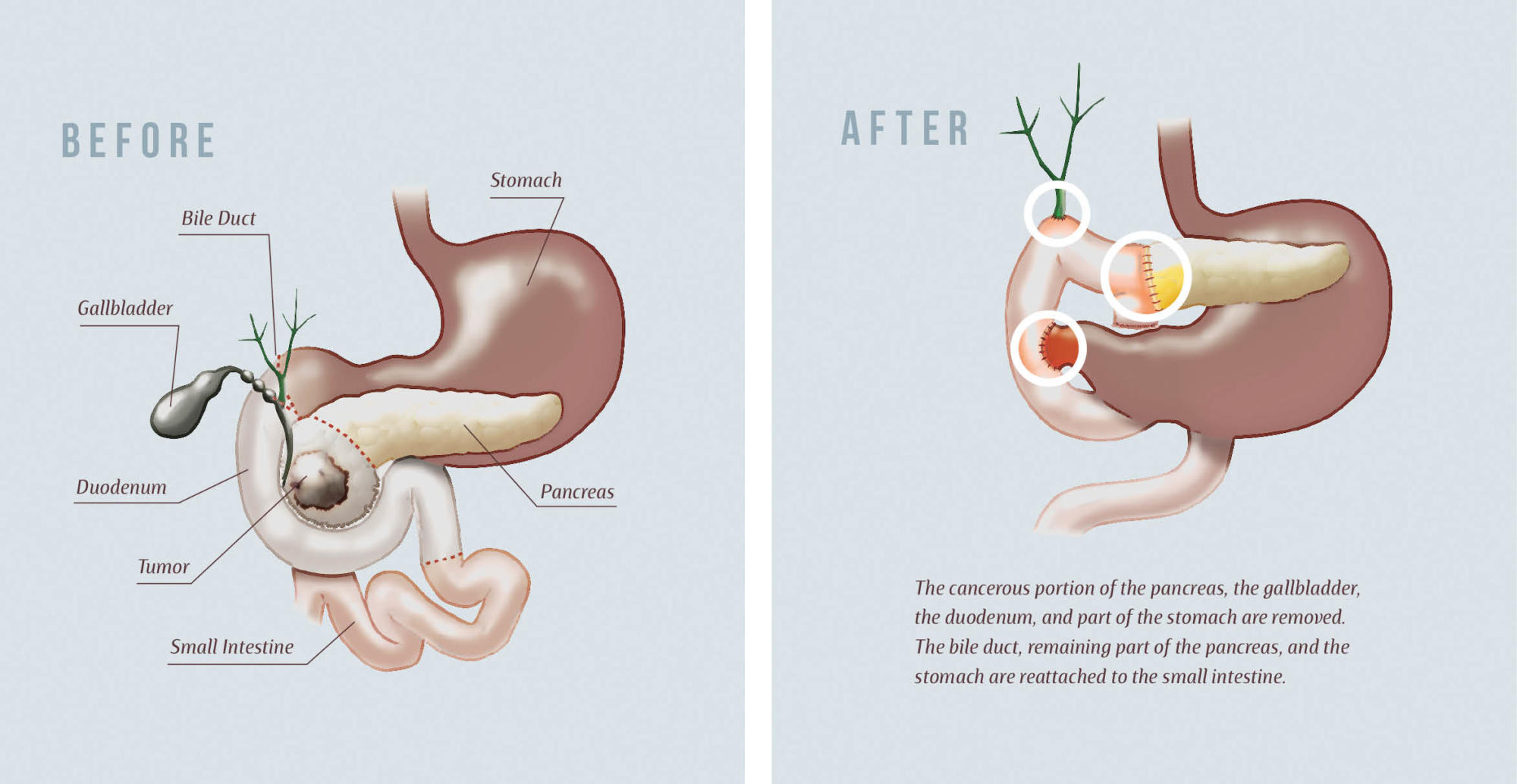
If the cancer is in the early stages, your doctor may recommend surgery to remove part or all of the pancreas, and sometimes parts of your other abdominal organs. The specific procedure your doctor recommends will depend on the location and size of your cancer, and whether it has spread.
Radiation therapy
Radiation uses high-energy beams to destroy cancer cells. It may be recommended before or after cancer surgery, often in combination with chemotherapy, or with other treatments if surgery is not an option.
Chemotherapy
Chemotherapy uses medicines to help kill cancer cells. It can be injected into a vein or taken orally (by mouth, as tablets or liquids, for example). It may sometimes be combined with radiation.
Targeted therapy
Targeted therapy uses medicines that attacks specific abnormalities within cancer cells.
Treating complications of pancreatic cancer
Your doctor may suggest treatments to help with some of the complications that can arise from the cancer. These complications and treatments include:
- jaundice — placing a stent inside the bile duct to hold it open, or a bypass to create a new way for bile to flow from the liver to the intestines
- pain — pain relief medicine, radiation therapy, or an injection to reduce pain signals to the brain
- bowel obstruction — placing a stent in the small intestine to hold it open, or bypass surgery to attach the stomach to a lower part of the intestines
- weight loss — eating more food when possible, and pancreatic enzyme supplements to help digestion, under advice from a dietitian
Palliative care
Palliative care aims to give you the best possible quality of life when you are seriously ill. If you have palliative care, your healthcare team will try to relieve your cancer symptoms without trying to cure it.
Palliative care may also involve medicines, radiotherapy or chemotherapy to help with pain or other symptoms.
You can speak to your doctor, nurse or cancer specialist and ask if palliative care is right for you, and what options are available.
Can pancreatic cancer be prevented?
Pancreatic cancer can’t be prevented, but you can reduce your risk by addressing any factors that increase your risk, for example, avoiding smoking.