
Key facts
- Osteoarthritis is a very common long-term condition that causes joint pain, stiffness and reduced movement.
- It can affect any joint in your body, but mostly occurs in the knees, hips, fingers, big toes, ankles and spine.
- Osteoarthritis can make it hard for you to do daily activities.
- Excess weight, a previous injury and repeated joint movements increase your risk of osteoarthritis.
- Regular exercise, healthy eating, pain management and sometimes surgery can help to treat symptoms.
What is osteoarthritis?
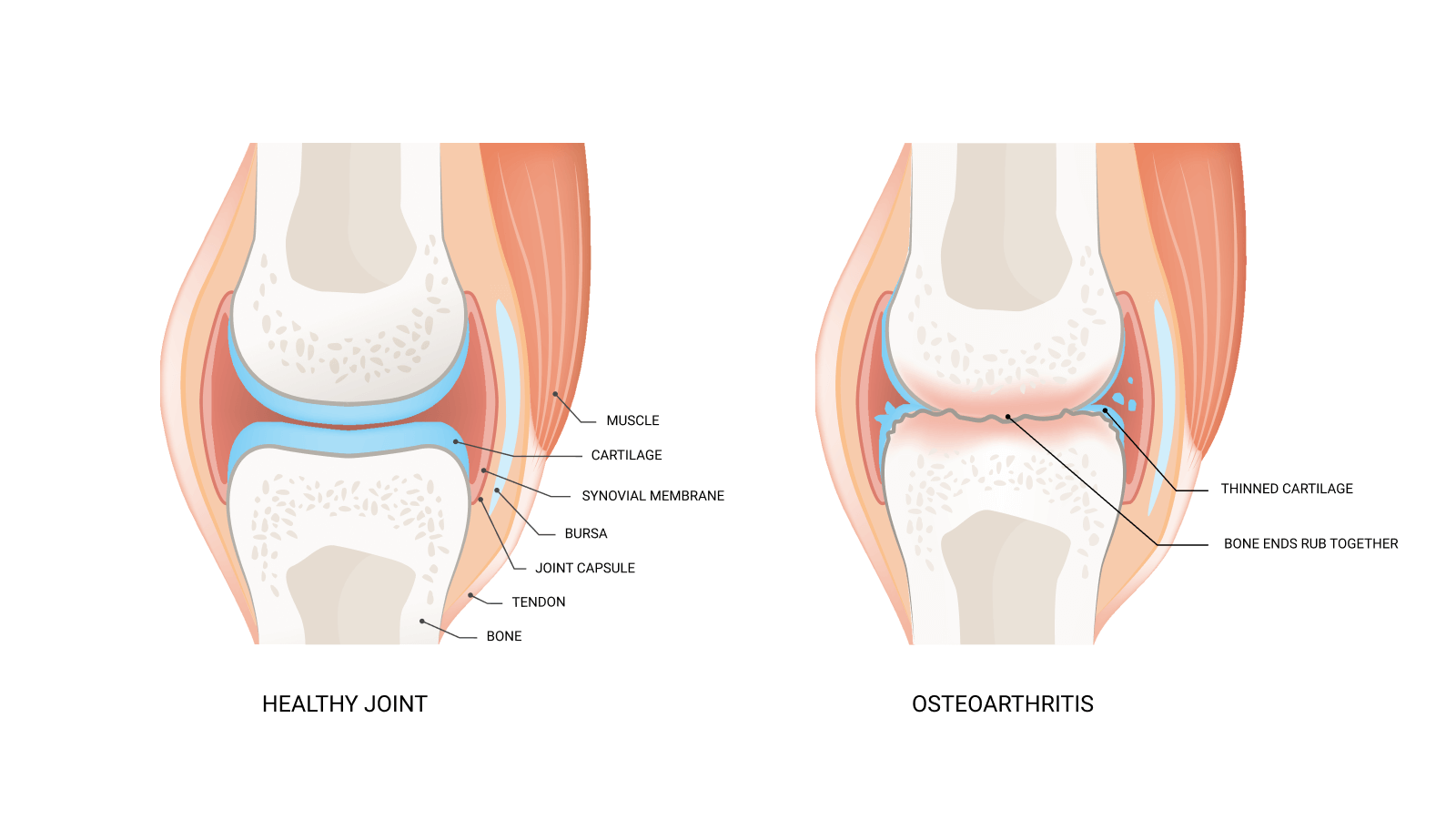
Osteoarthritis is a long-term condition where the joints in your body become inflamed and damaged. Over time, the cartilage layer that protects the ends of your bones wears away and new spikes of bone develop. Without cartilage, the bones in the joint rub together, causing pain, swelling, stiffness and reduced movement. This can make it harder for you to walk, climb stairs, or do other daily activities.
The condition can affect any joint in your body, but often it affects the knees, hips, fingers, big toes, ankles and spine. It can worsen over time.
Osteoarthritis is the most common type of arthritis in Australia. It is not the same as osteoporosis, a different condition where your bones become weak, fragile and more likely to break.
Osteoarthritis is a chronic condition where the joints in your body become inflamed and damaged, causing pain, swelling, stiffness and reduced movement.
What are the symptoms of osteoarthritis?
The main symptoms of osteoarthritis are:
- joint pain and stiffness
- problems with moving joints
- clicking noises or grating sensations when moving a joint
- less joint flexibility than before
- swelling and weakness of a joint
When you first develop osteoarthritis, you may only notice symptoms in your joints when you are moving them. As time goes on, you might notice symptoms with less activity or when you’re not moving. Some people have mild symptoms, while others may experience more severe, ongoing symptoms.
How common is osteoarthritis?
Osteoarthritis is very common. It becomes more common as you get older. It affects 1 in 5 Australians over age 45 and 1 in 3 over age 75. It is more common in females than males.
Osteoarthritis can develop at any age, but it is more common in people over age 40 and in those who have previously injured a joint.
Why might I have osteoarthritis?
Osteoarthritis does not have a specific, single cause. However, you may have a higher risk of developing osteoarthritis if you:
- are overweight
- have had a previous injury to a joint, such as a dislocation or a fracture
- have family members with osteoarthritis
- have a job that involves repetitive movements (such as kneeling, climbing, squatting, heavy lifting or hand movements)
How is osteoarthritis diagnosed?
Talk to your doctor if you have pain in your joints. Your doctor will ask you about your symptoms and examine you to work out if you might have osteoarthritis.
Tests are not usually necessary to diagnose osteoarthritis. Your doctor might arrange tests if it’s not clear what type of arthritis you have.
Your doctor may refer you for an x-ray to look for narrowing and changes in the shape of your joints. An x-ray won’t tell you how much osteoarthritis will affect you. Some people have a lot of joint pain, but their x-ray looks normal. Others have only mild symptoms, but their x-ray shows a lot of joint damage.
A blood test may help rule out other types of arthritis, such as rheumatoid arthritis.
How can I manage osteoarthritis?
There is no cure for osteoarthritis, but many people with osteoarthritis can manage their symptoms effectively. This can help them continue with daily activities and live healthy and enjoyable lives.
Be careful of any products or treatments that claim to cure osteoarthritis completely — your doctor will help you find the right treatment for you.
Regular exercise
Regular exercise is one of the most effective treatments for managing osteoarthritis. It keeps your joints and muscles healthy and flexible and can reduce pain. Exercise helps prevent other health problems as well.
In general, your exercise should include:
- muscle stretches or yoga — to help maintain or improve your flexibility
- muscle strengthening — exercises with weights and resistance bands improve your muscle strength, which takes pressure off your joints, strengthens your bones and improves your balance
- activities like brisk walking, swimming or cycling — to improve your general fitness and the health of your heart and lungs
It’s a good idea to choose low-impact activities that don’t put a lot of stress on your joints. Choose activities that you enjoy and are convenient for you to do. Remember that activities such as gardening, looking after pets and taking the stairs instead of the lift all count as exercise.
Talk to your physiotherapist about how to start an exercise program that is right for you.
Healthy eating and weight loss
There is no diet that will cure osteoarthritis. A balanced diet helps to keep you healthy.
Extra body weight increases stress on many joints — especially your knees, hips and lower back. If you are overweight, losing weight can help decrease pain and limit further damage to your joints.
Be aware of saturated fats that are found in red meat, poultry and full-fat dairy products. Too much of these will increase your level of unhealthy LDL-cholesterol, which has been linked with increased cartilage damage in people with osteoarthritis.
Special devices and footwear
Walking sticks can help to reduce the load on your hips and knees and reduce pain when moving about.
Some people with knee osteoarthritis try taping the joint, wearing a brace, or using shoe insoles that adjust how you stand and walk. It’s not clear whether these are helpful.
Ask your physiotherapist for advice about using aids or supports.
Pain management
It can be helpful to understand how your osteoarthritis pain works and your own response to it. Pain coaching, cognitive behaviour therapy or mindfulness may help to reduce the effect of pain on your life.
Massages, heat packs and transcutaneous electrical nerve stimulation (TENS) may help with pain.
Some people find that paracetamol helps improve their pain. Research shows that it’s not very effective for knee or hip osteoarthritis pain, but you can take it if it helps you.
A group of pain-relieving medicines called non-steroidal anti-inflammatory medicines (NSAIDs) can reduce osteoarthritis pain, stiffness and swelling. Check with your doctor if these are suitable for you. They have many potential side effects, such as stomach ulcers and bleeding, kidney problems and heart problems.
NSAIDs also come in creams or gels. These are safer than tablets, but they don’t usually help with hip symptoms.
An injection of cortisone into the painful joint can give you pain relief for a few weeks, depending on which joint is affected. However, there is a limit to how many injections you can have.
Ask your doctor or pharmacist about the best pain relief for you and how to use it.
Surgery
If your symptoms are affecting your daily activities and can’t be managed in other ways, your doctor may refer you to an orthopaedic surgeon. There are several different types of surgery for osteoarthritis.
Arthrodesis involves joining two bones together, which means you won’t be able to move the joint. It is most commonly used in ankle, wrist, finger or thumb joints to treat pain.
Arthroplasty (joint replacement) involves removing the damaged ends of your bones and replacing them with metal, ceramic, or plastic parts. It can be done on knees, hips, shoulders, elbows, fingers, ankles, toes and even the spine.
Osteotomy involves removing a small section of bone to improve the position of the bones in the joint. It is usually done on knees and occasionally hips.
Arthroscopy (sometimes called keyhole surgery) involves inserting a small camera into the joint to see directly into the area. Your surgeon may be able to remove or repair any damaged cartilage. It is not recommended for knee osteoarthritis unless your knee locks up.
Can I prevent osteoarthritis?
You can reduce your risk of developing osteoarthritis by:
- avoiding joint injuries or overuse — a sports injury prevention exercise program may help
- maintaining a healthy weight — by eating a healthy diet and exercising
Complications of osteoarthritis
Many people will not experience significant problems from their osteoarthritis. However, severe osteoarthritis may lead to:
- poor sleep due to pain
- reduced ability to exercise
- restrictions performing daily tasks
- a higher risk of falls in older people
- anxiety and depression
As osteoarthritis is a long-term condition. You may feel anxious, frustrated or upset about how it is affecting your life. Talk with your doctor or a friend you trust if you need help and support.



