Key facts
- An implantable cardioverter defibrillator (ICD) is a small device placed near the heart, which detects and corrects abnormal rhythms of the heart.
- You might need an ICD if you have a heart arrhythmia, such as an abnormally fast or irregular heartbeat.
- Fitting an ICD will require either a local or general anaesthetic, depending on your circumstances.
- People with ICDs should avoid certain types of electronic devices with strong magnetic fields, such as chainsaws and MRI.
- It’s important to tell any health professionals you see that you have an ICD.
What is an implantable cardioverter defibrillator (ICD)?
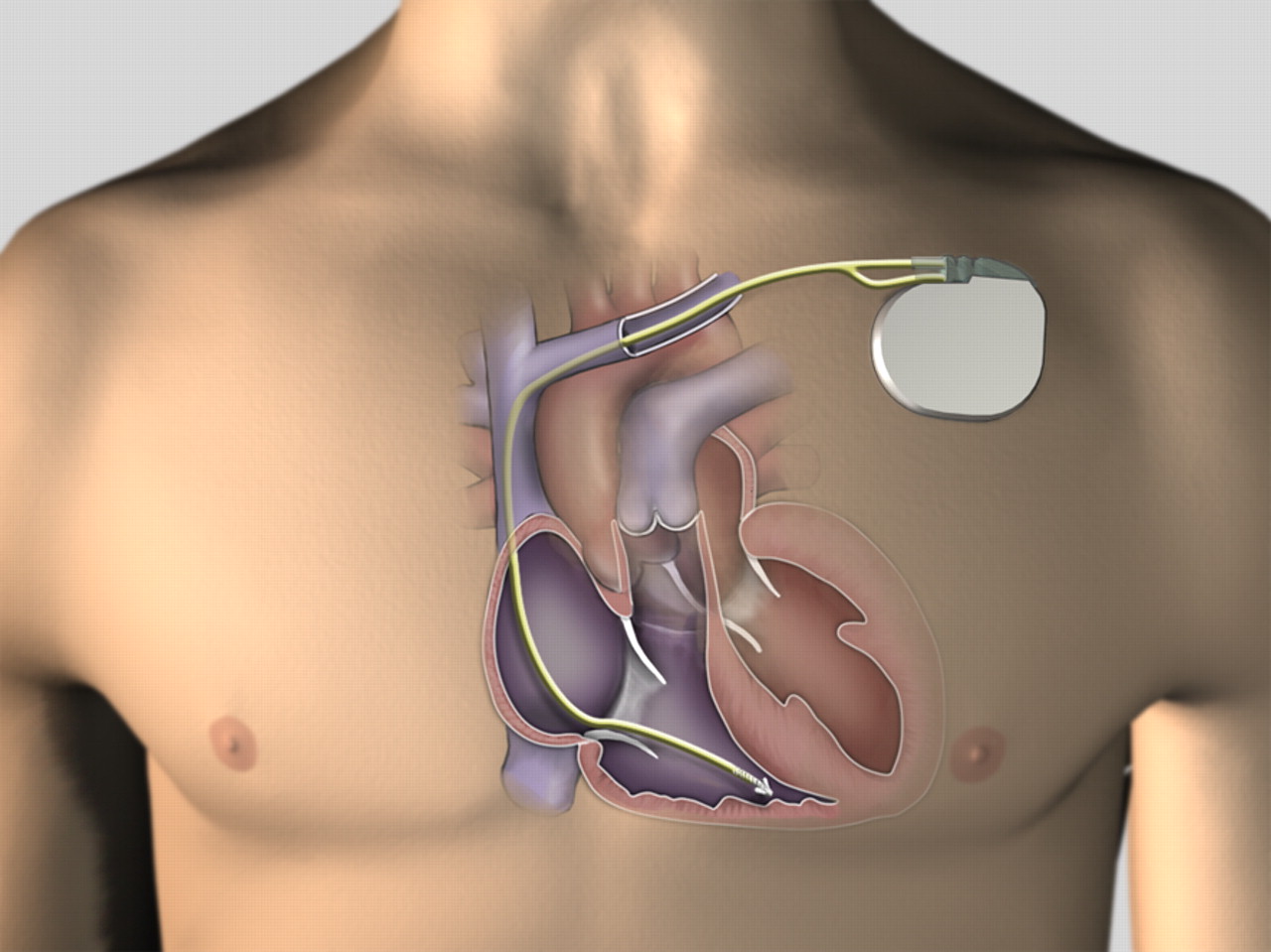
An implantable cardioverter defibrillator (ICD) is a small battery-operated medical device. It is placed in the body and connected to the heart to detect and correct abnormal rhythms of the heart. It is also called an ICD.
What does an ICD do?
An ICD, also sometimes called an AICD (automated implantable cardioverter defibrillator), sits under the skin near the heart. It monitors the heart’s rhythm 24 hours a day and detects abnormal rhythms in the ventricles (these are the parts of the heart that pump blood around the body).
If the heart beats too fast or too slow, or in an irregular way, blood won’t be pumped properly. Sometimes, an abnormal rhythm can make it too hard for the heart to pump blood at all.
An ICD uses electrical impulses to send messages for the heart to return to a normal rhythm — similar to how a pacemaker works. But if those impulses don’t work, the ICD will send a stronger electric shock to jolt the heart back into a normal rhythm.
Do I need an ICD?
You might need an ICD if you have a heart arrhythmia, such as an abnormally fast or irregular heartbeat. Your doctor would probably arrange for you to have tests first. The types of test that are performed will vary depending on your individual circumstances, but may include an electrocardiogram (ECG) or echocardiogram to see how your heart is beating.
If you are worried about your heart, see a doctor. Your doctor will discuss treatment options. Some people find that medication is effective.
How is an ICD fitted?
The ICD is inserted by surgery under the skin of your upper chest. This takes 1 to 3 hours to complete.
You might have a sedative to relax you before surgery. In most cases, this surgery requires a local anaesthetic, but some people will have a general anaesthetic. Your doctor will discuss your pain-relief options with you.
Your doctor will make an incision to create a ‘pocket’ in the upper chest, below your collarbone. This is 5 to 10 centimetres long.
One or 2 leads are guided through a vein, towards the heart, and are connected to a defibrillator. Your doctor will check the device is working properly.
The defibrillator is tucked inside the pocket and the incision is sutured; a dressing will be applied. There will be a visible bulge under the skin where the ICD was inserted.
What are the complications and risks of an ICD?
As with any type of surgery there are risks associated with ICD surgery.
The most common risks during the ICD procedure is bruising or bleeding from the wound and swelling.
Other less-common risks include:
- puncture of the lung causing an air leak
- vein or heart-valve damage, resulting from the placement of ICD leads
- movement of the ICD or its leads, which may need to be repositioned
- infection of the wound or wires
- failure of the ICD to work
What happens after an ICD-fitting procedure?
You will have a dressing over your wound and the site of the surgery may feel a bit sore. There may be some bruising. You should avoid wearing tight-fitting clothes while the wound is healing — since this might irritate your skin.
It may take a few weeks for you to start returning to normal activities after the procedure.
Your doctor will give you advice on how to look after your wound and what exercises or movements you can do in the weeks immediately after the procedure.
You might be advised not to lift anything heavy with the arm on the same side as the ICD. You might be advised not to push or pull things with that arm, and not to drive.
Always check with your doctor or clinic if you are unsure about what you should (or shouldn’t) do.
Call your doctor if:
- your wound is infected (it is red, swollen worm or leaking fluid)
- you have a fever up to 8 weeks after the procedure
- you continue to experience the heart symptoms you had before the procedure
- you lose consciousness, either due to arrhythmia or while receiving a shock
- you have any numbness or tingling in the arm closest to the ICD
- you hear a beeping noise coming from the ICD
How will life with an ICD be different?
Living with an ICD can be stressful and often people feel nervous for a little while after the procedure. Talk to your family and healthcare team about how you are feeling and any concerns you might have.
You will need to go to an ICD clinic for regular follow-up appointments and have ‘device checks’. Device checks monitor the electrical functioning of your heart, your device settings, and its battery life. Most ICD batteries will last between 5 and 15 years.
Create an action plan with your doctor so you know what to do if you get an electric shock from your ICD. Carry an ID card with your ICD details in your wallet or purse.
Tell all health professionals who treat you that you have an ICD.
When you have an ICD you need to avoid certain types of electronic devices with strong magnetic fields. These may cause your device to stop working. Most household items are OK, but you should keep the following items at least 15 centimetres away from your ICD:
- mobile phones — use yours on the opposite side of the body to the ICD and avoid putting it in a pocket near your device
- airport screening wands — let airport security know that you have an ICD
It is recommended that you avoid using the following items:
- industrial welders
- electric generators
- chainsaws
- magnetic resonance imaging (MRI)
- magnetic mattresses and pillows
Talk to your doctor if your work involves any of these items, if you are a commercial driver or if you operate heavy machinery.


