Key facts
- A glioma is a tumour that grows in the glial cells of the brain or spinal cord.
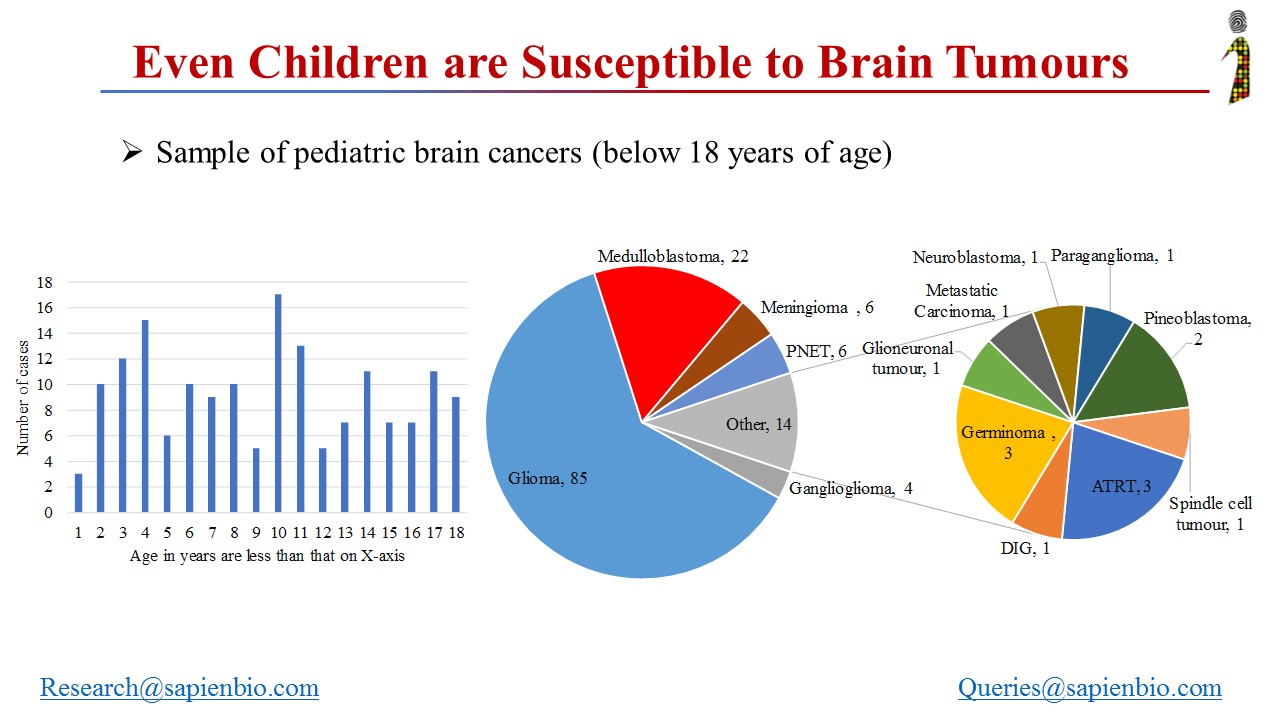
- There are different types of gliomas.
- There are several treatment options for gliomas in children.
What is a glioma?
A glioma is a tumour that grows in the glial cells of the brain and spinal cord. Glial cells surround nerve cells and help them work properly.
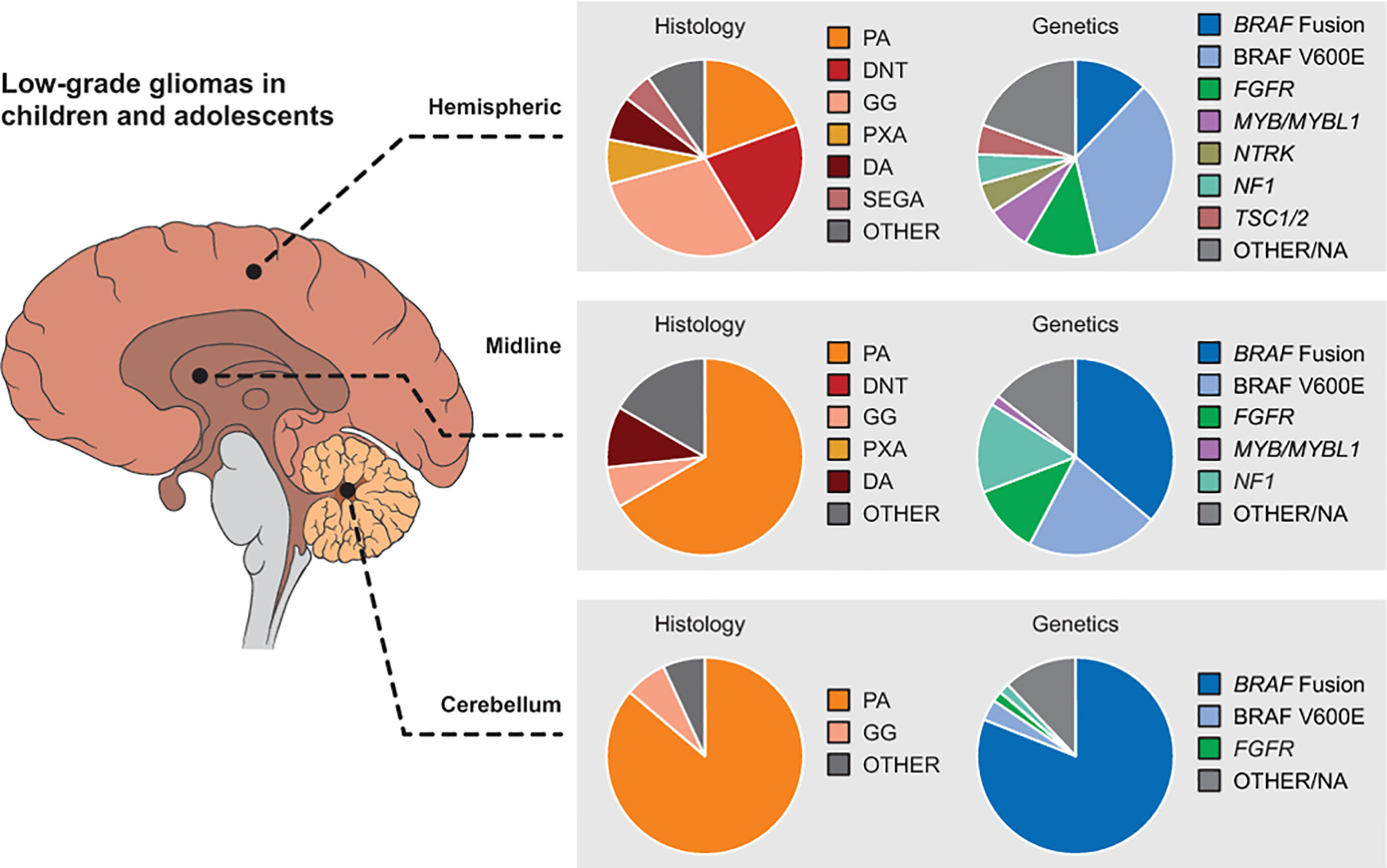
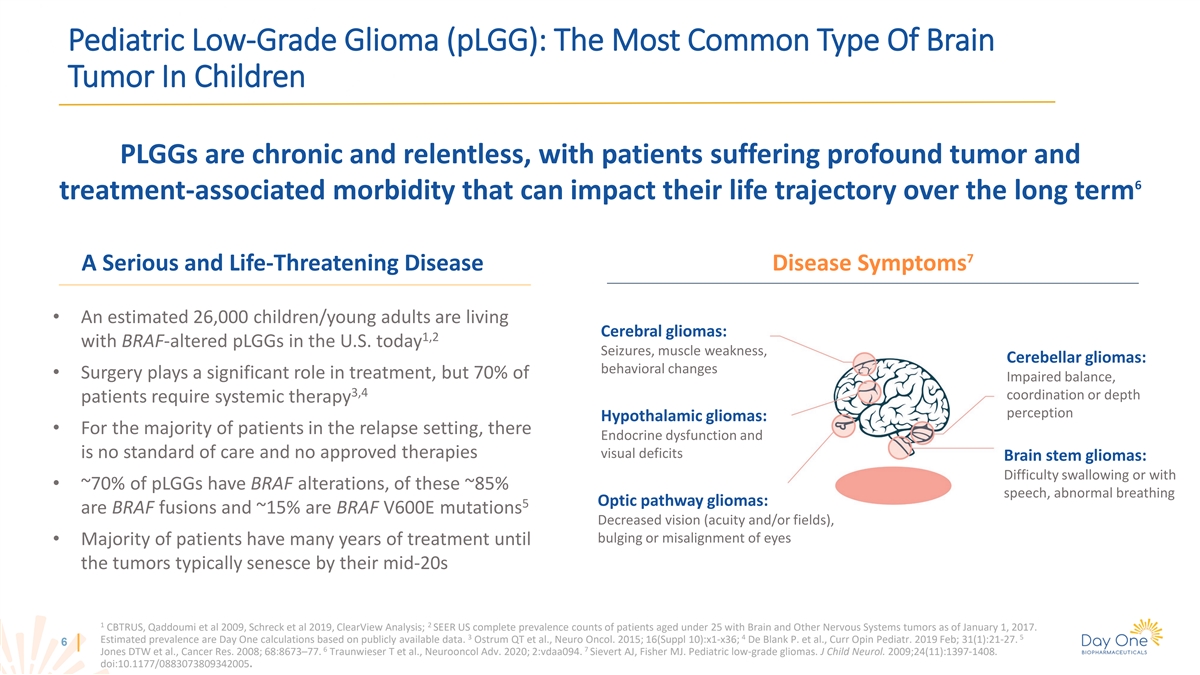
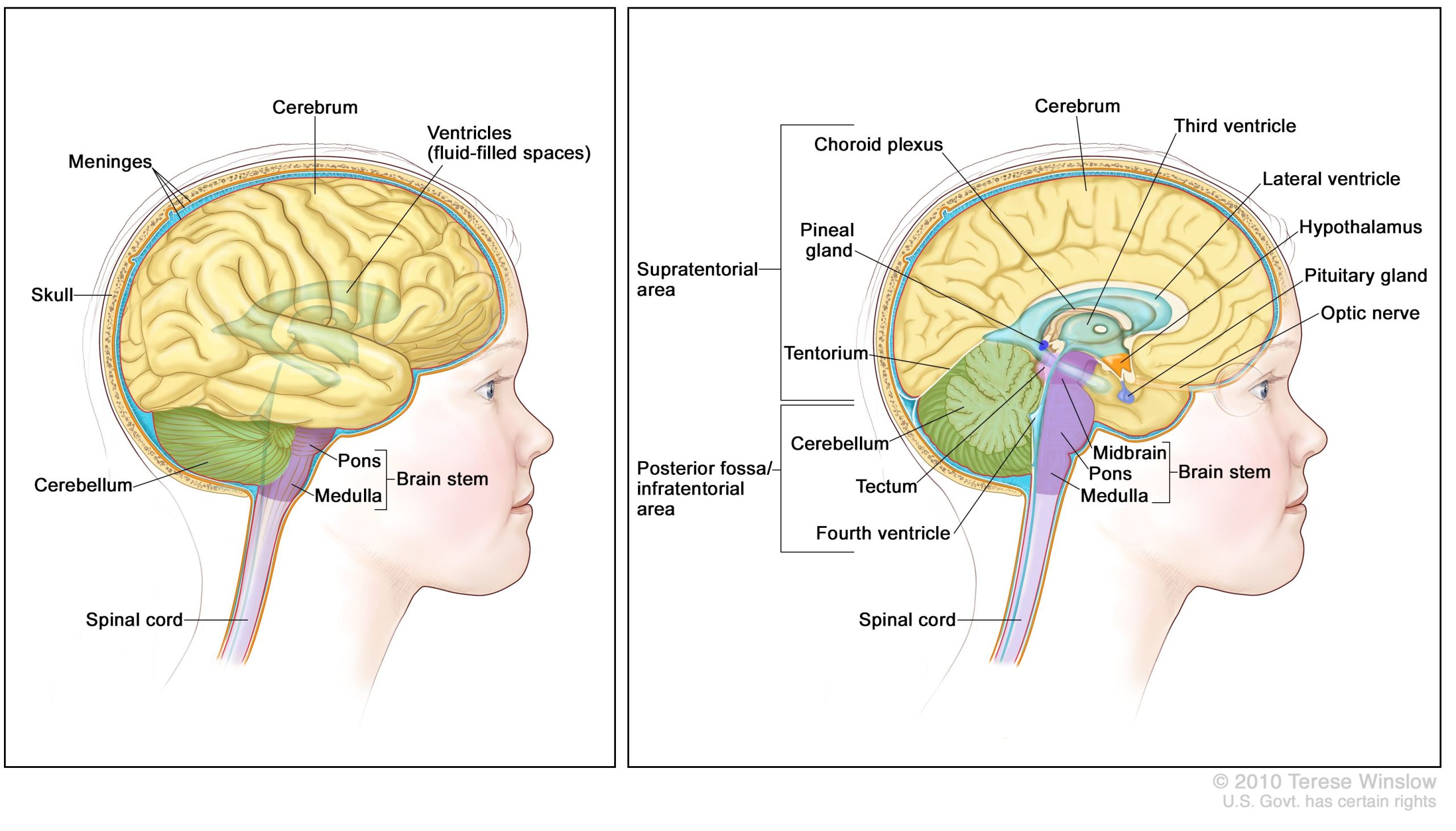
Gliomas can be benign (not cancerous) or malignant (cancerous). In children, they can grow in:
- the cerebrum (the front part of the brain)
- the cerebellum (the back part of the brain)
- the brain stem (the part of the brain connected to the spinal cord)
- the optic nerves (the nerves that control eyesight)
Types of gliomas
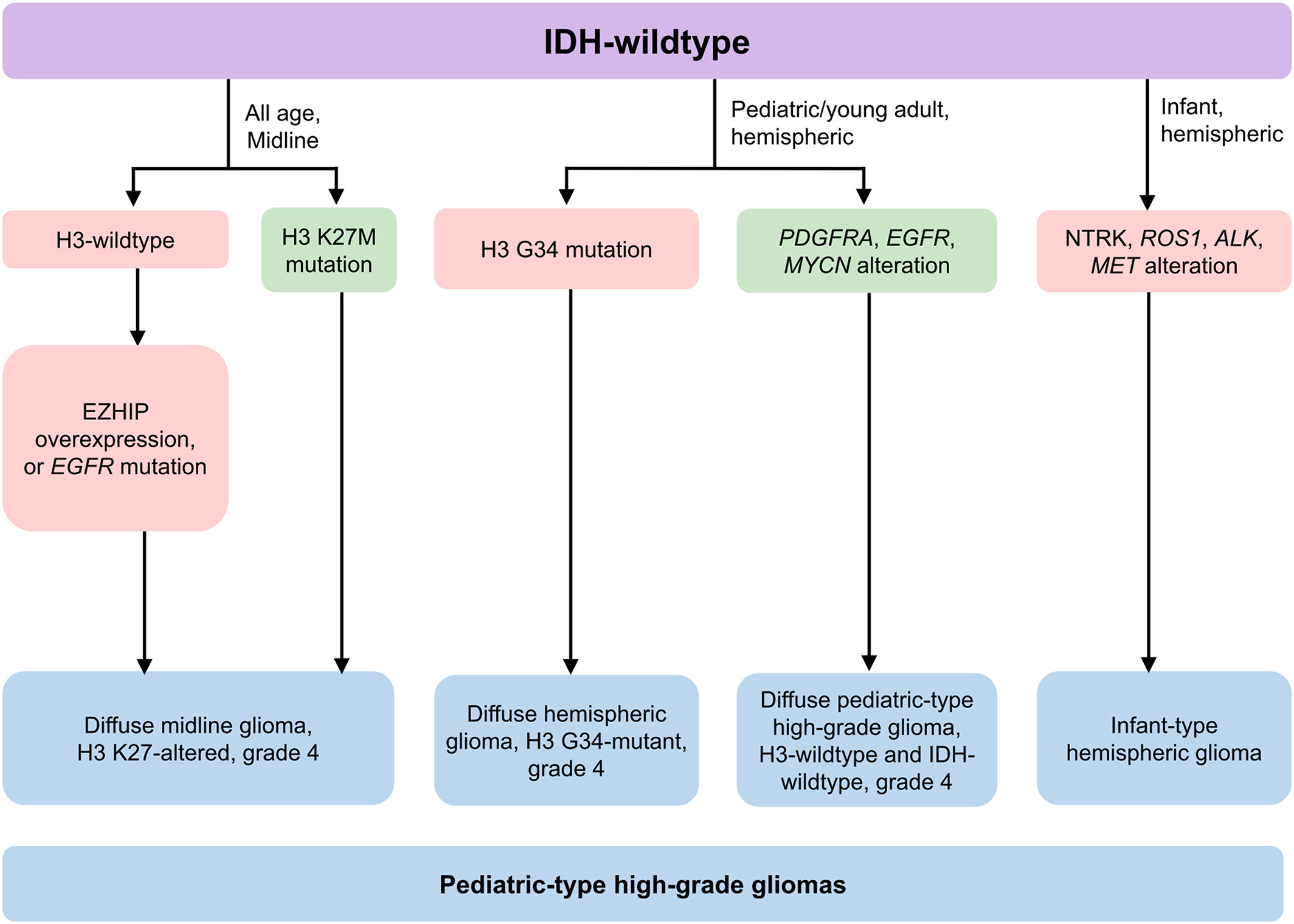
Gliomas can be slow-growing (called ‘low grade’) or aggressive (called ‘high grade’). If the tumour is Grade 1 or 2 it is low grade; if it is Grade 3 or 4 it is high grade.
There are different types of gliomas.
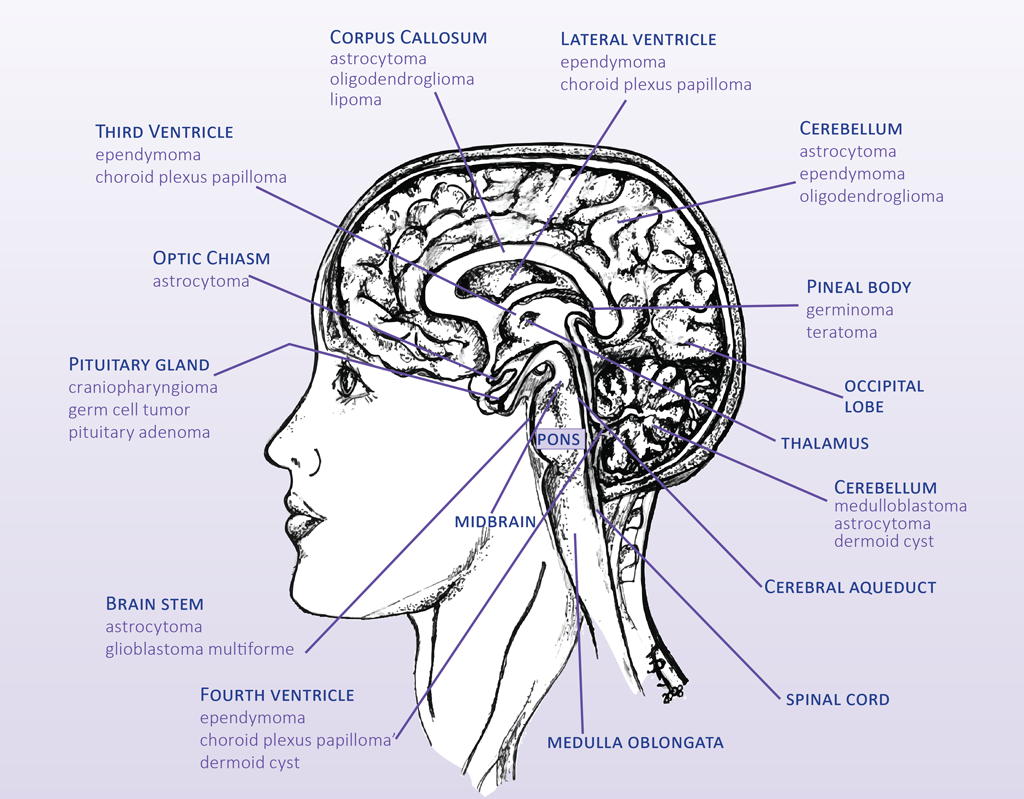
Astrocytomas
The terms ‘astrocytoma’ and ‘glioma’ are often used interchangeably. These can be high or low grade.
The different types of astrocytoma include:
- juvenile pilocytic astrocytoma (JPA), the most common low-grade tumour in children, which usually grows in the back part of the brain
- glioblastoma multiforme (GBM), a high-grade tumour that usually grows in the upper part of the brain
- anaplastic astrocytoma, a high-grade tumour that usually grows in the upper part of the brain
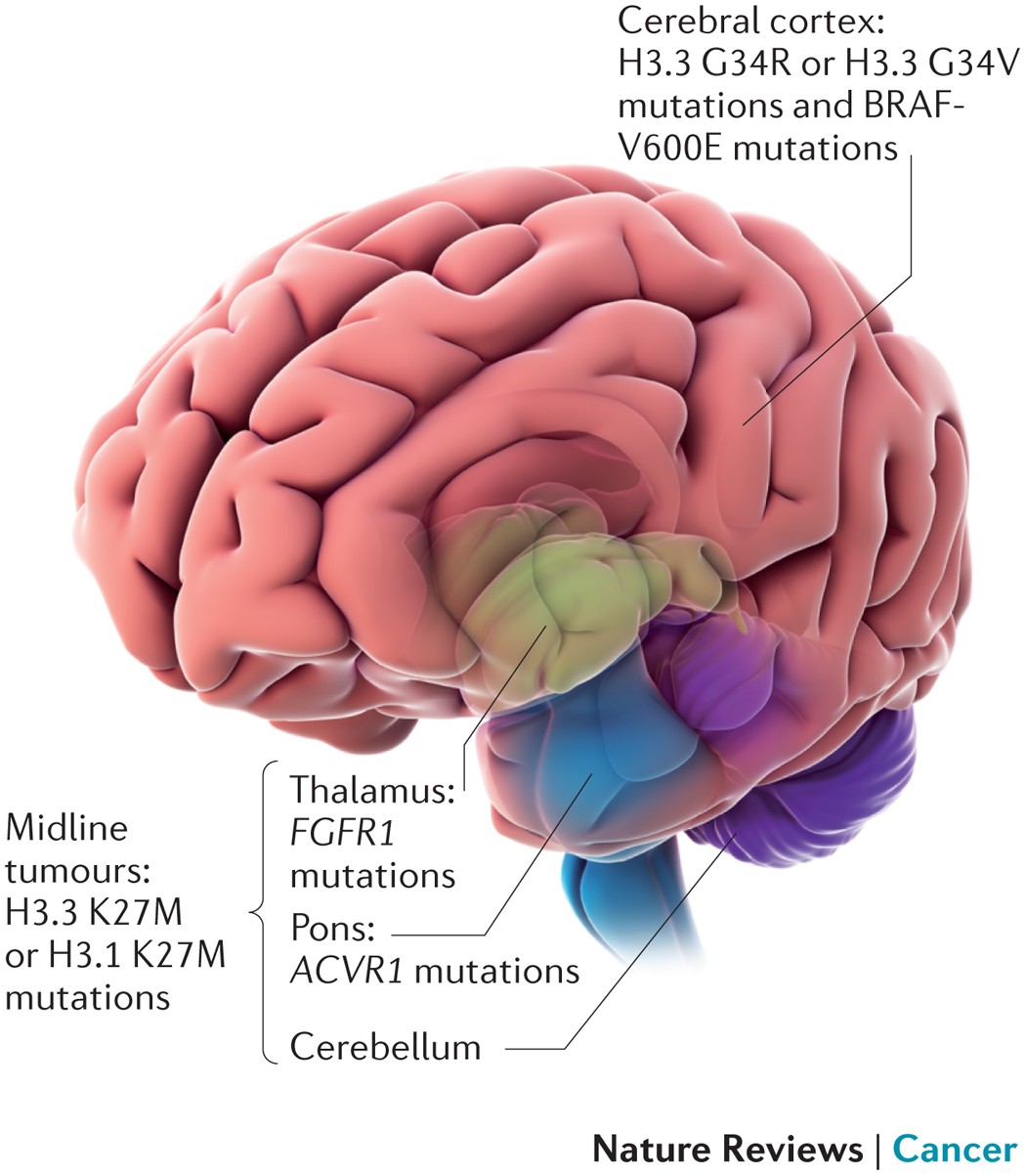
Diffuse midline gliomas (DMG)
Diffuse midline gliomas include tumours previously called diffuse intrinsic pontine gliomas (DIPGs).
These are tumours that grow in the brain stem, which controls heart rate and breathing.
Optic pathway gliomas
These are gliomas that grow in the optic nerve. The optic nerve connects the brain with the eyes.
What are the symptoms of glioma?
The symptoms of a glioma will depend on:
- where the tumour is
- how fast it is growing
- the age of your child
Symptoms can be caused by the pressure of the growing tumour on the brain and include:
- headaches, especially in the morning — the headache often goes away after vomiting
- nausea or vomiting
- problems with vision, hearing or speech
- problems with balance and coordination, trouble walking
- weakness or numbness in a part of the body, especially only on one side
- back pain
- changes in behaviour
Other symptoms can include:
- weight loss or weight gain for no reason
- seizures
- drowsiness or coma
In babies, symptoms may include:
- loss of appetite
- developmental delays
- losing physical or mental abilities they had before
- swelling of the head
- irritability
- failure to thrive — where a child does not gain enough weight
What causes glioma?
We don’t know why some children develop gliomas.
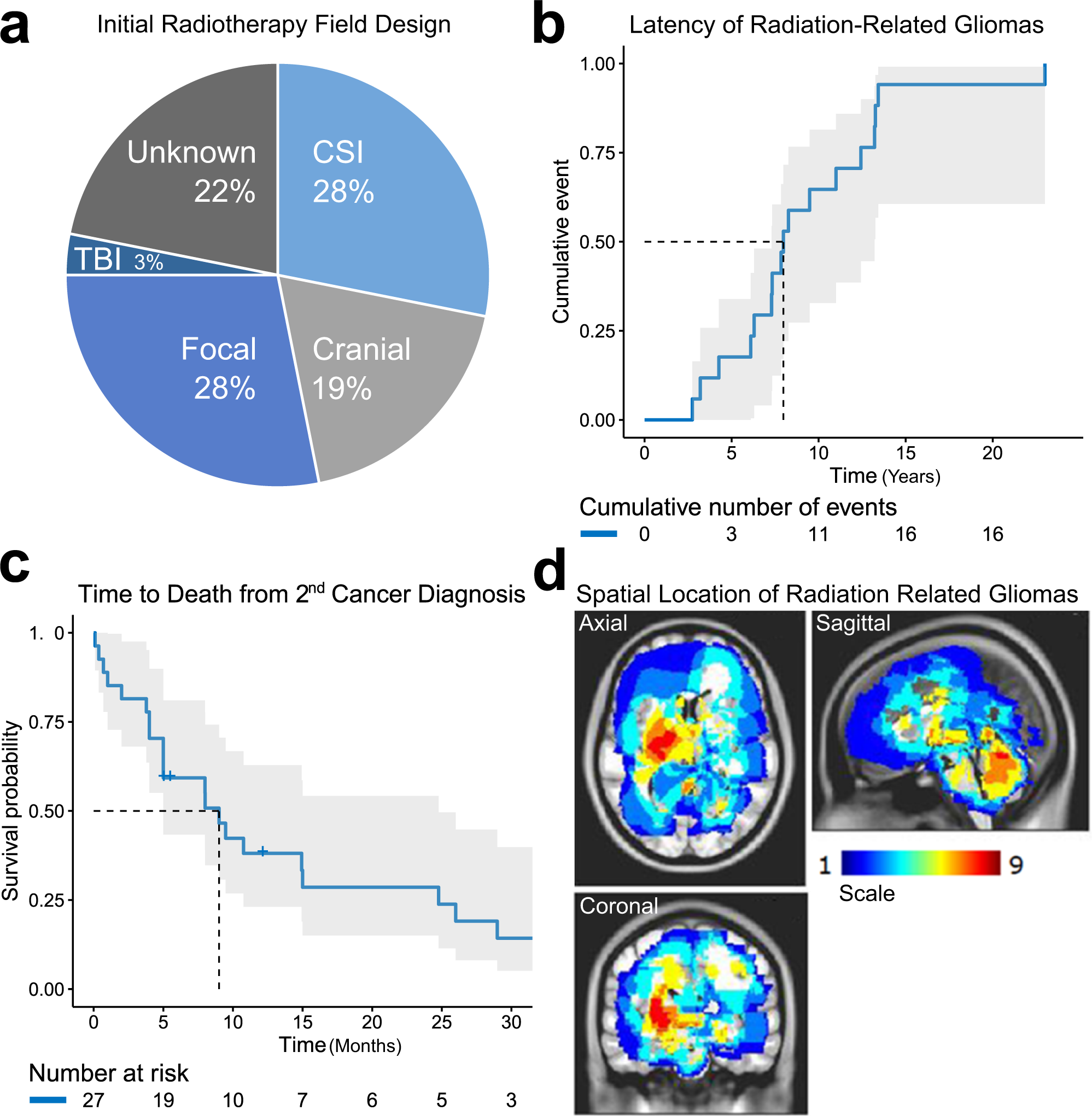
Gliomas are more common in children who:
- have a family history of brain cancer
- have been exposed to radiation
- have some genetic conditions
When should I see my doctor?
If you are worried about your child’s symptoms, see your doctor.
How is glioma diagnosed?
Your doctor will ask about your child’s symptoms and examine them.
If your doctor thinks that your child may have a glioma, your child will need medical tests. These may include:
- blood tests
- urine (wee) tests
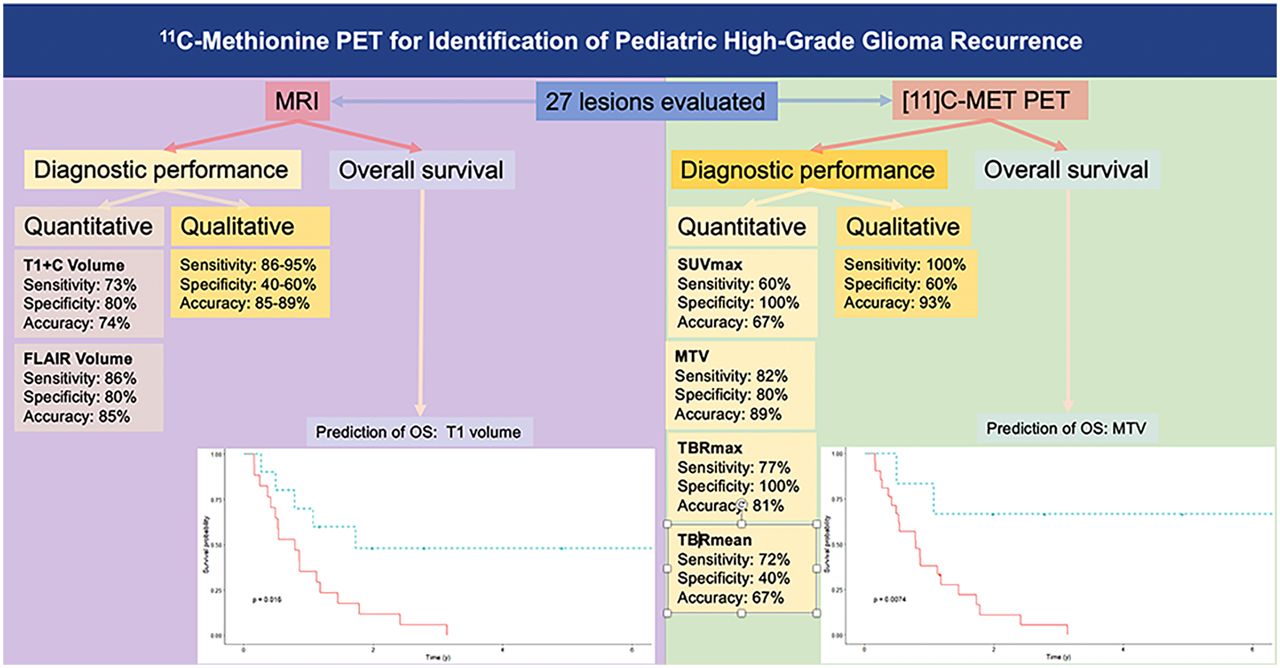
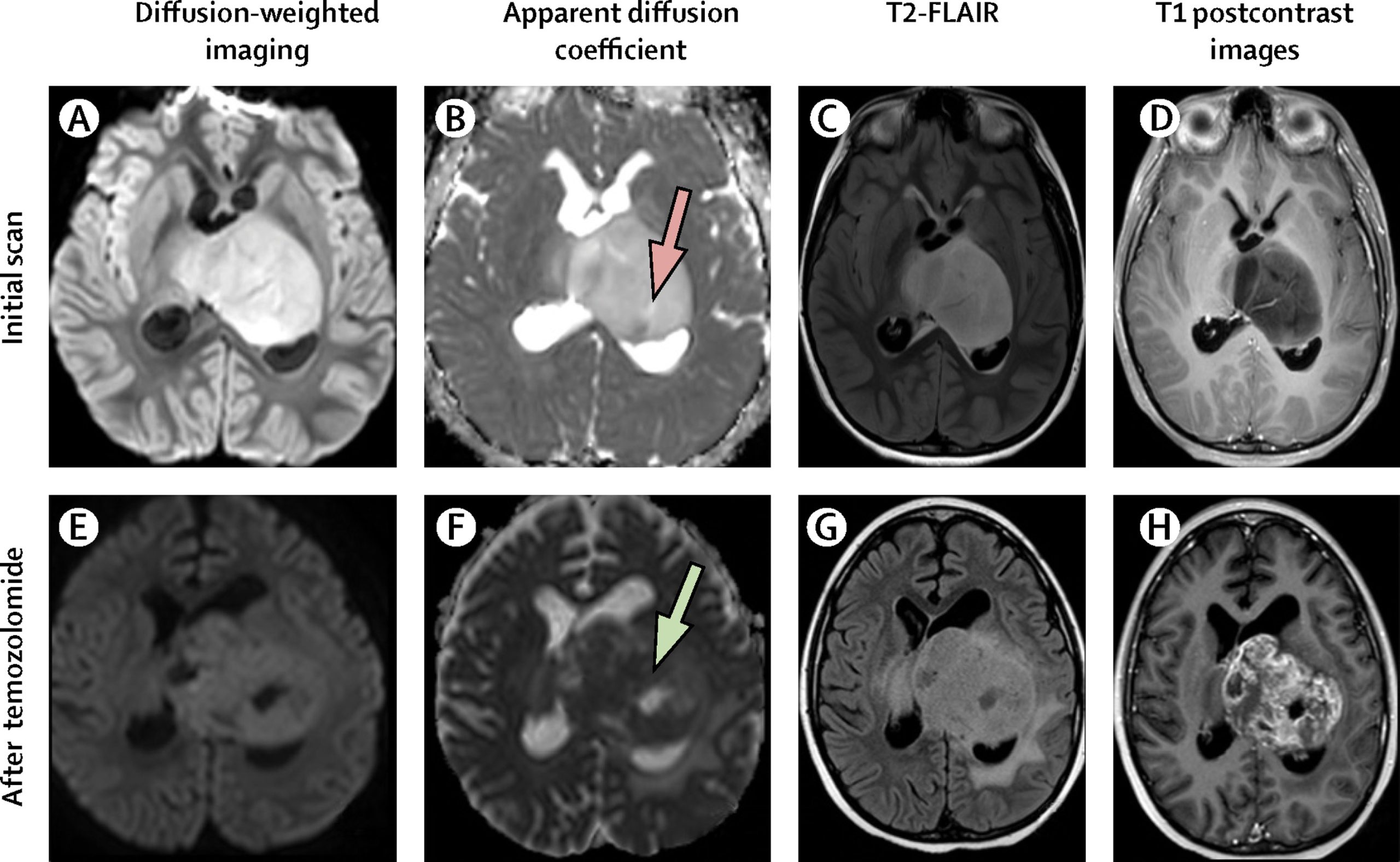
- CT scan, magnetic MRI scan, or PET scan
- a biopsy
- a lumbar punctureto sample the fluid that sits around the spinal cord
If your child has a glioma, they will be looked after by a team of health professionals, known as a multidisciplinary team.
Specialists your child might see include:
- paediatric oncologist (doctors who specialise in childhood cancer)
- paediatric surgeon (doctors who specialise in operating in children)
- neurologist (specialist in disease affecting the brain)
- radiation oncologists (doctors who specialise in using radiotherapy to treat cancer)
- endocrinologist (doctors who specialise in hormones and body development)
- nurses who specialise in caring for children with cancer
Other healthcare professionals your child might see include:
- your child’s regular doctor
- social workers
- rehabilitation therapists
- psychologists
- cancer care coordinators
- physiotherapists
- speech therapists
How is glioma treated?
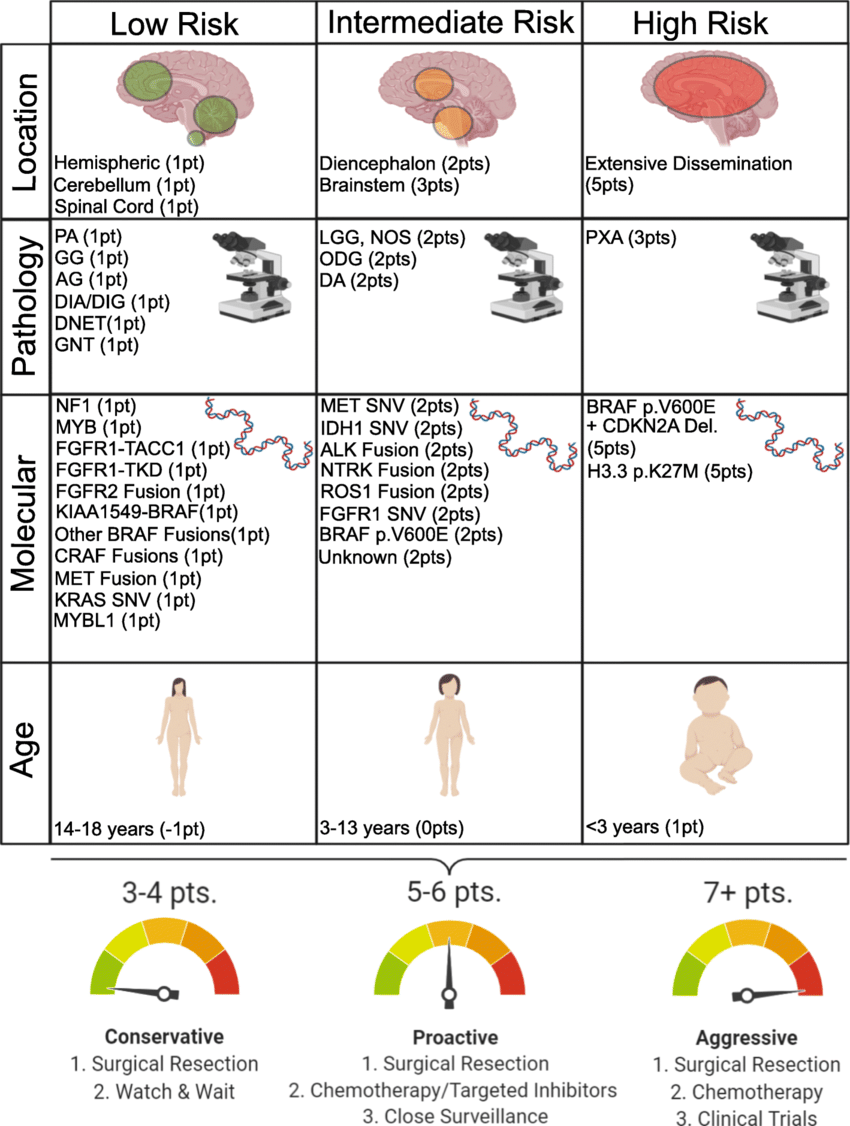
Your child’s treatment will depend on:
- their age
- the type of glioma
- where the glioma is in the brain or spinal cord
- how quickly the glioma is growing
- how your child reacts to the treatment
Your doctor will suggest treatment options based on your child’s situation. Most children have a mix of treatments. Treatment can last for several years.
Treatment options include the following.
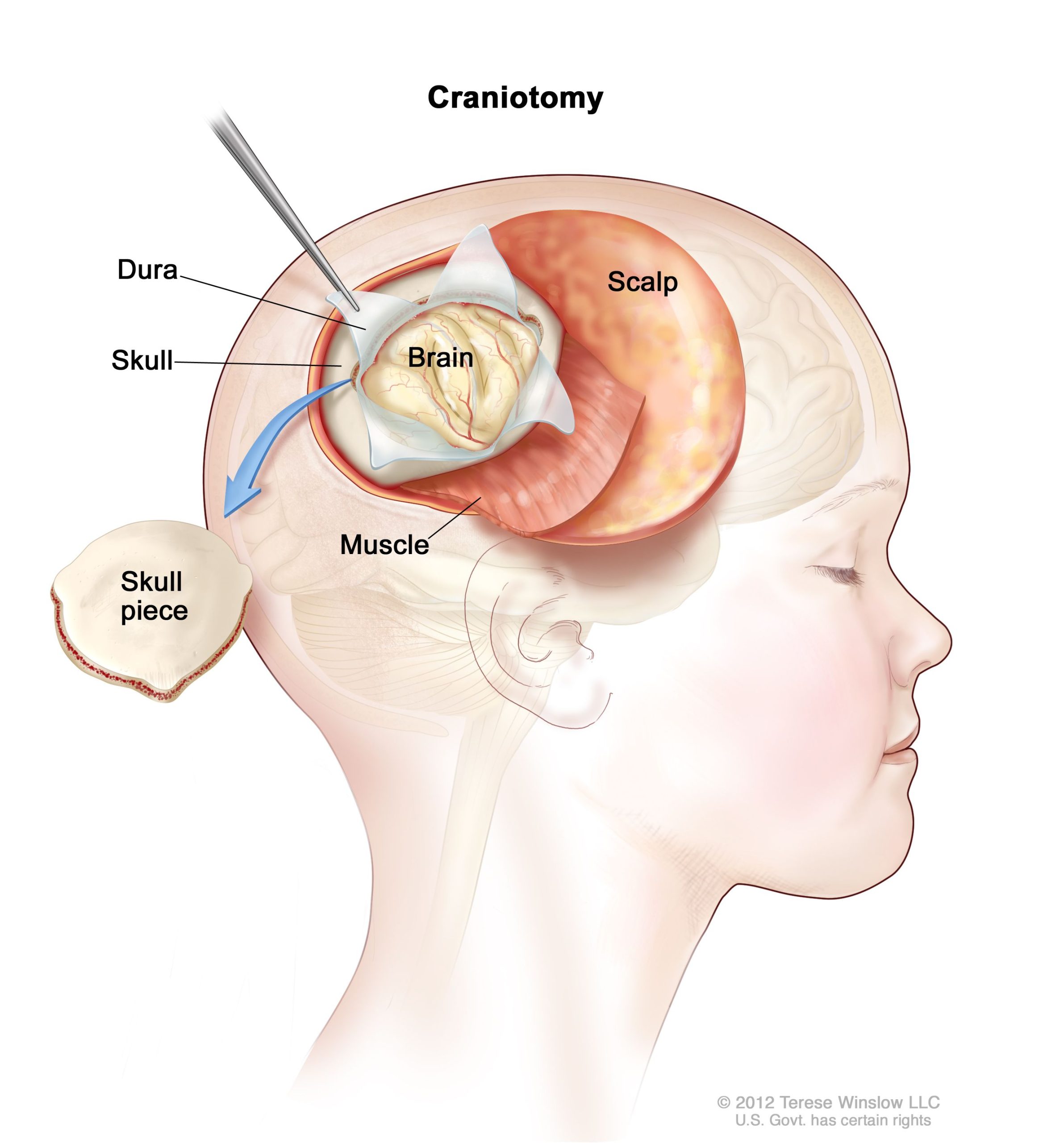
Surgery
Surgical treatment will attempt to remove as much of the glioma as possible. Surgery might not always be possible, for example if the tumour is in a very delicate part of the brain like the brain stem, or if the tumour has spread to other brain tissue.
Surgery might be the only treatment needed, especially if it is a slow growing (low-grade) tumour.
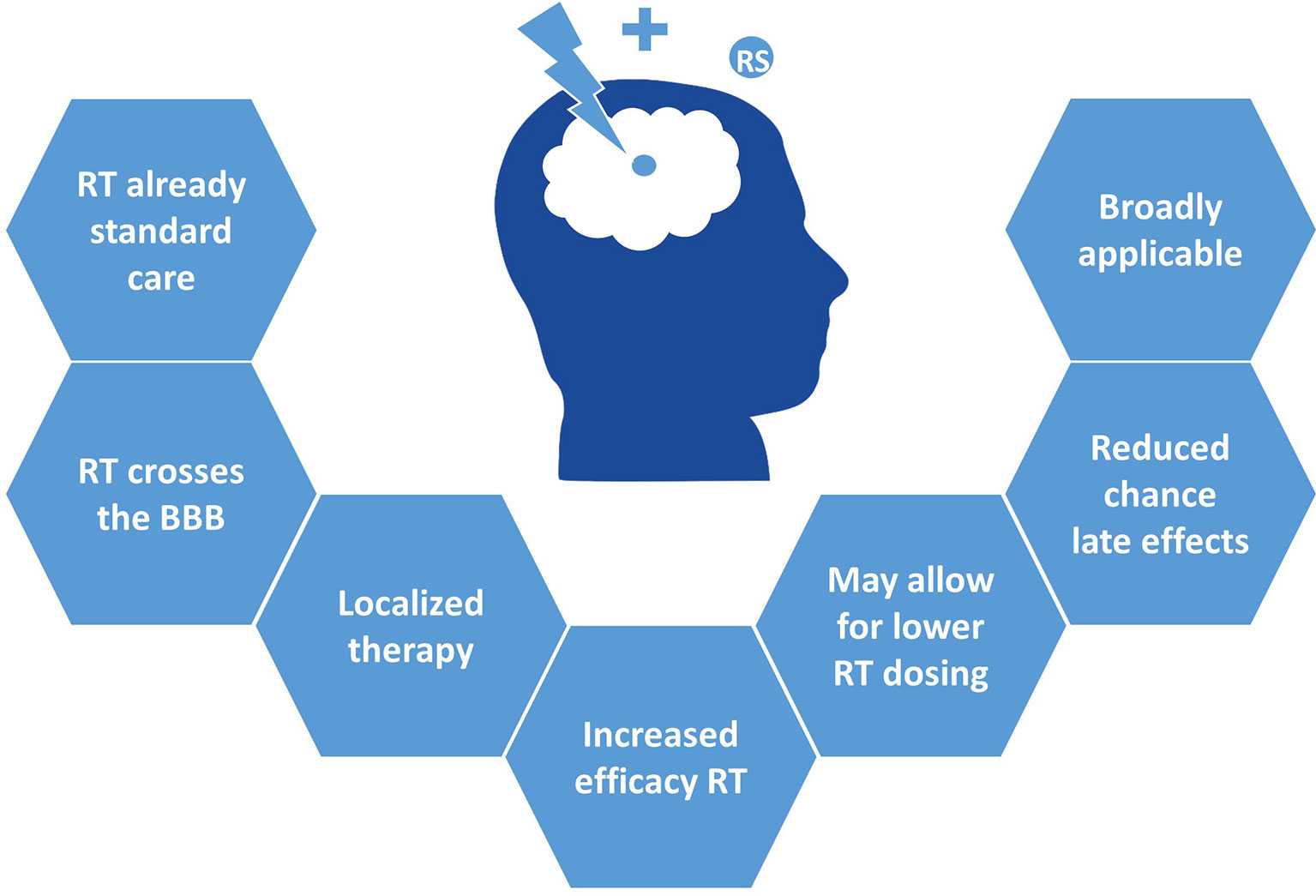
Radiotherapy and chemotherapy
Radiotherapy (radiation treatment) and chemotherapy (cancer medicine) can shrink the tumour. Radiotherapy is not usually suitable for children aged under 3 years.
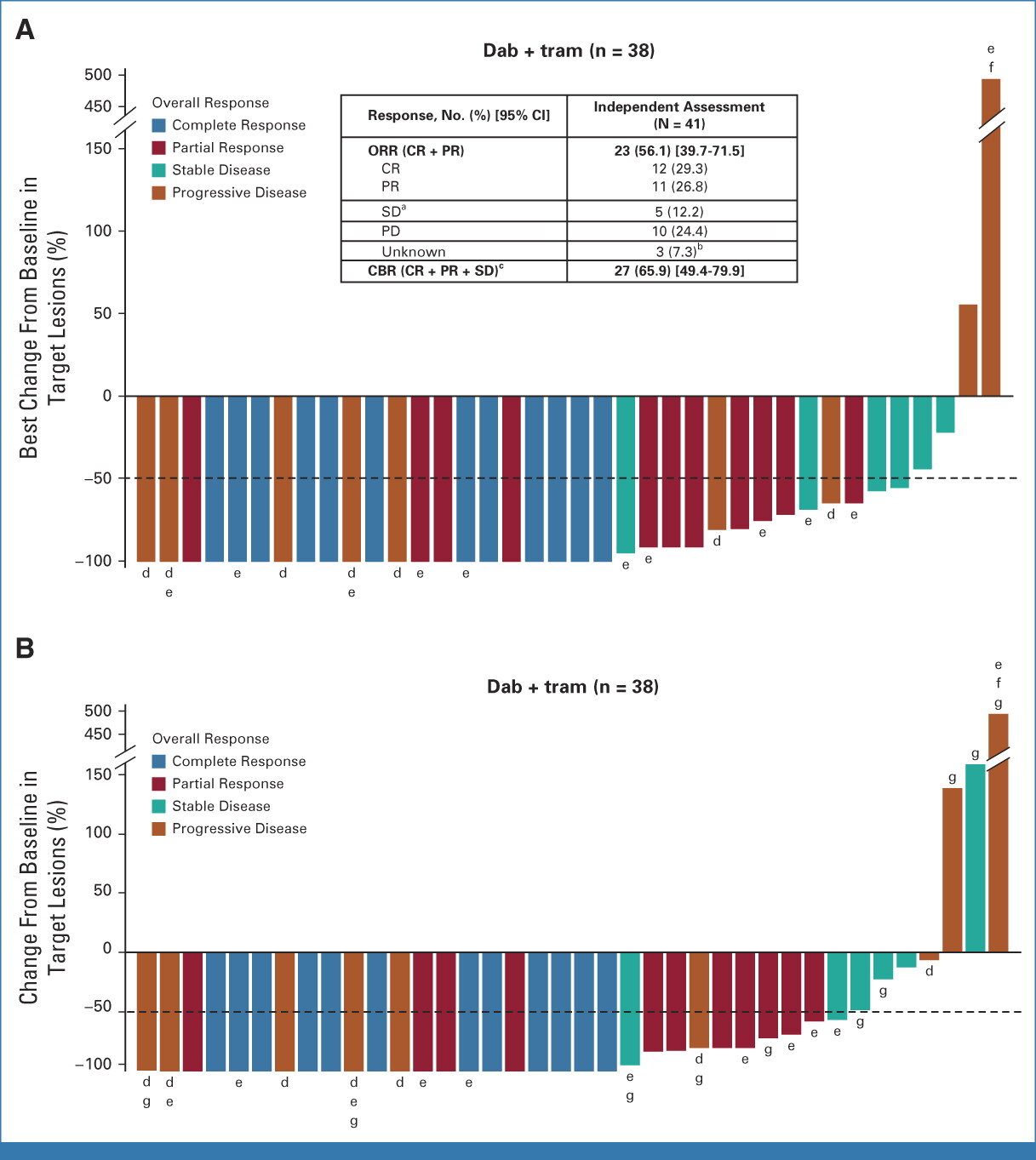
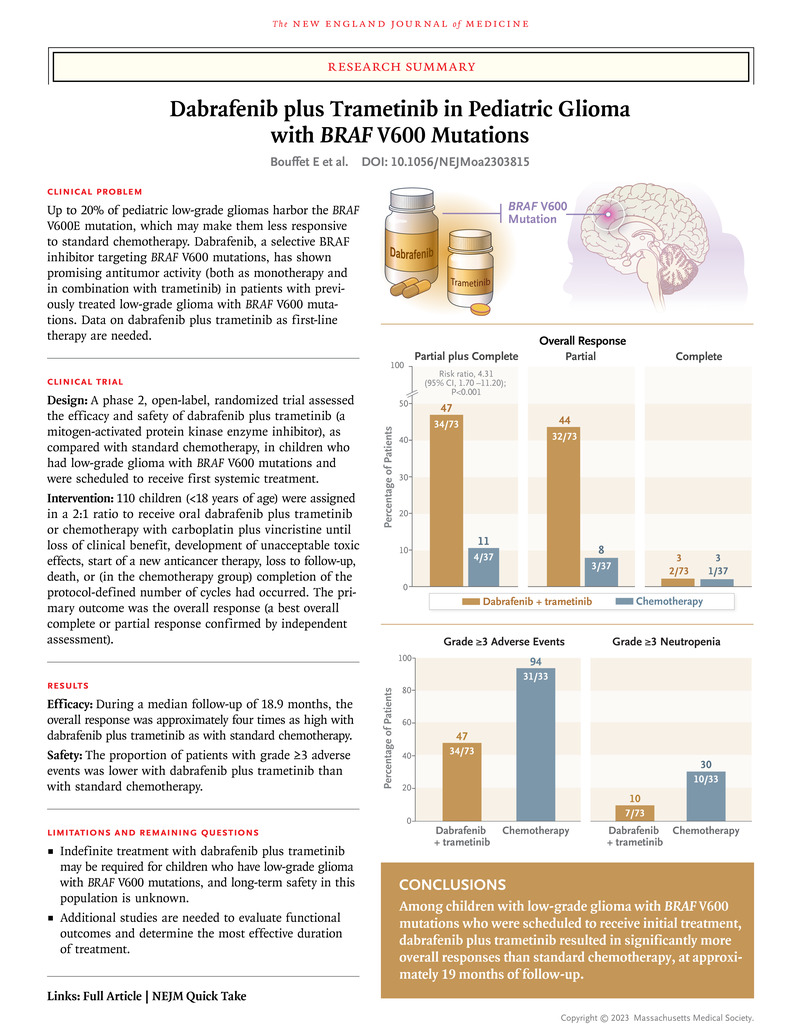
New treatments
There have been many advances in treating brain cancer recently.
Some places in Australia now offer advanced radiotherapy techniques such as:
- radiosurgery
- gamma knife
- proton beam therapy
- precise surgery techniques, such as cyberknife therapy
There are also targeted therapies that attack cancer cells without harming healthy cells.
Your child might also be able to take part in a clinical trial, giving them access to new medicines.
Other treatments
Your child might receive other medicines, such as:
- steroids, to reduce swelling and improve symptoms
- hormones, if the treatment has affected their hormone balance
- medicines to stop seizures or give pain relief
After treatment finishes, your child will need regular check-ups and scans. Gliomas can come back again. If this happens, the medical team might suggest different treatments.
Can glioma be prevented?
We don’t completely understand what causes some brain tumours in children. However, if a child develops cancer, it’s not because of something they, or their parents did to cause it. No one is to blame if a child develops cancer.
Complications of a glioma
Due to advances in treatment of children’s cancer, many children survive into adulthood. Talk to your doctor about your child’s diagnosis and prognosis (long-term survival).
Your child’s prognosis will depend on:
- their age at diagnosis
- the type of glioma they have
- where the tumour is and whether it is slow or fast growing
- how the glioma responds to treatment