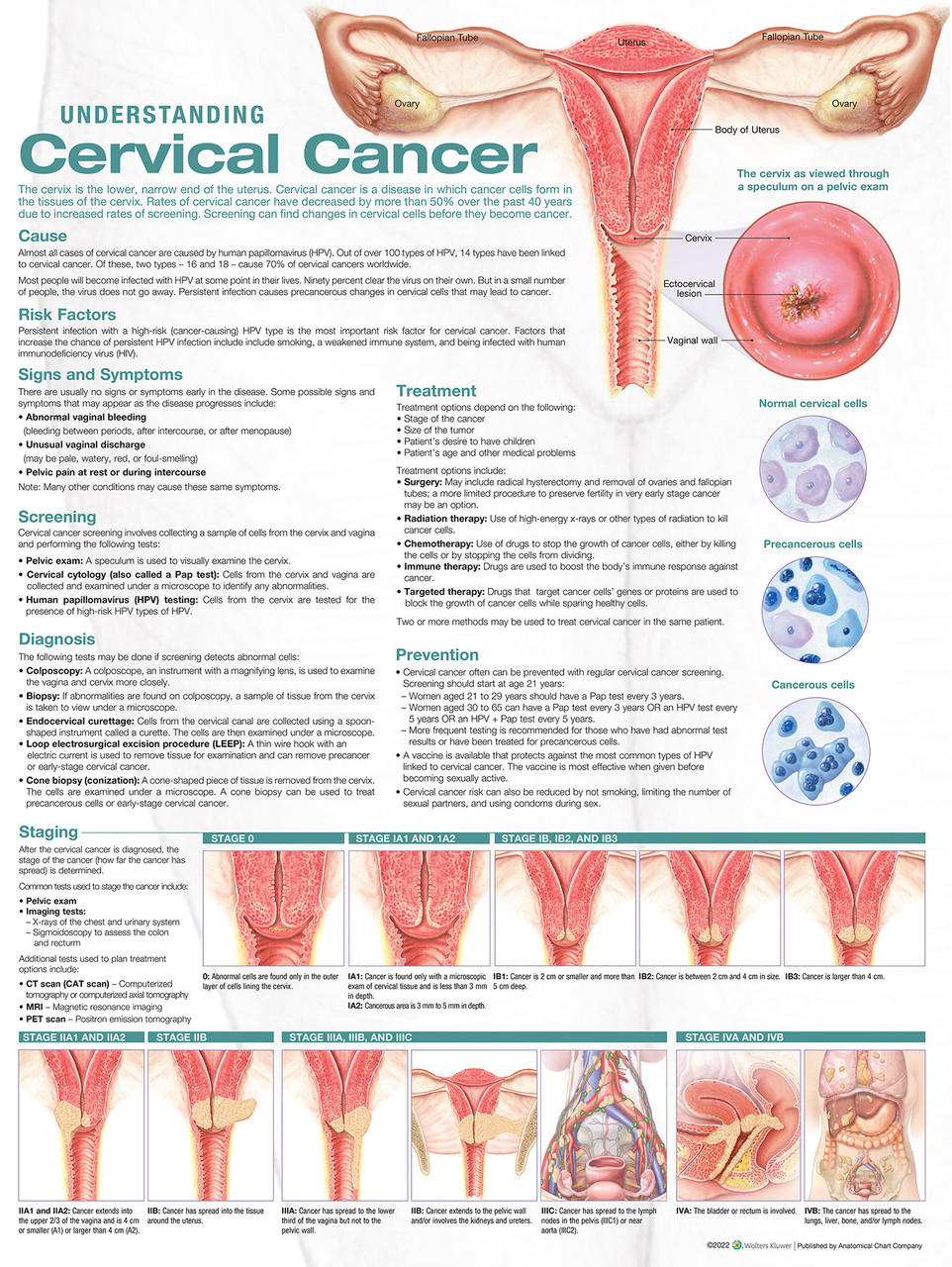
What is cervical cancer?
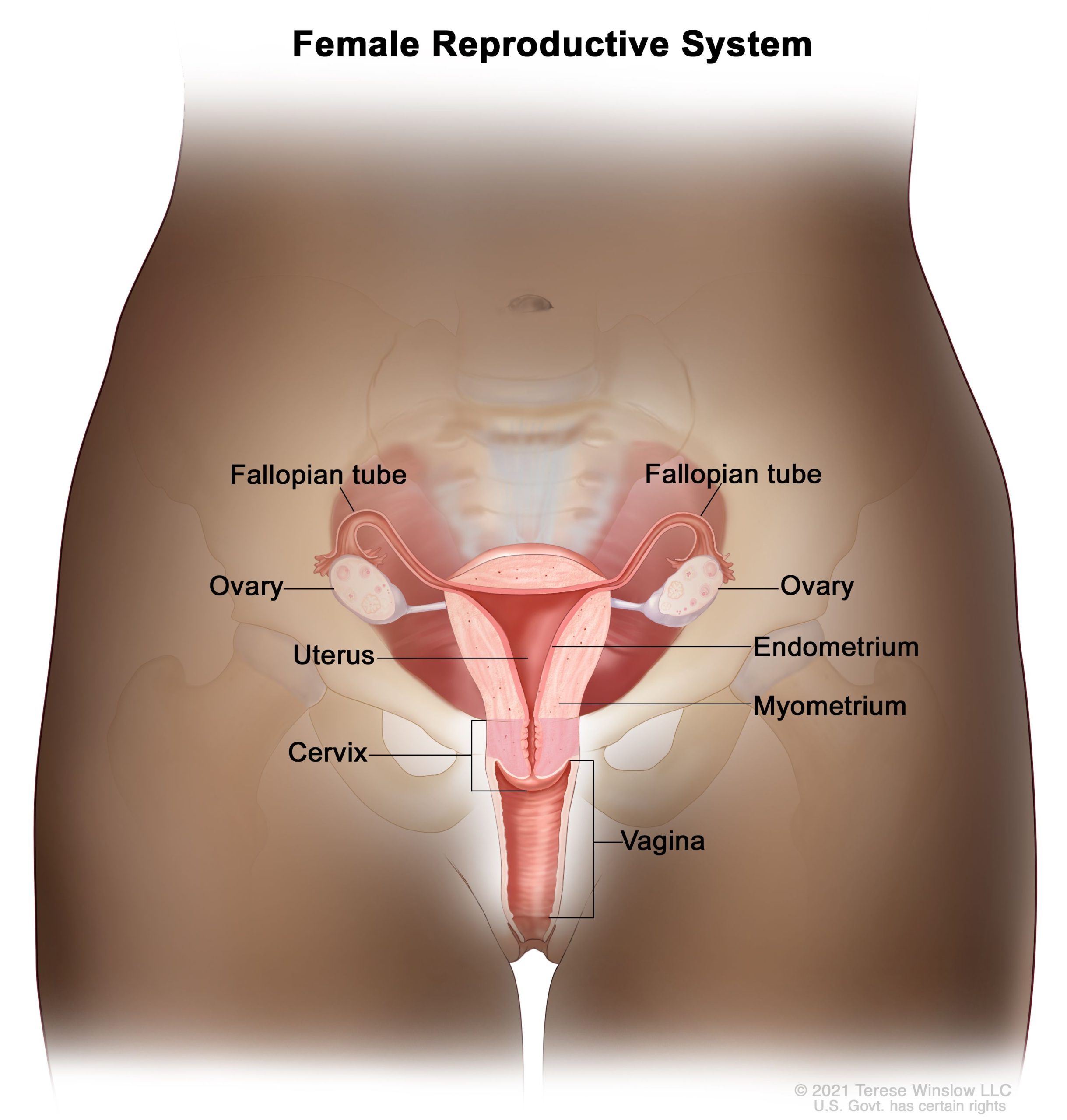
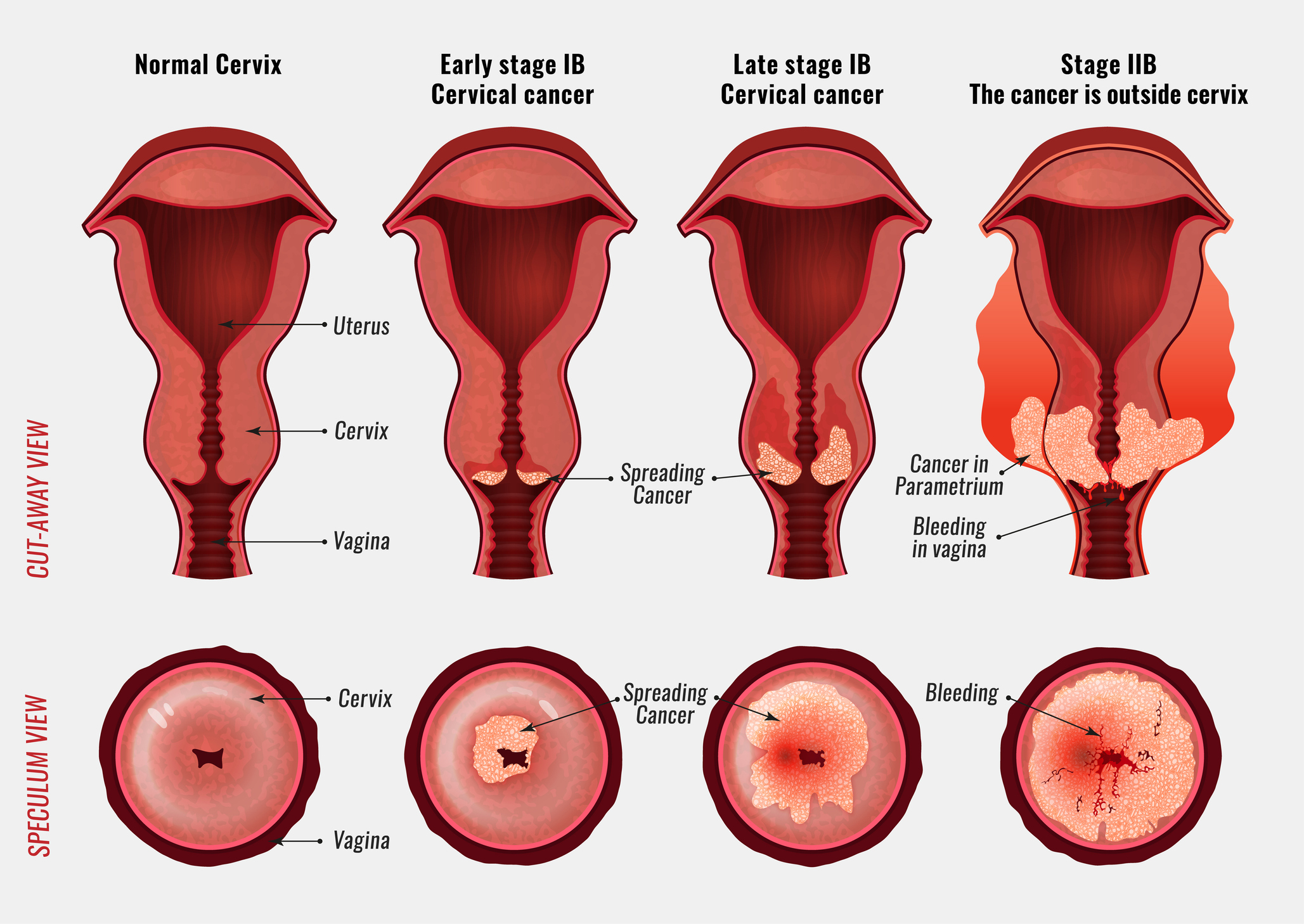
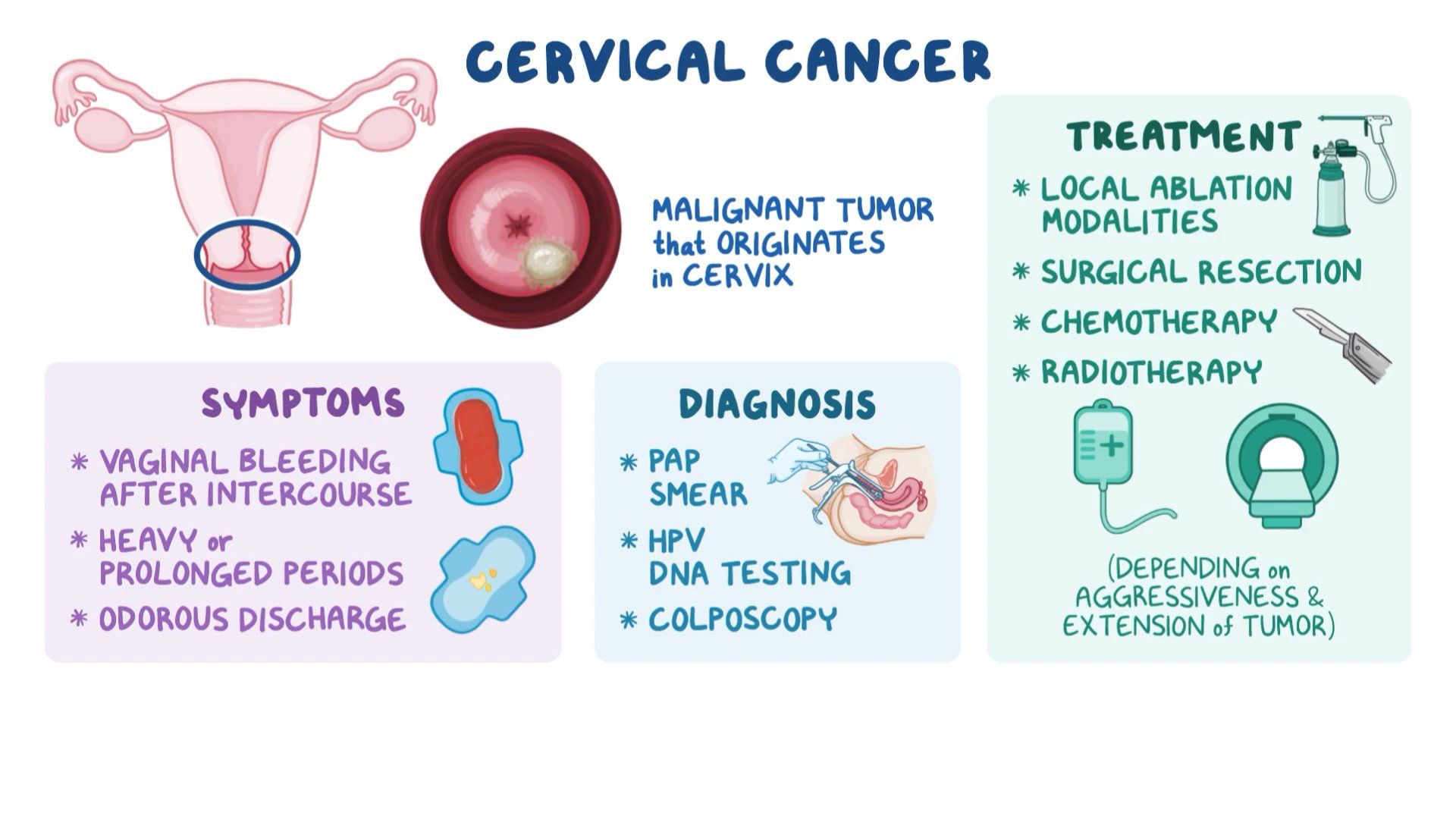
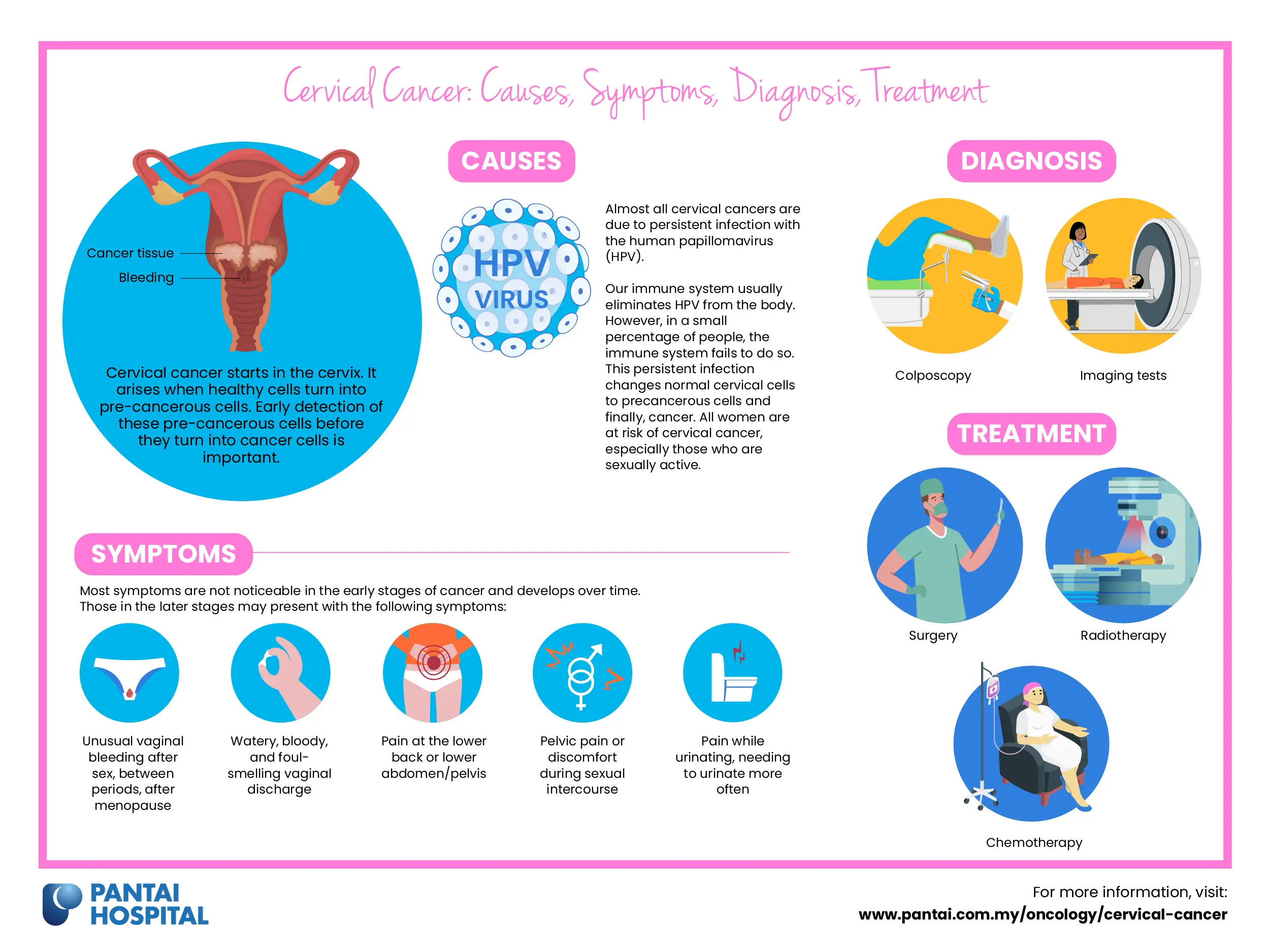
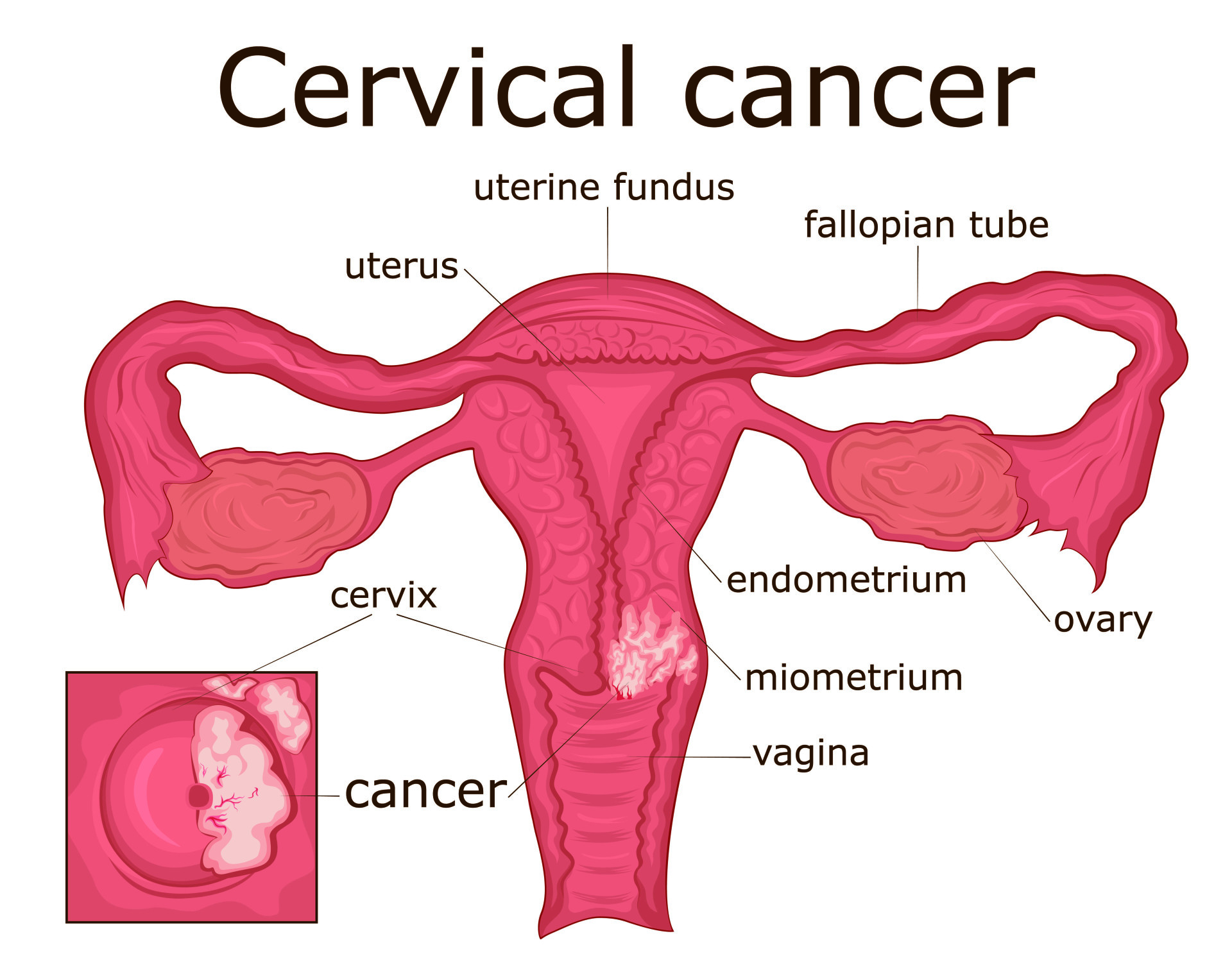
Cervical cancer is cancer that begins growing in or on the cervix, the neck of the uterus. Cancer happens when cells begin to grow and spread in an uncontrolled way.
Cervical cancer is divided into two main types, depending on which cervical cells are affected:
- Cervical squamous cell carcinoma is cancer of the squamous cells in the cervix and makes up about 70 per cent of all cervical cancers.
- Cervical adenocarcinoma affects the mucus-producing cells of the cervix and makes up about 25 per cent of cervical cancers.
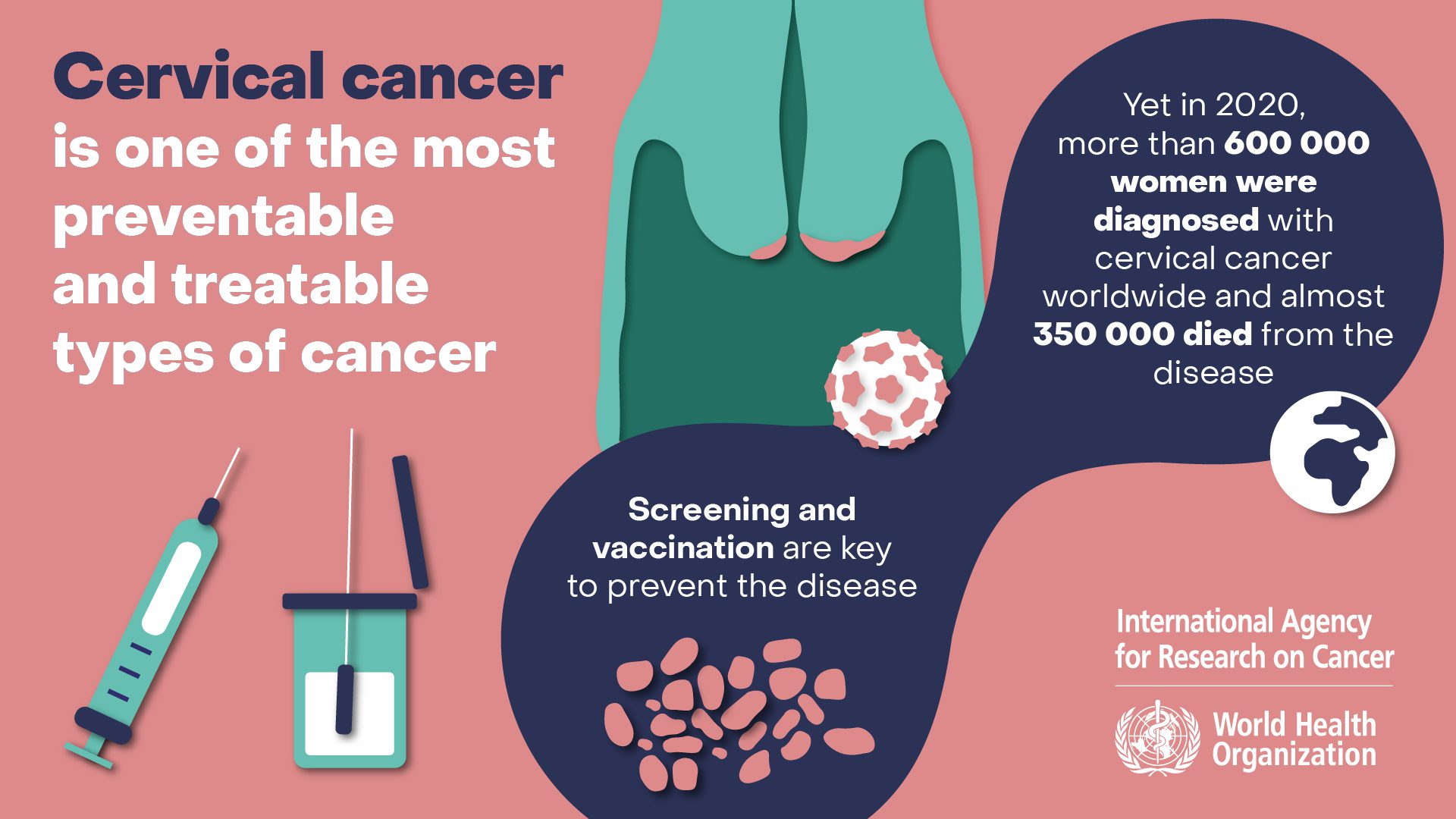
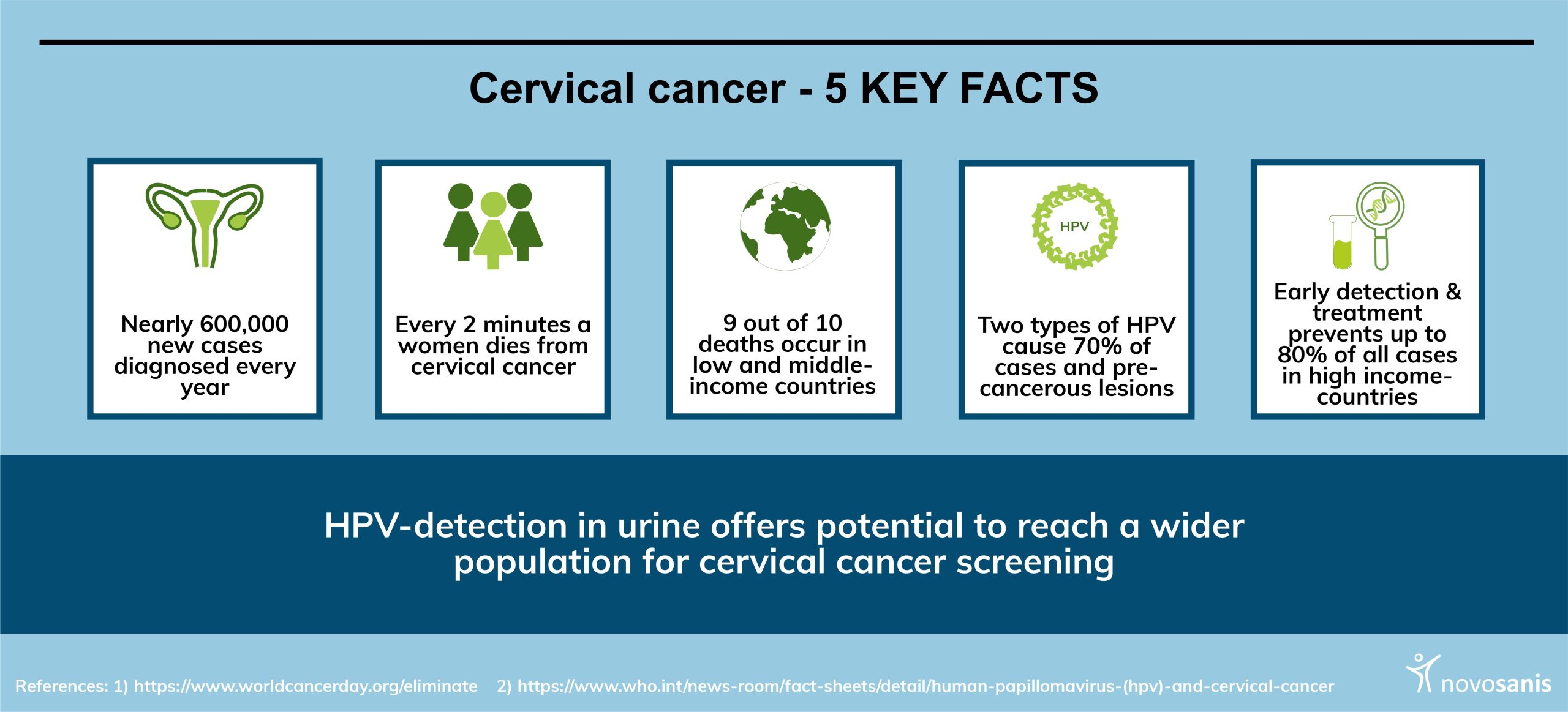
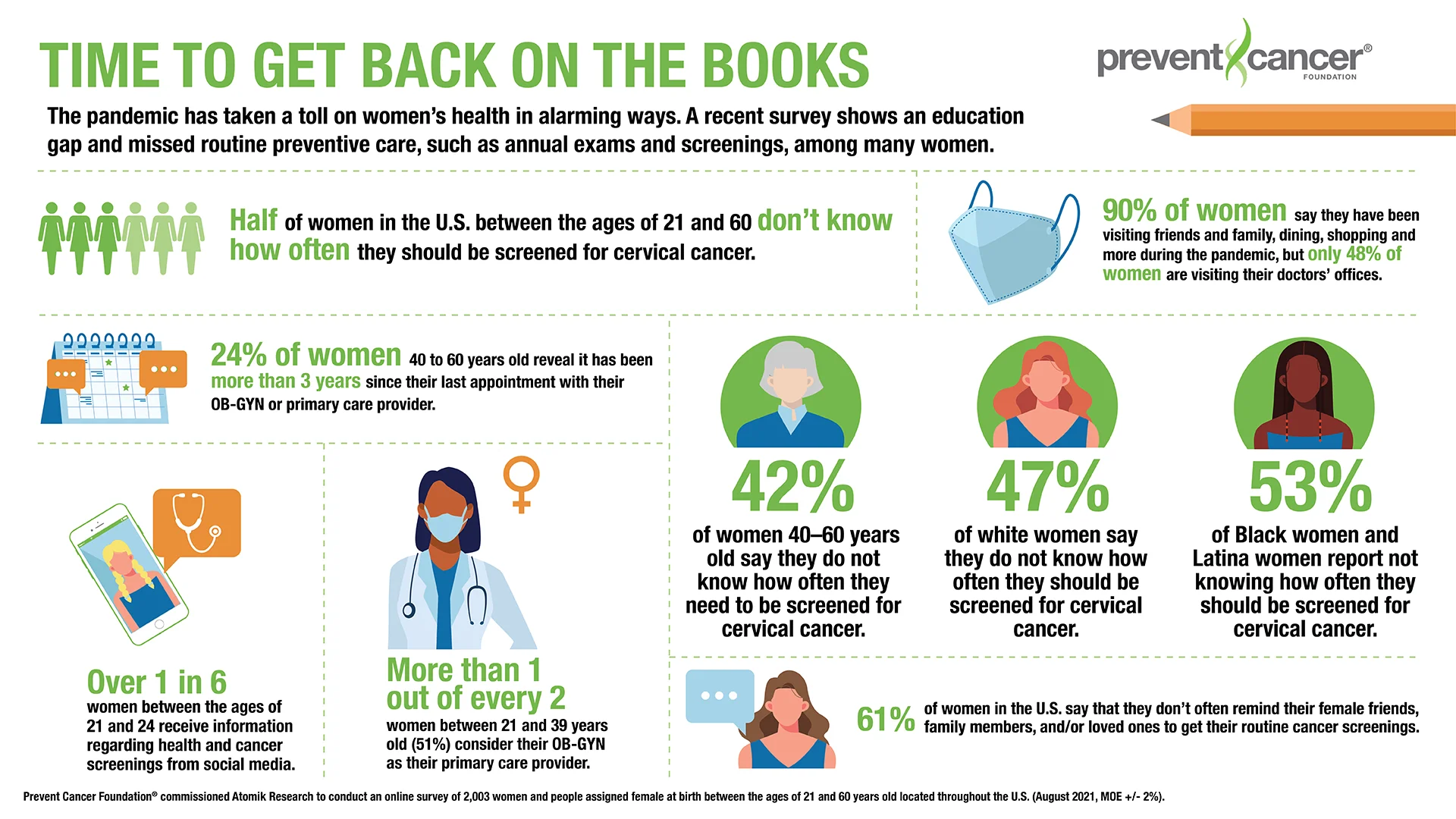
Cervical cancer affects about 900 Australians per year. The number of cases has decreased following the introduction of the national cervical cancer screening program in 1991, and again after the national HPV immunisation program was introduced in 2007.
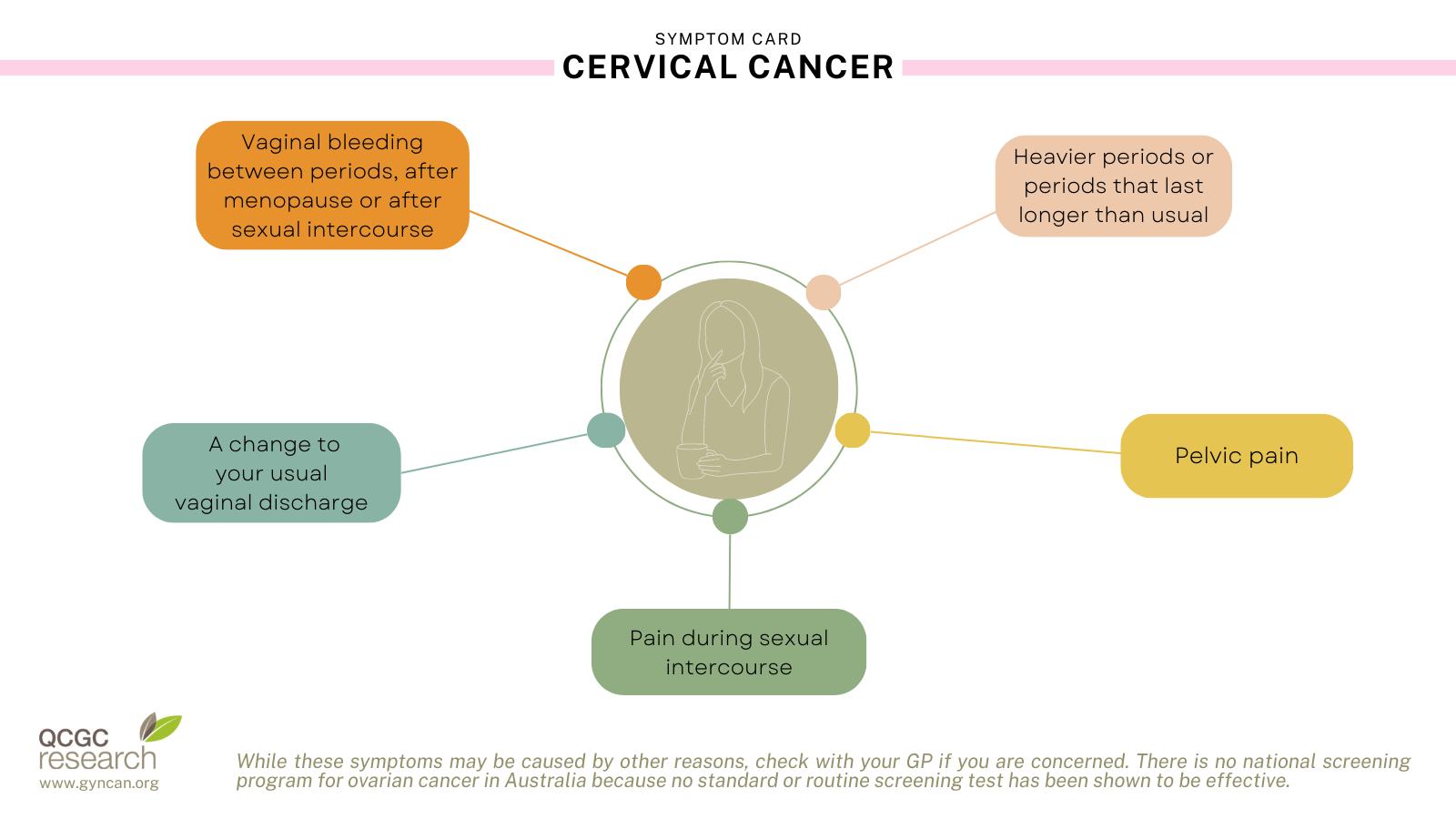
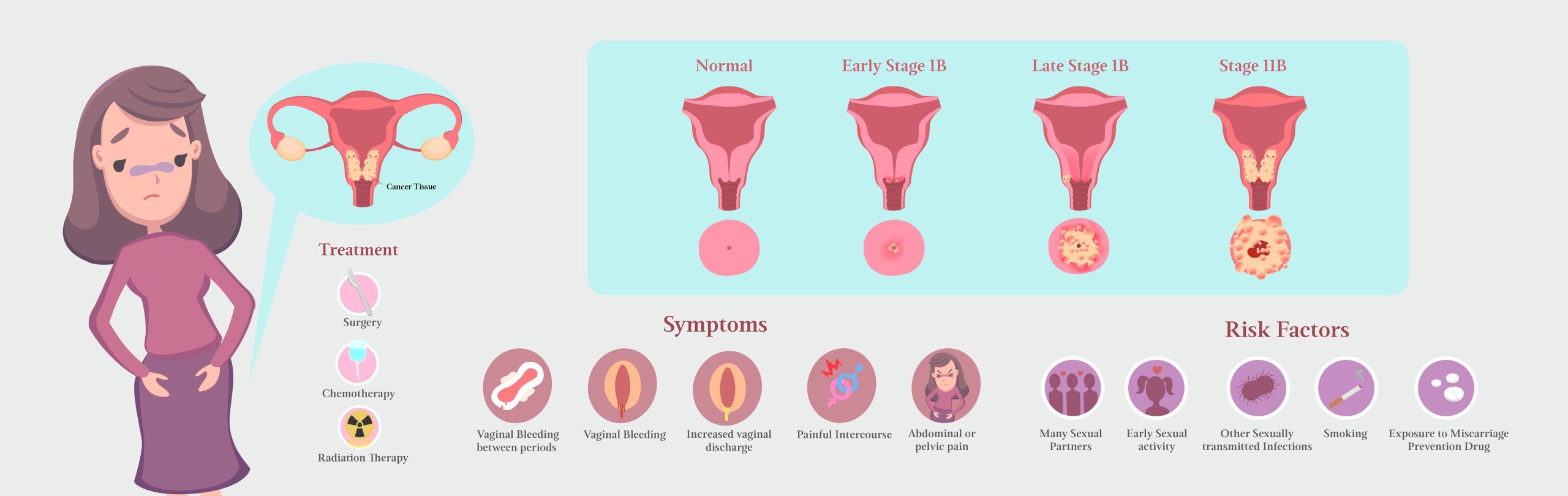
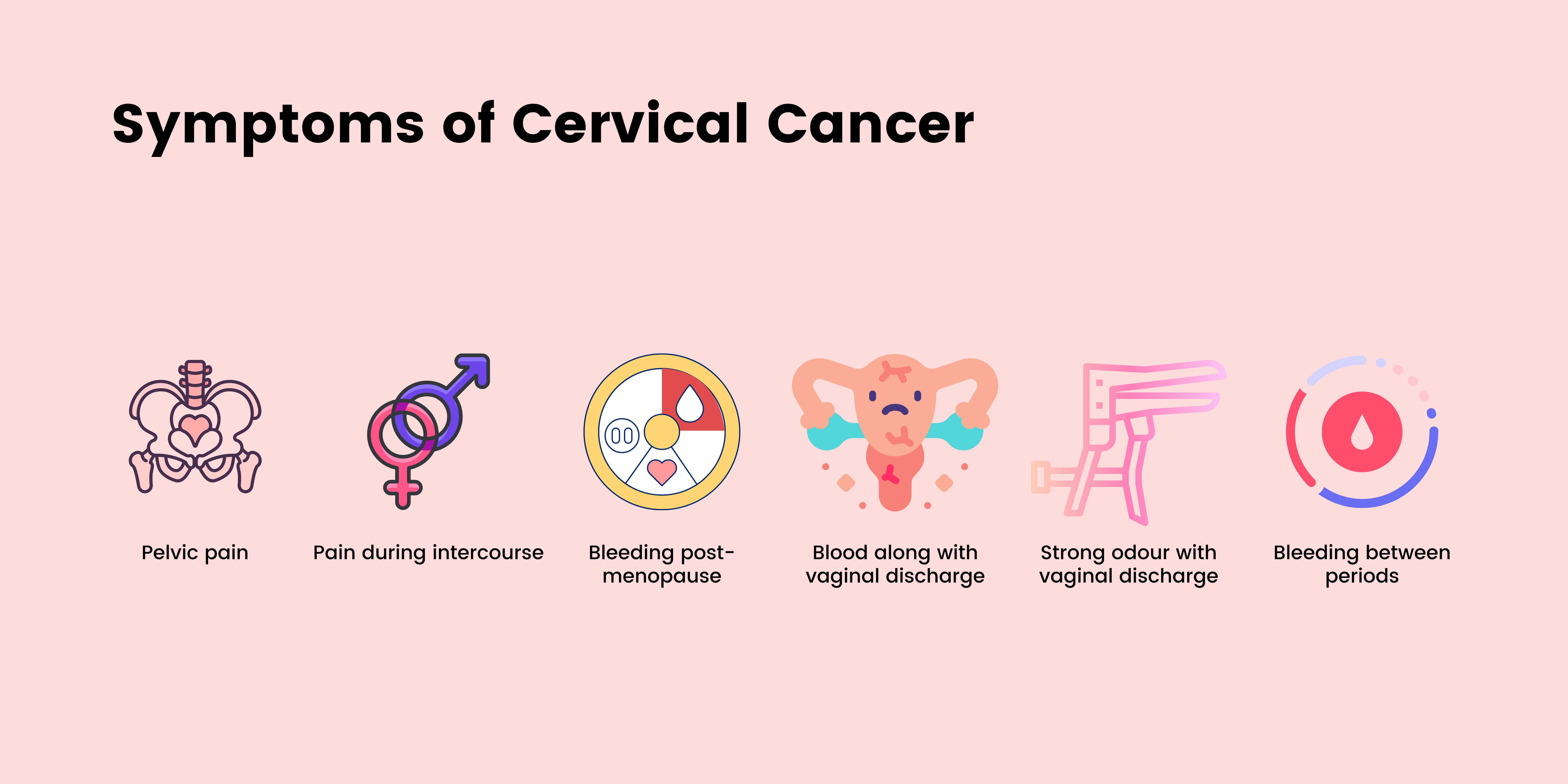
What are the symptoms of cervical cancer?
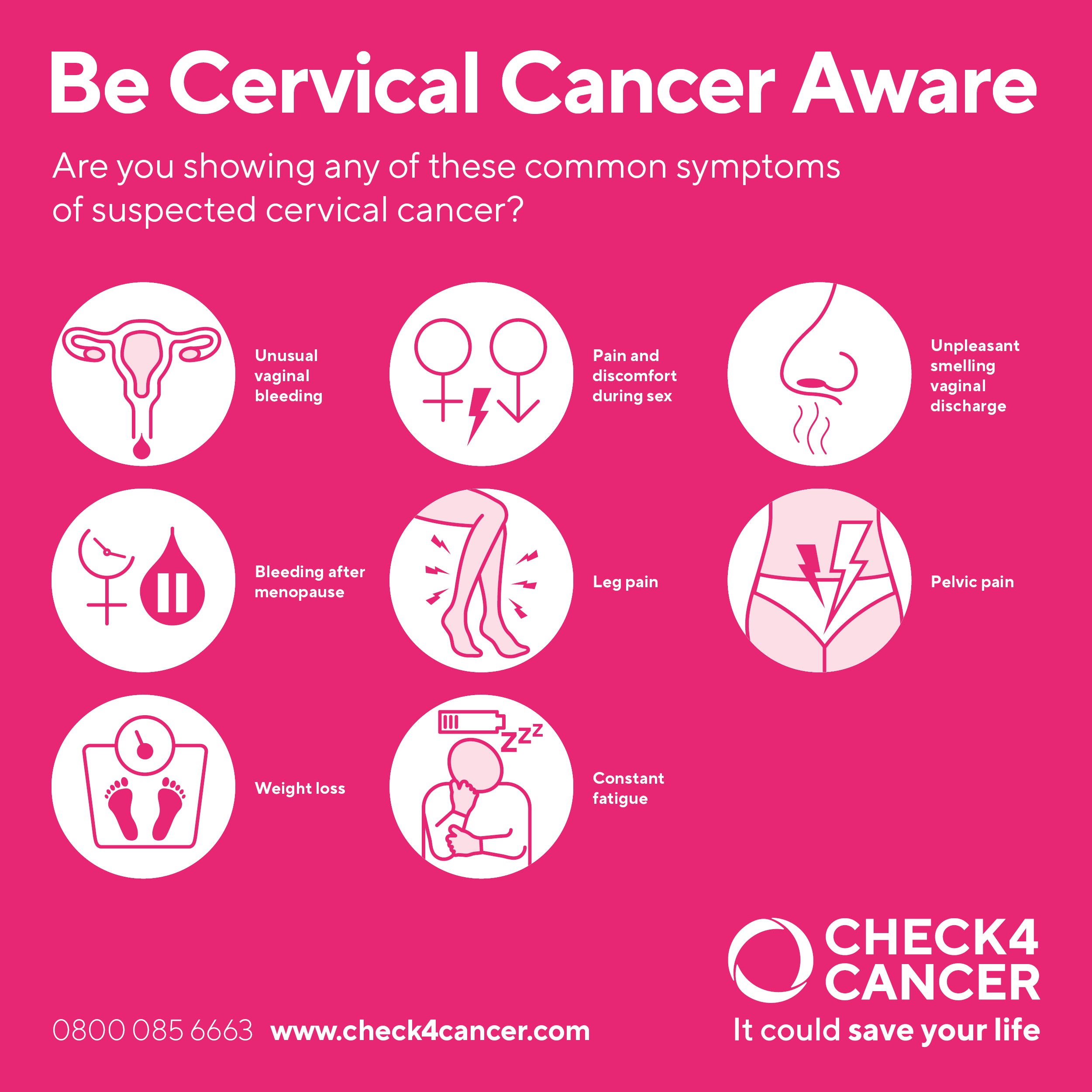
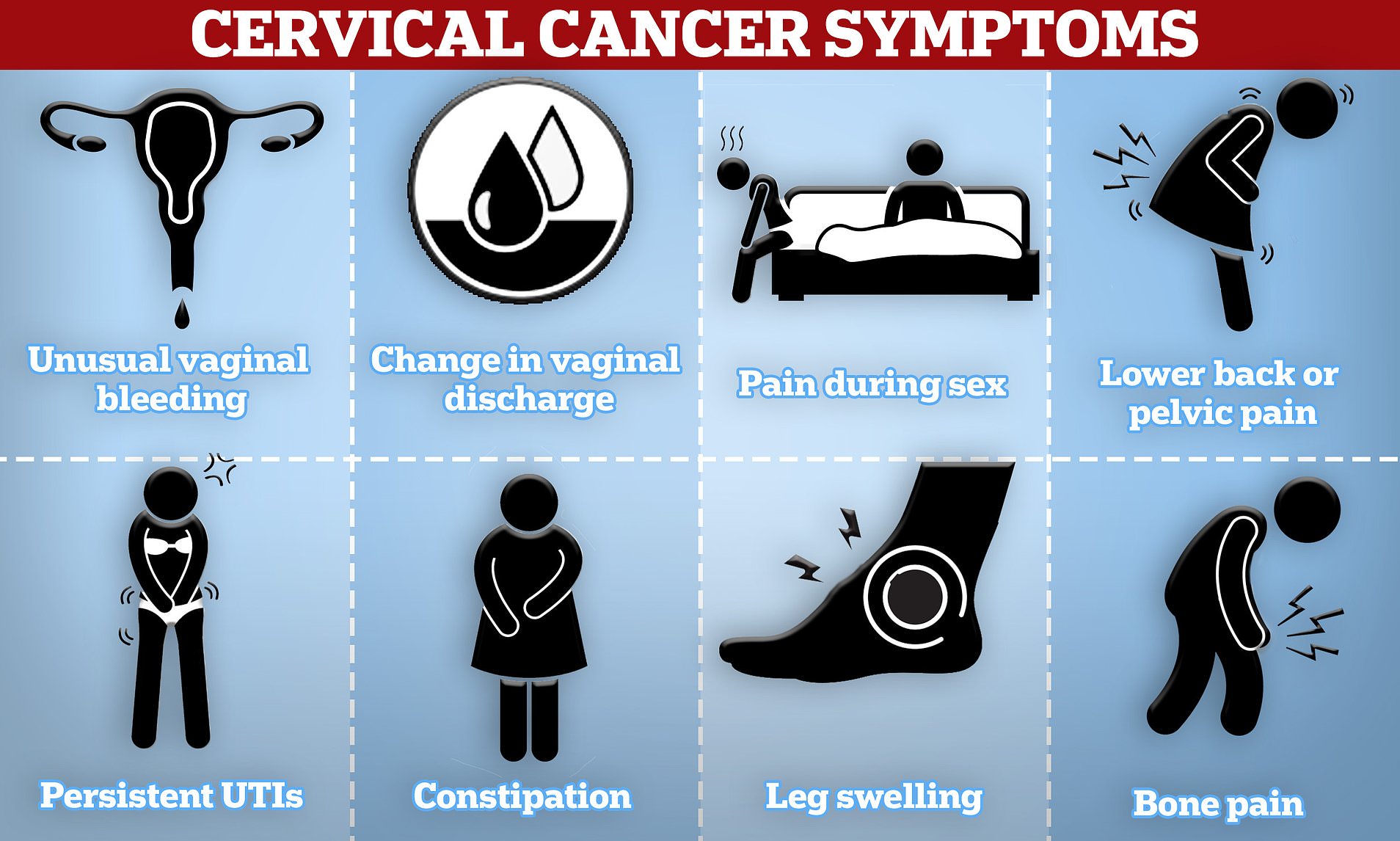
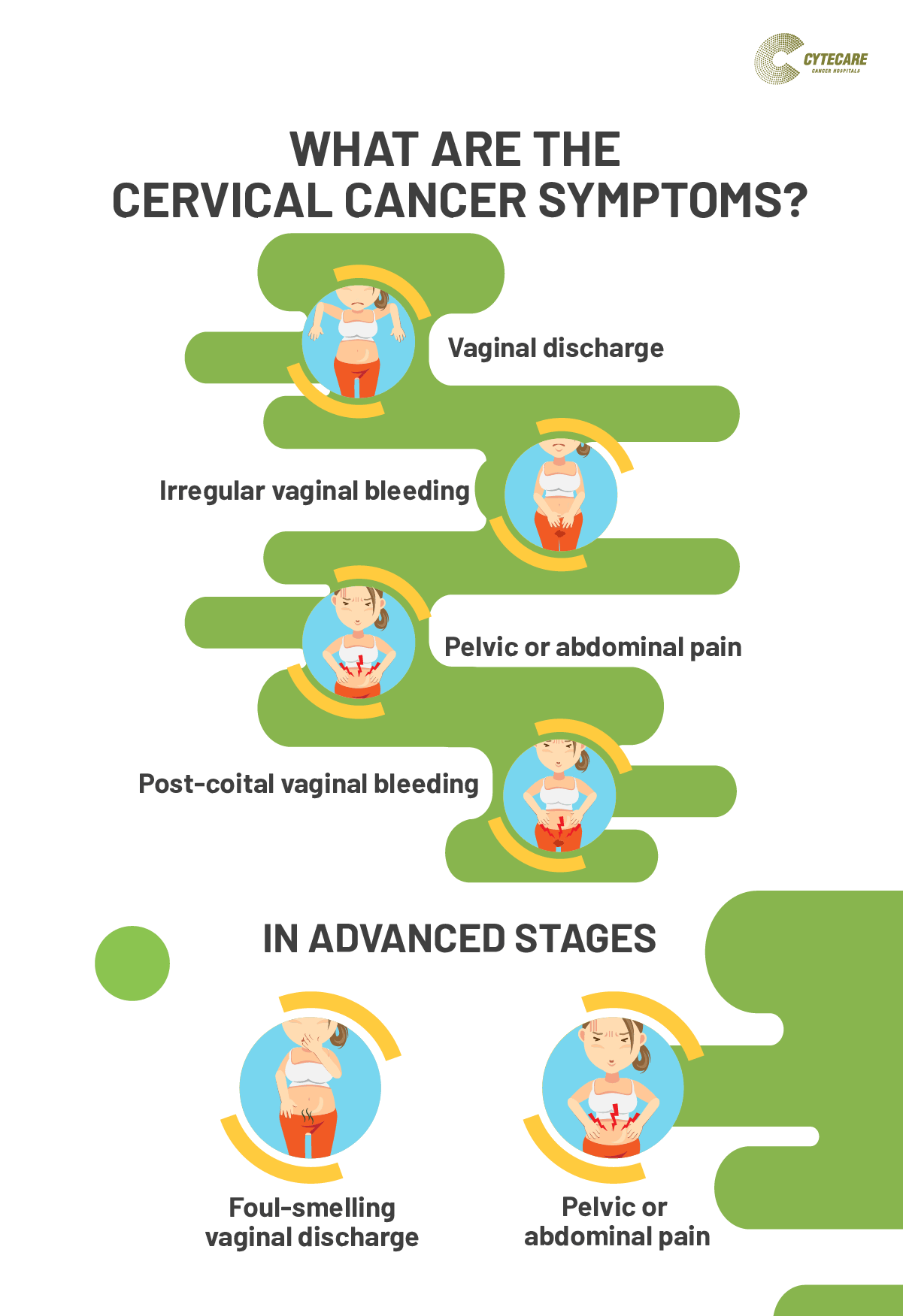
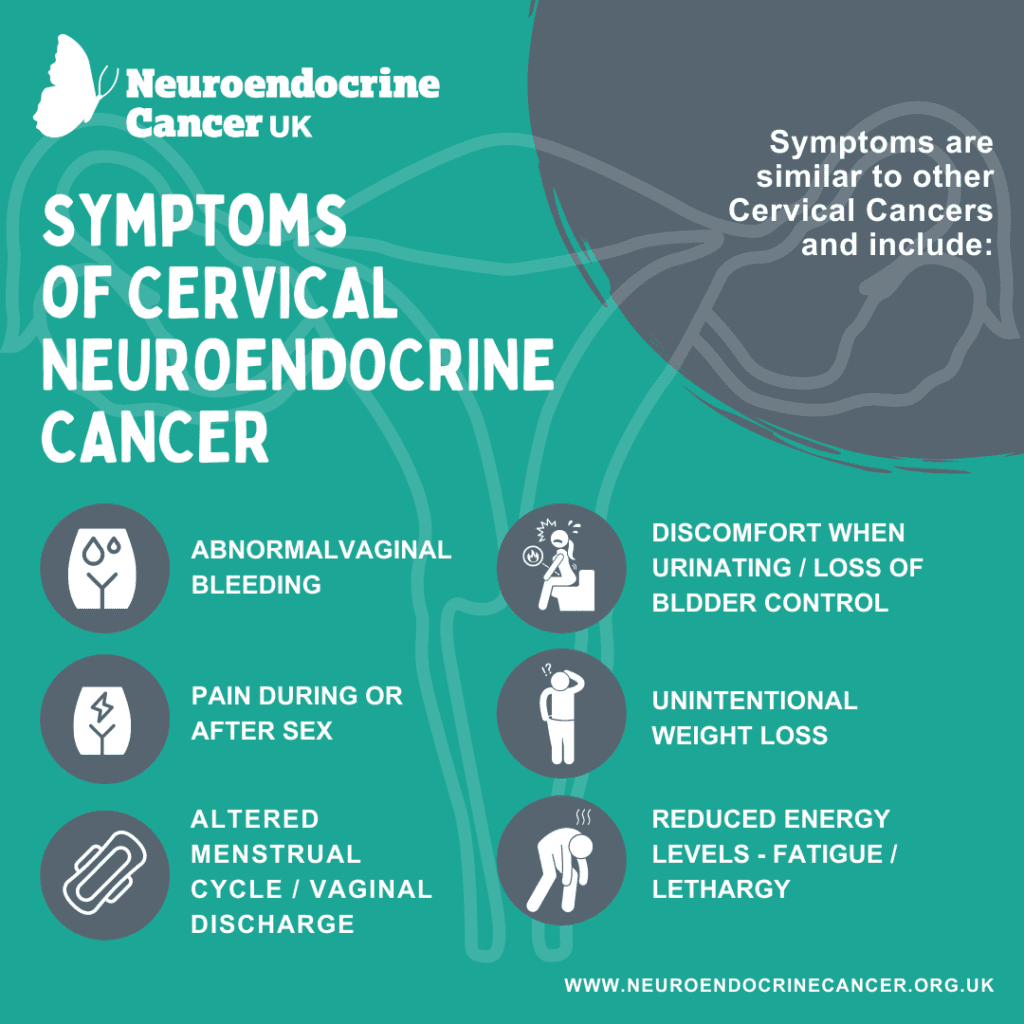
In its early stages, cervical cancer may cause very minor symptoms or none at all.
Common symptoms of early cervical cancer include:
- vaginal bleeding when you do not expect it — for example, between periods, after menopause or after sex
- heavier or longer periods than usual
- unusual vaginal discharge
- pelvic pain
- pain during sex
Symptoms of more advanced cancer are uncommon, but include:
- feeling very tired
- leg pain or swelling
- lower back pain
When should I see my doctor?
Many women experience unexpected vaginal bleeding and/or pelvic pain at different stages of life. In most cases, it’s not caused by cervical cancer. However, you should see your doctor if your symptoms concern you or they continue for longer than a couple of weeks.
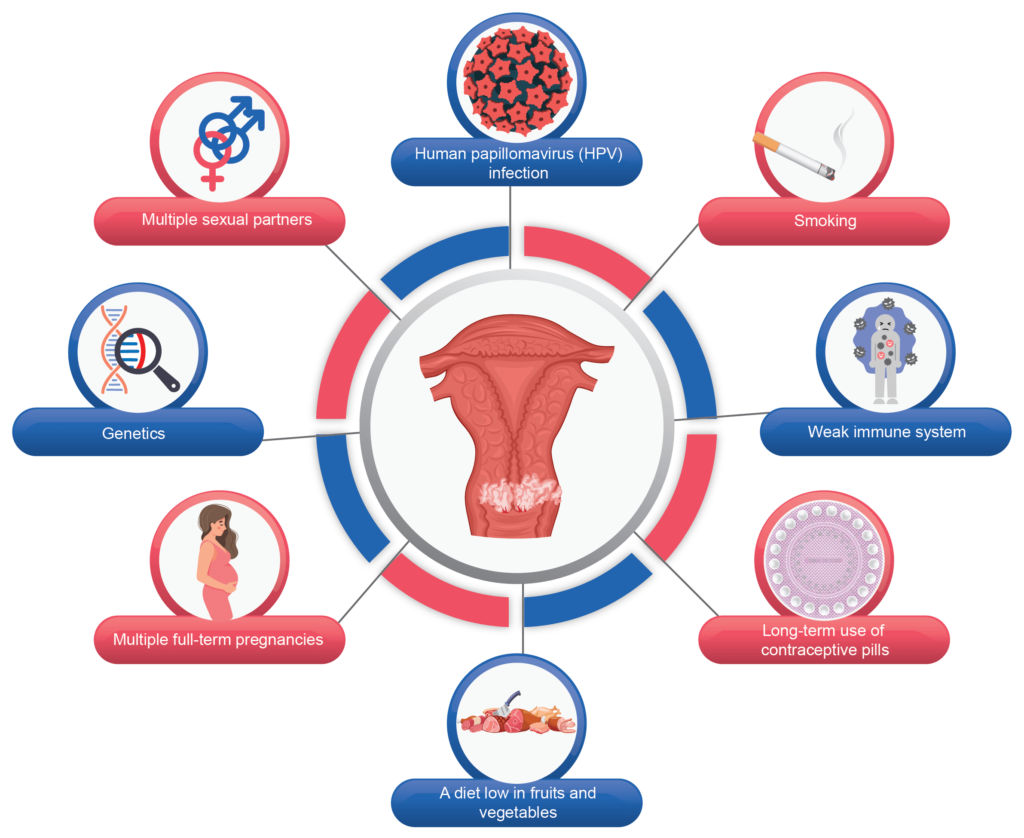
What causes cervical cancer?
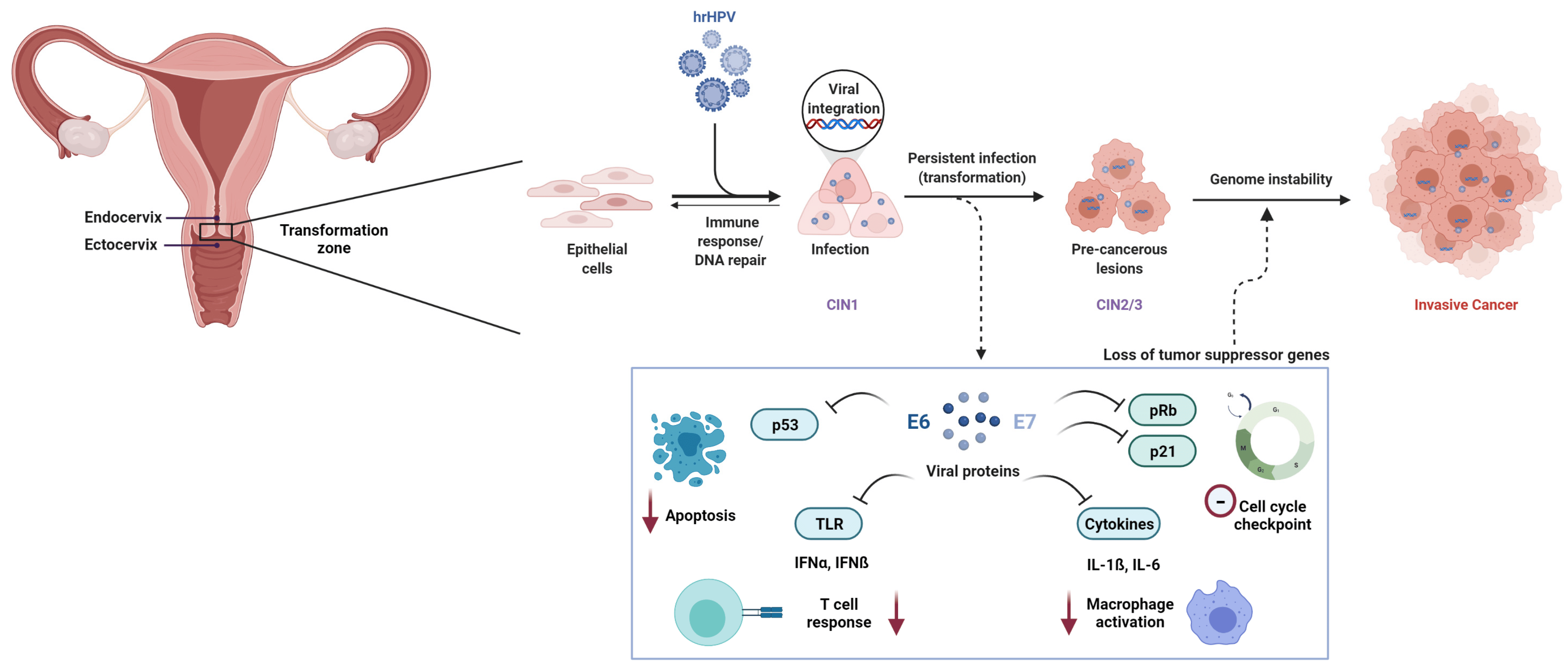
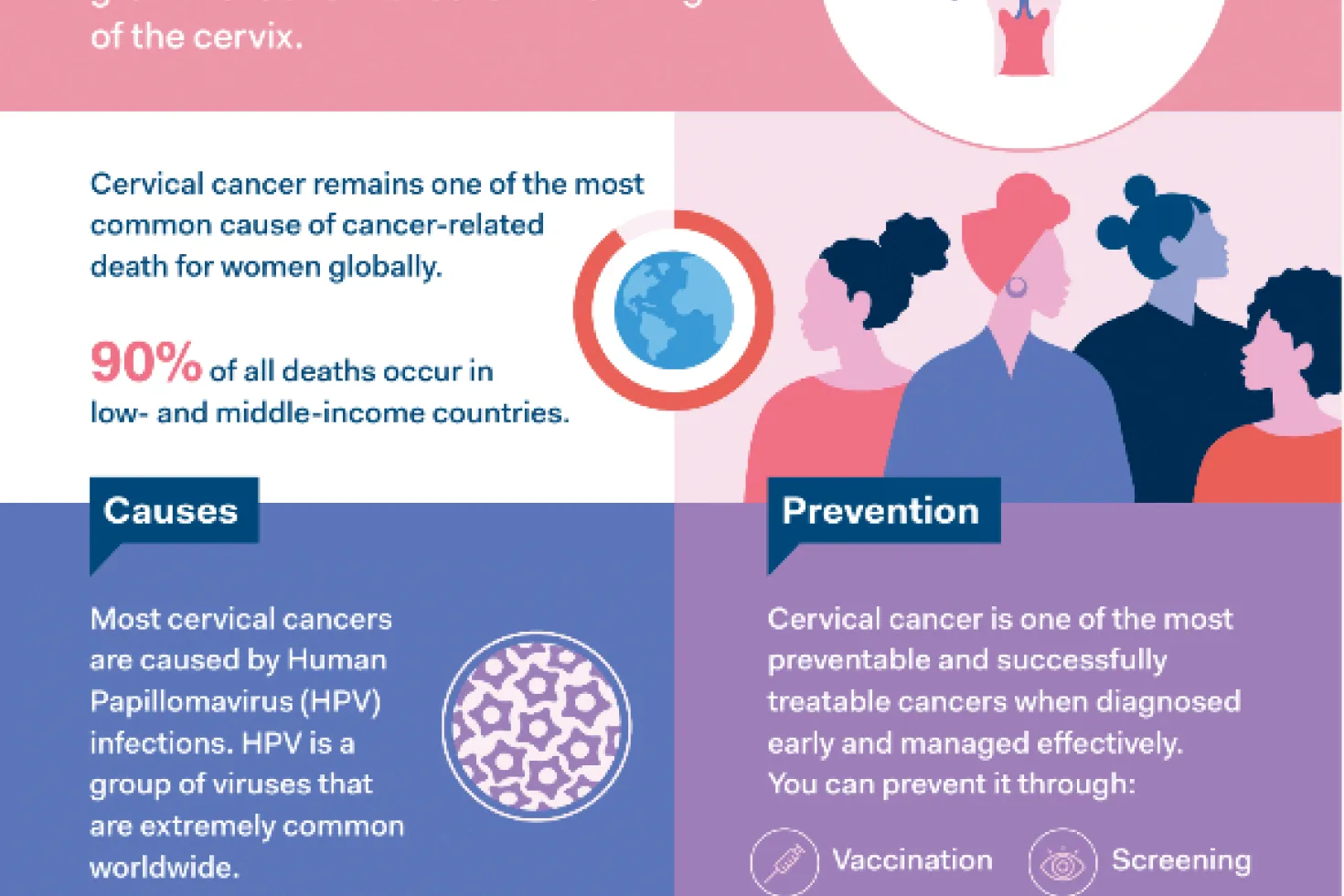
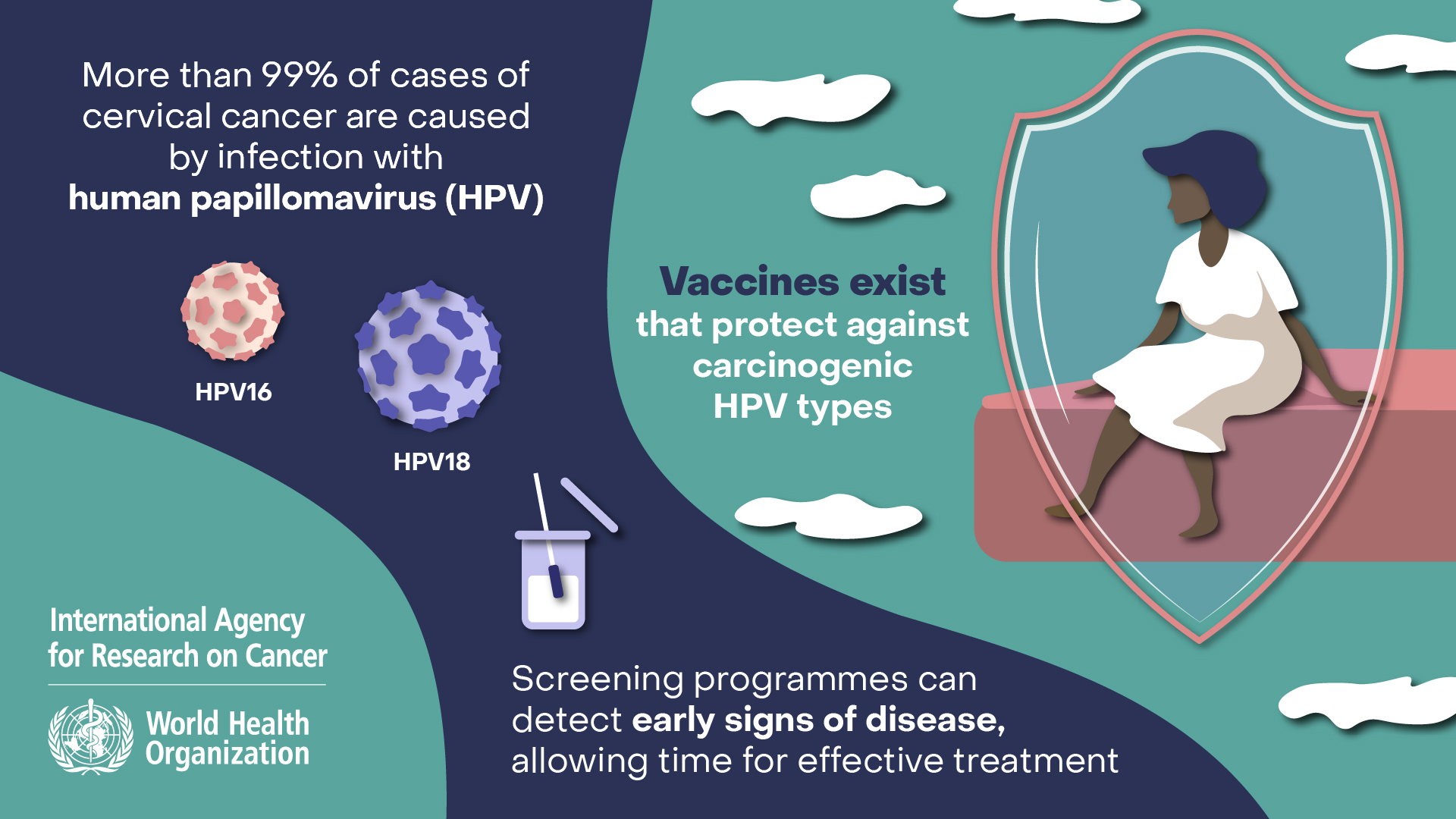
Most cases of cervical cancer follow infection with high-risk types of the genital human papilloma virus (HPV). Genital HPV infection is extremely common; about 4 in 5 people will be infected with at least one type during their lifetimes. Genital HPV is usually passed on during sexual contact with someone who is infected.
Most people who get HPV will have no symptoms and the virus will be quickly destroyed by their immune system. In some women, the infection does not clear and can cause changes in the cervix (precancerous changes), which may lead to cancer. These changes happen very slowly, usually over years.
Although HPV is the main cause of cervical cancer, there are other factors that can increase your risk of developing this cancer, including:
- smoking, including passive smoking
- long-term use of the oral contraceptive pill
- a weakened immune system
- exposure to the chemical diethylstilbestrol (DES)
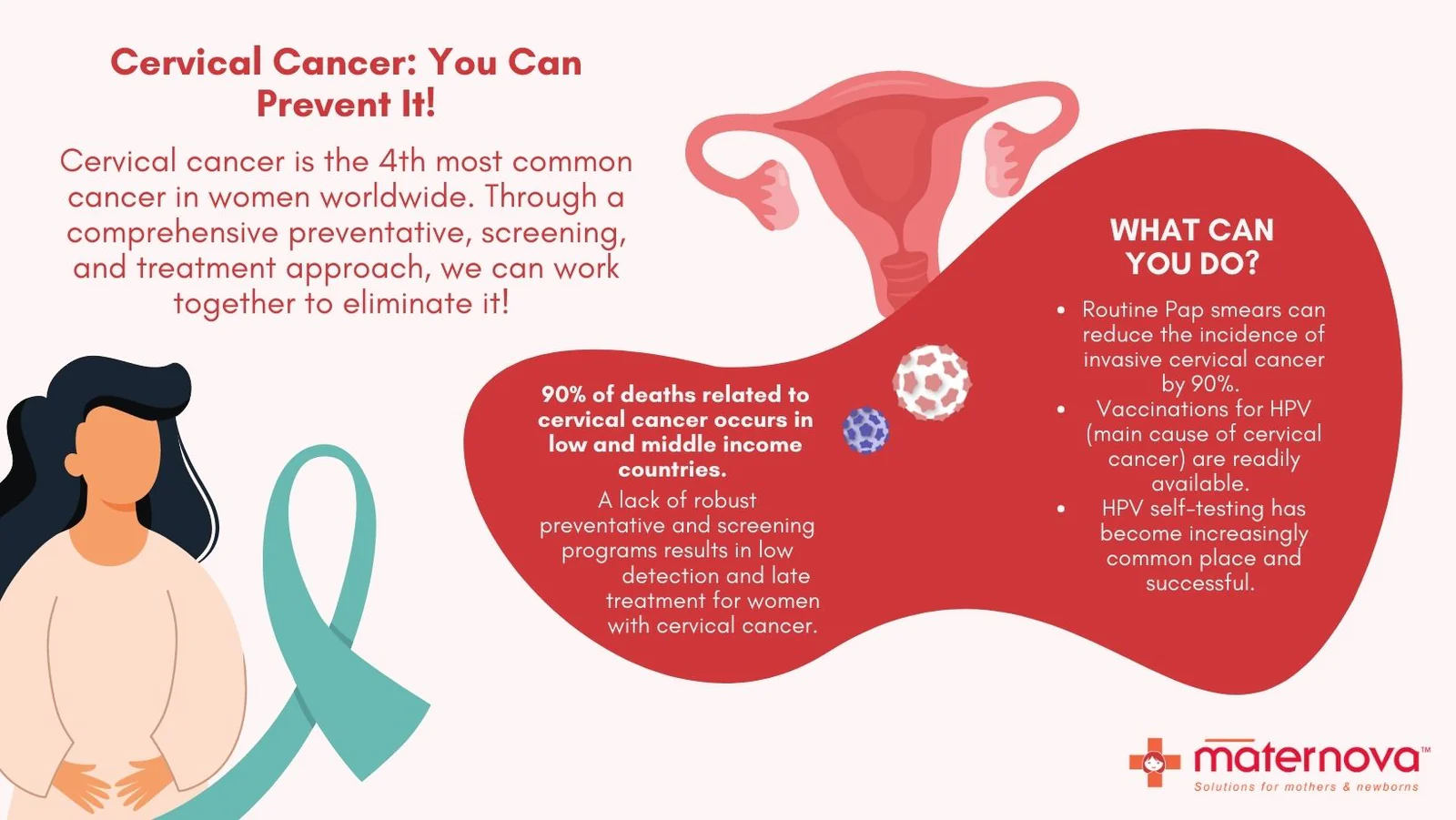
Can cervical cancer be prevented?
There are a few tools available in Australia today to prevent cervical cancer, and to catch it early if it does develop.
The HPV vaccine is available free to 12- and 13-year-old boys and girls on the National Immunisation Program Schedule. It is very effective at preventing infections from high-risk cancer-causing types of HPV.
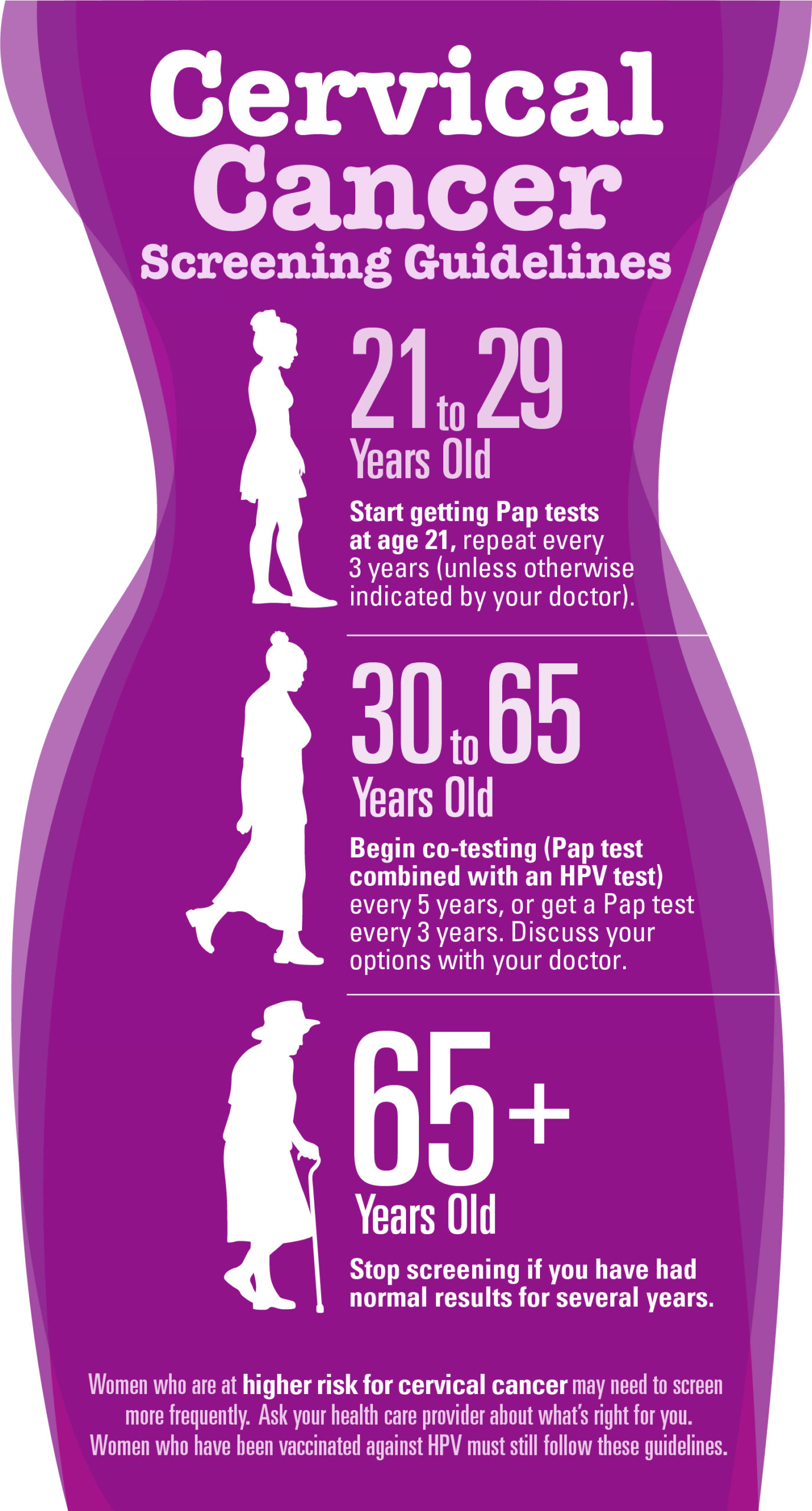
The National Cervical Screening Program recommends regular cervical screening tests. These replace Pap smear tests. Cervical screening tests check for high-risk types of HPV in a sample of cells taken from the cervix. This means that any early changes in the cervix that could later lead to cancer can be caught early and treated before they become cancer.
In July 2022, self-collection of samples for cervical screening tests became available to all people with a cervix aged 25 to 74. This means that you can take your own sample for the test from your vagina, using a swab. But, people who have symptoms of cervical cancer or are experiencing unusual bleeding, pain or discharge are not recommended for self-testing. Speak to your doctor about what’s right for you.
More information on self-collection is available from the Department of Health and Aged Care.
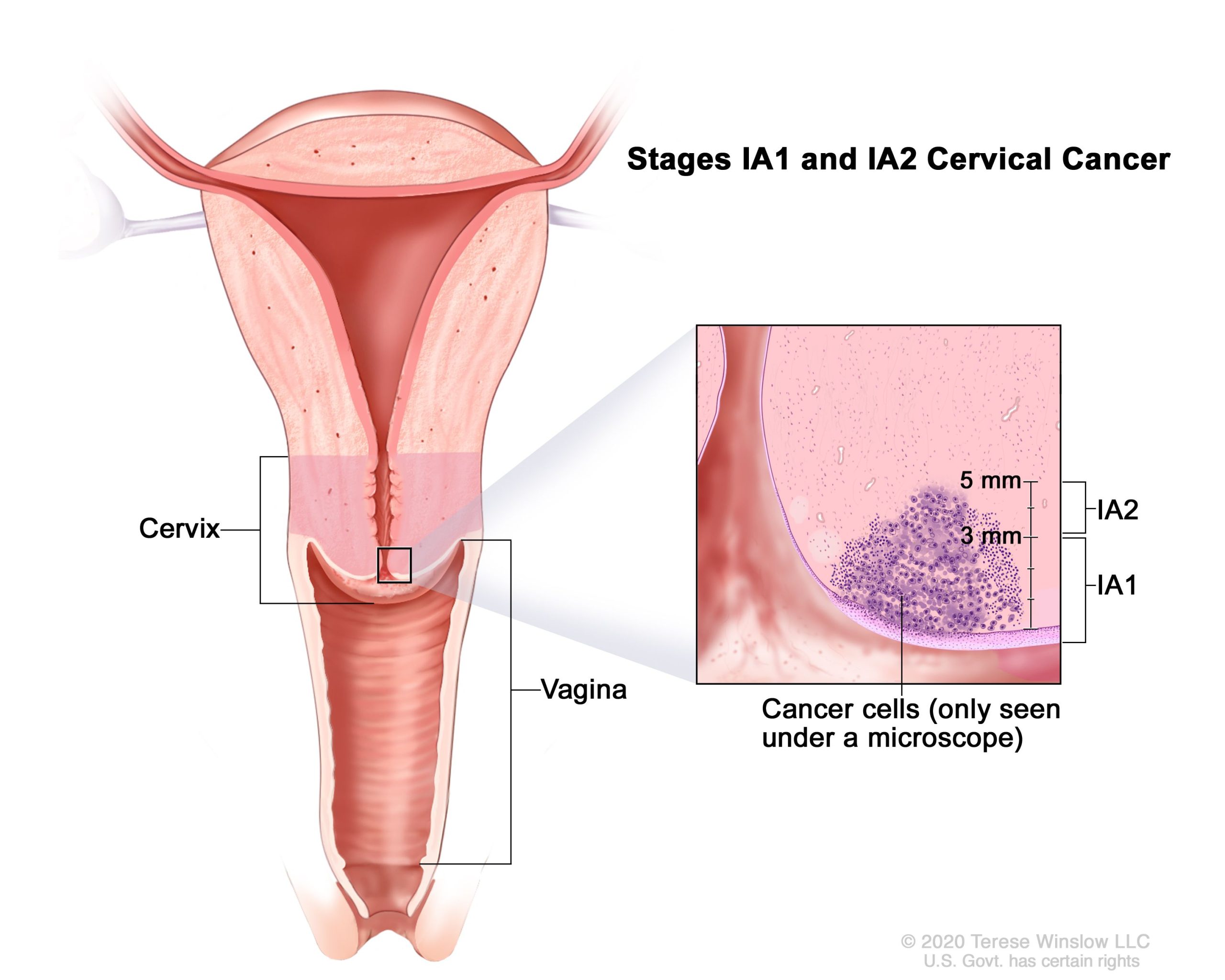
How is cervical cancer diagnosed?
Some cases of cervical cancer are diagnosed by tests following a positive cervical screening test in women with no symptoms.
If you have a positive cervical screening test, or symptoms that could be caused by cervical cancer, your doctor may arrange tests including:
- a colposcopy, a procedure in which a specialist doctor looks at your cervix with a magnifying device (similar to binoculars), to look for abnormal cells that could be cancer
- a biopsy, which involves removing a sample of your cervix and checking it under a microscope for cancer cells — this can occur during colposcopy
- blood tests to check your kidney and liver function and the state of your general health.
- imaging scans such as a CT scan and/or an MRI to look for signs of cancer spread inside your body
How is cervical cancer treated?
If the above tests show precancerous cell changes, there are treatment options to remove these cells to prevent them developing into cervical cancer. The different procedures used to treat precancerous cells are:
- a wire loop excision (also known as a LLETZ or LEEP), which uses a thin loop of wire heated with electricity to remove the abnormal area of tissue in the cervix.
- a cone biopsy, in which the area of abnormal cells is removed using a scalpel instead of a wire.
- in some cases, laser surgery is used to destroy abnormal cells on the cervix using a strong, hot light (a laser), which is shone through the vagina.
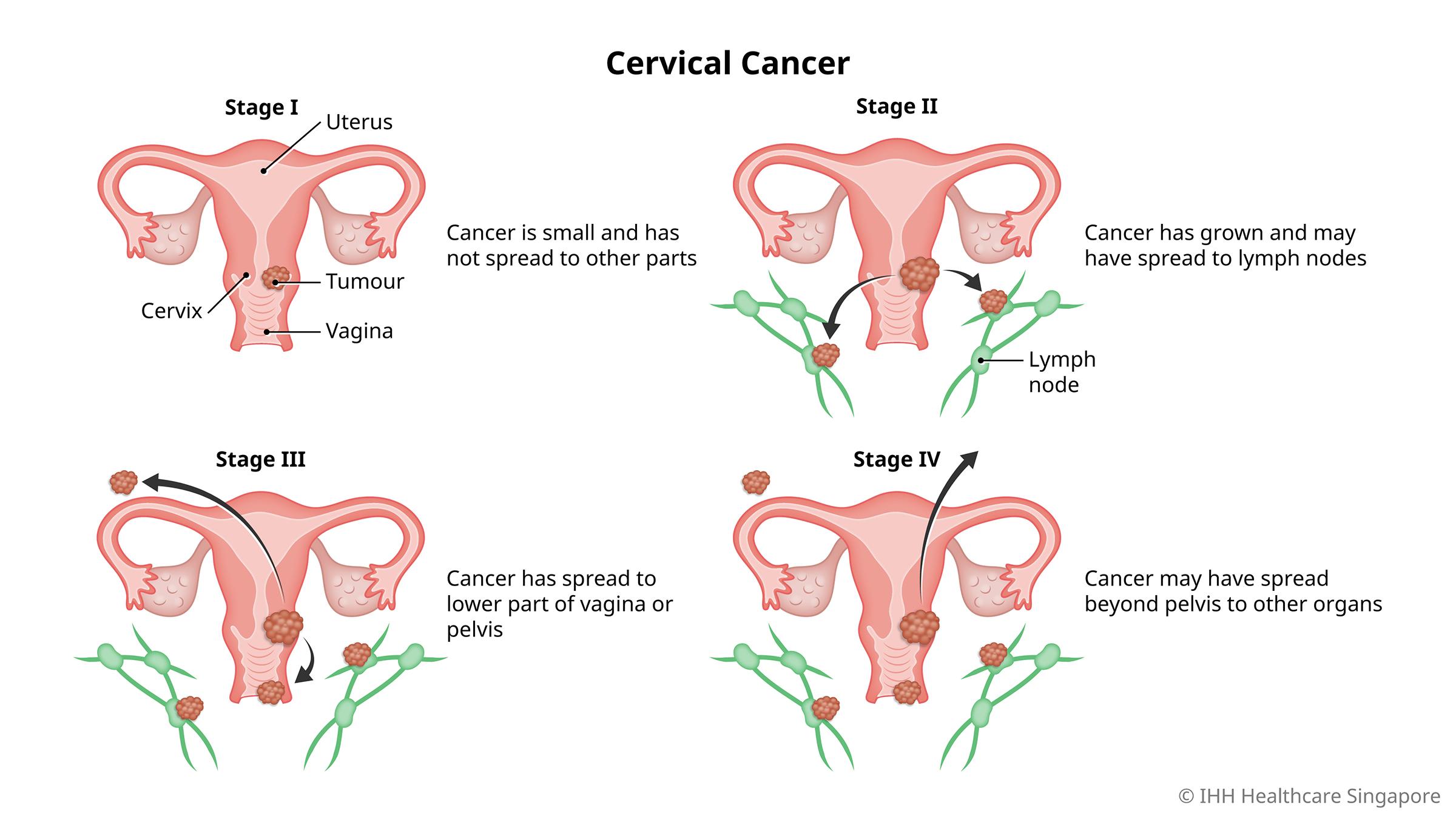
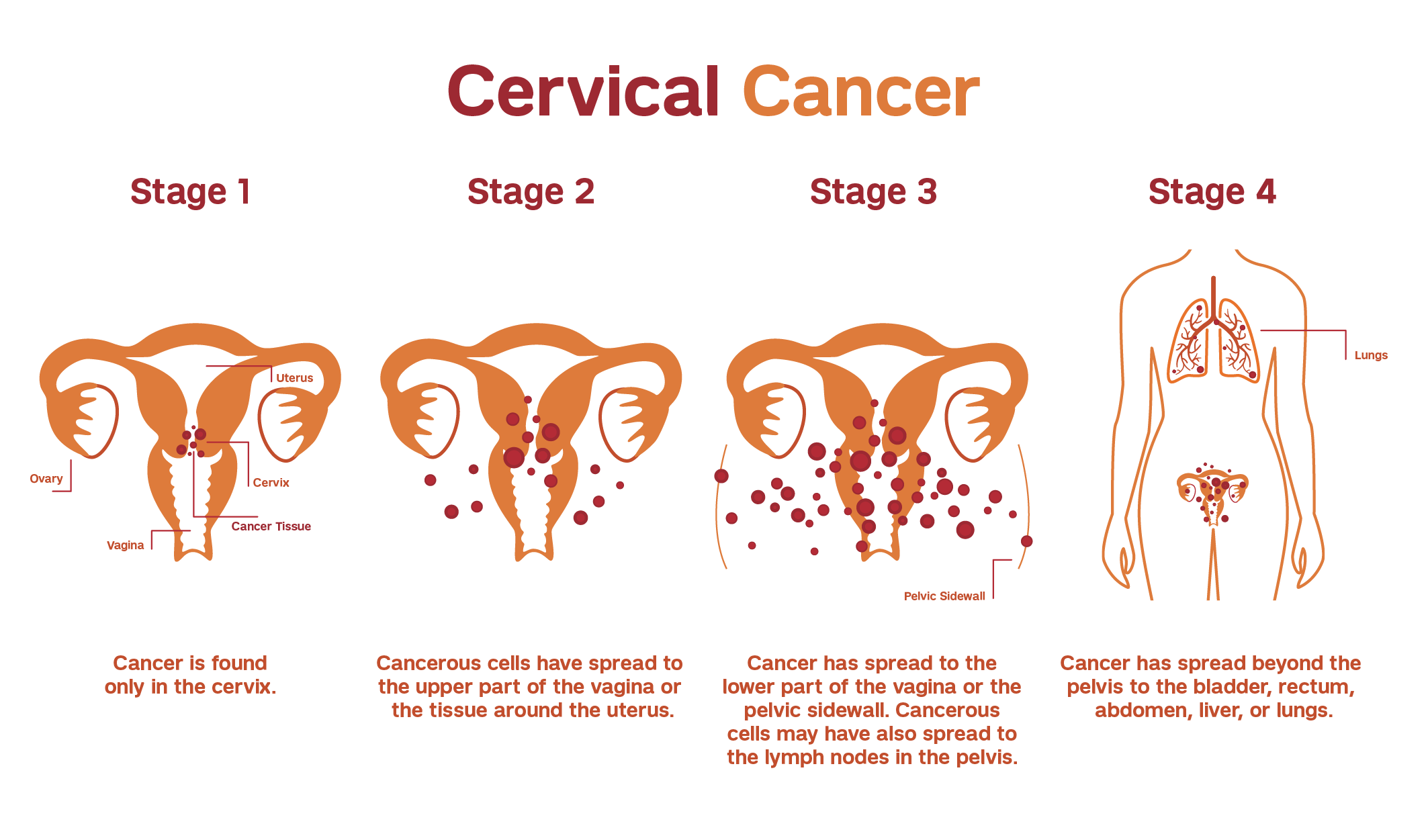
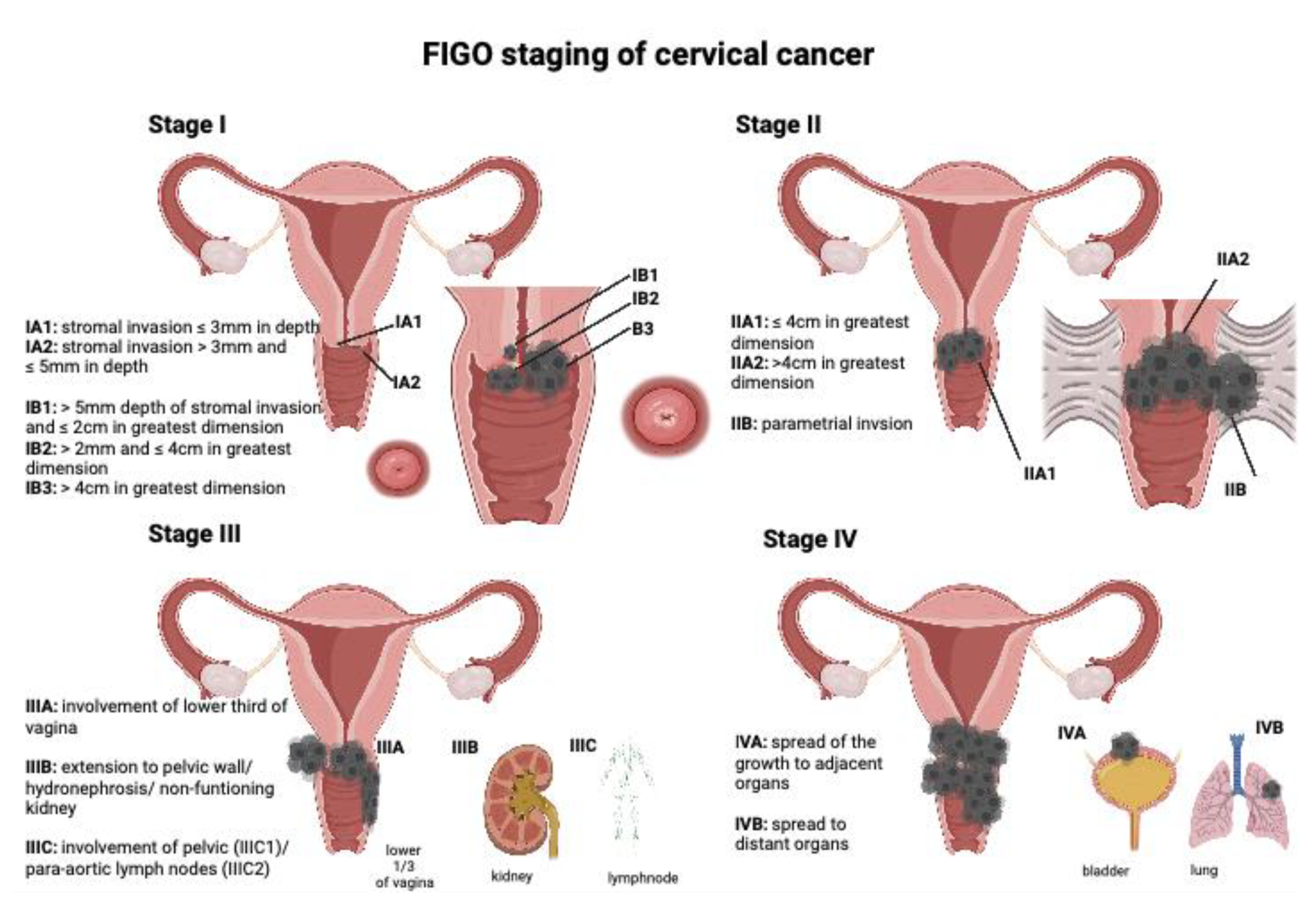
If pre-cancerous cells are not treated, they can progress to cervical cancer. Many cases of cervical cancer are found early and are treated with surgery. If cervical cancer spreads to other parts of the body (metastasis), a patient may need to undergo other treatments such as radiation and chemotherapy.
There are many different procedures and surgeries used to treat cervical cancer, including:
- a cone biopsy, which removes a cone of tissue around the cancer with a scalpel
- a trachelectomy, which involves removing the upper part of the vagina and part or all of the cervix — this may be an option for those who wish to have children after treatment
- a hysterectomy, which involves removing the uterus, cervix, and the top of the vagina. It is the most common operation used to treat cervical cancer. If your uterus is removed, you will not be able to have children
- a bilateral salpingectomy — this involves removing both fallopian tubes and may be performed at the same time as a hysterectomy
- a bilateral salpingo-oophorectomy, which involves removing both fallopian tubes and both ovaries. It can also be done at the same time as a hysterectomy. Removing the ovaries will cause sudden menopause in women who are pre-menopausal and means you will no longer be able to have children.
Your doctor will consider many factors when deciding which surgery is right for you, including:
- the type of cancer
- the size of the cancer and how far it has spread (its stage)
- your age and general health
- if you are pre- or post-menopausal
- whether you want to have children in the future
What are the complications of cervical cancer?
Like most cancers, cervical cancer can spread to other parts of the body and cause serious complications. However, when cervical cancer is caught and treated early, the expected outcome is usually very good.
Treatments for cervical cancer can affect your ability to fall pregnant and/or carry a pregnancy to term. Smaller surgical procedures performed on the cervix may increase the chance of miscarriage in future pregnancies.
The larger surgeries, which remove the uterus (hysterectomy), fallopian tubes (bilateral salpingectomy) or ovaries (bilateral oophorectomy), may mean you will not be able to have children.
Cancer treatments, including surgery, chemotherapy, and radiotherapy, may all cause a range of side effects. Your medical team is very experienced at helping people manage these side effects and can give you advice and support to manage them.
Other questions you might have
Can I still become pregnant?
Cervical cancer itself may not affect your ability to conceive. However, some surgeries or treatments used to treat cervical cancer might affect your ability to have children. If fertility is important to you, you should discuss options for preserving fertility with your doctor before starting treatment.
Does a cervical biopsy hurt?
Cervical biopsies can be uncomfortable but are usually over quickly. You may wish to speak to your doctor about options for pain relief if you are concerned.
Are cervical biopsies accurate?
No medical test is 100 per cent accurate. Cervical biopsies are taken and checked by specialist doctors and are usually very accurate. If you are concerned, you may wish to seek a second opinion from another specialist.
Is cervical cancer hereditary?
HPV causes most cases of cervical cancer, and it’s not hereditary. However, you may be at a higher risk for cervical cancer if you have a first-degree relative with a history of cervical cancer.