Key facts
- Breast cancer occurs when cells in the breast grow abnormally and form a tumour.
- Symptoms may include a lump in the breast, discharge from the nipple, and changes in the appearance or texture of the breast or nipple.
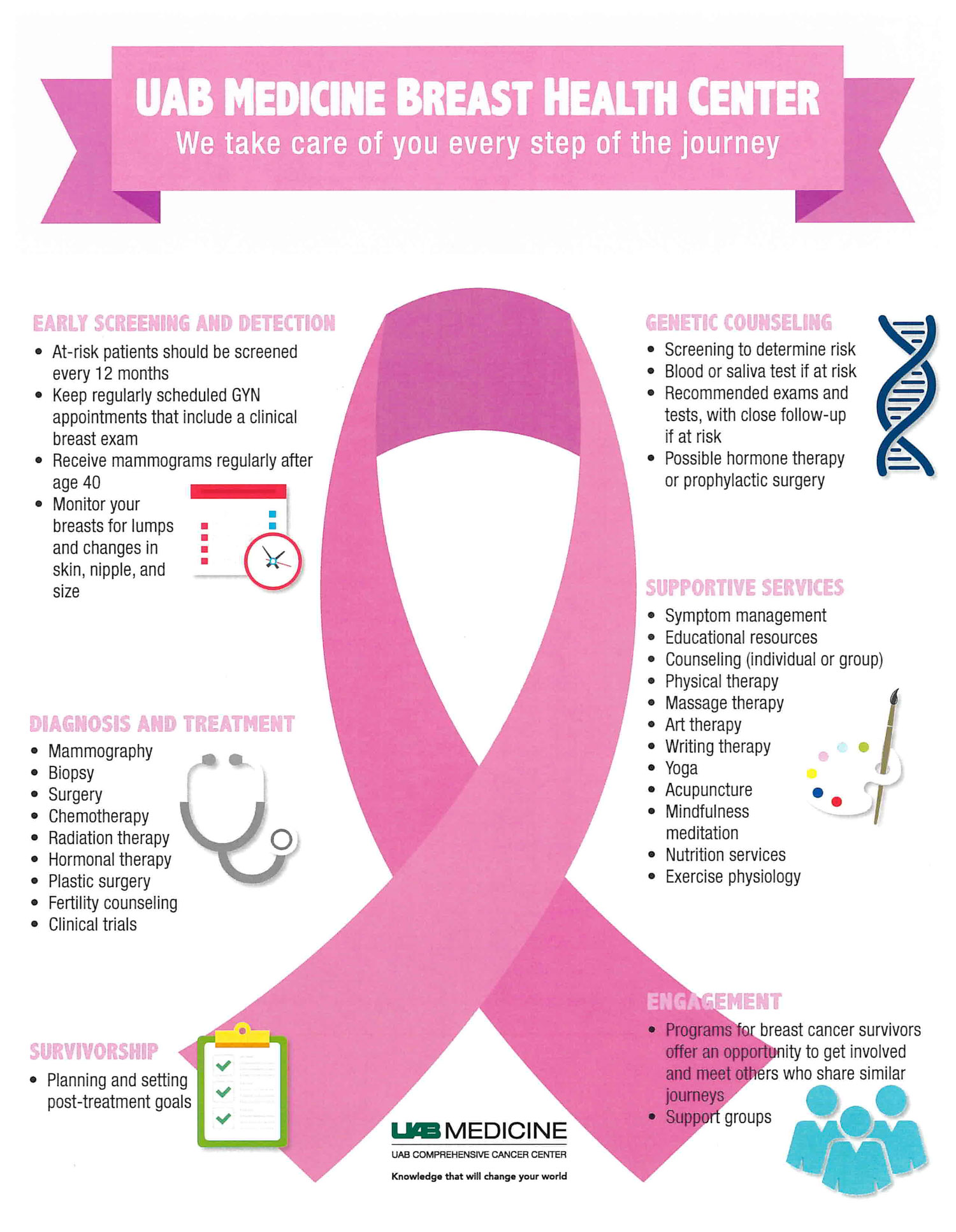
- Breast screening is a safe and helpful way to detect breast cancer early, especially in women aged 50 to 74.
- Treatment for breast cancer depends on which stage the cancer is at, and may include surgery, radiotherapy or chemotherapy.
- With prompt detection and treatment, 9 in 10 women with breast cancer survive at least 5 years, and many live much longer.
What is breast cancer?
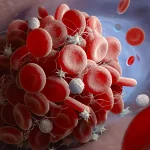
Breast cancer is a disease where cells in the breast grow abnormally and in an uncontrolled way to form a lump, known as a tumour. If left untreated, lumps may spread from breast tissue to other parts of the body, such as the bones, liver or lungs. Breast cancer affects both men and women, although it is less common in men.
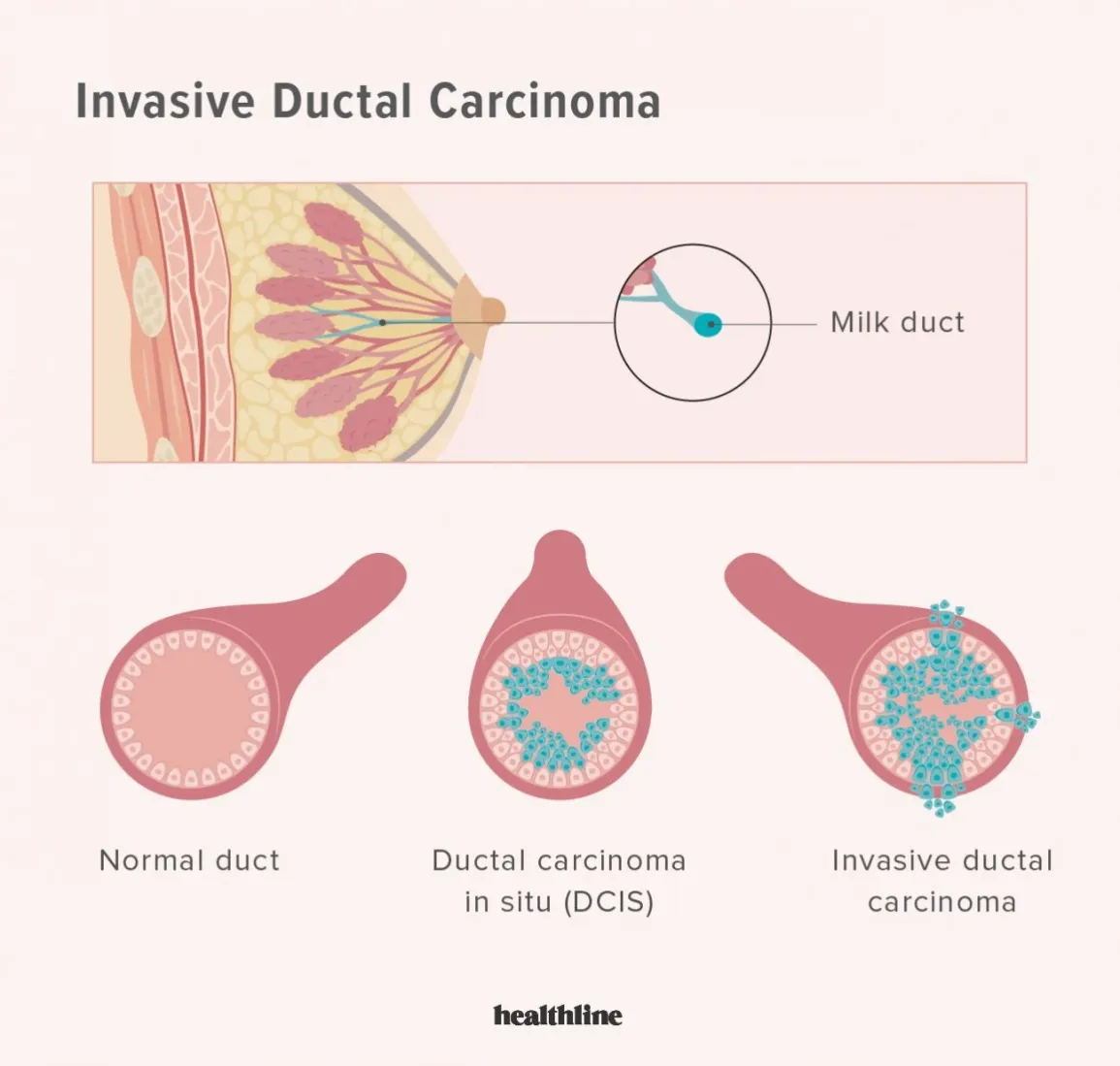
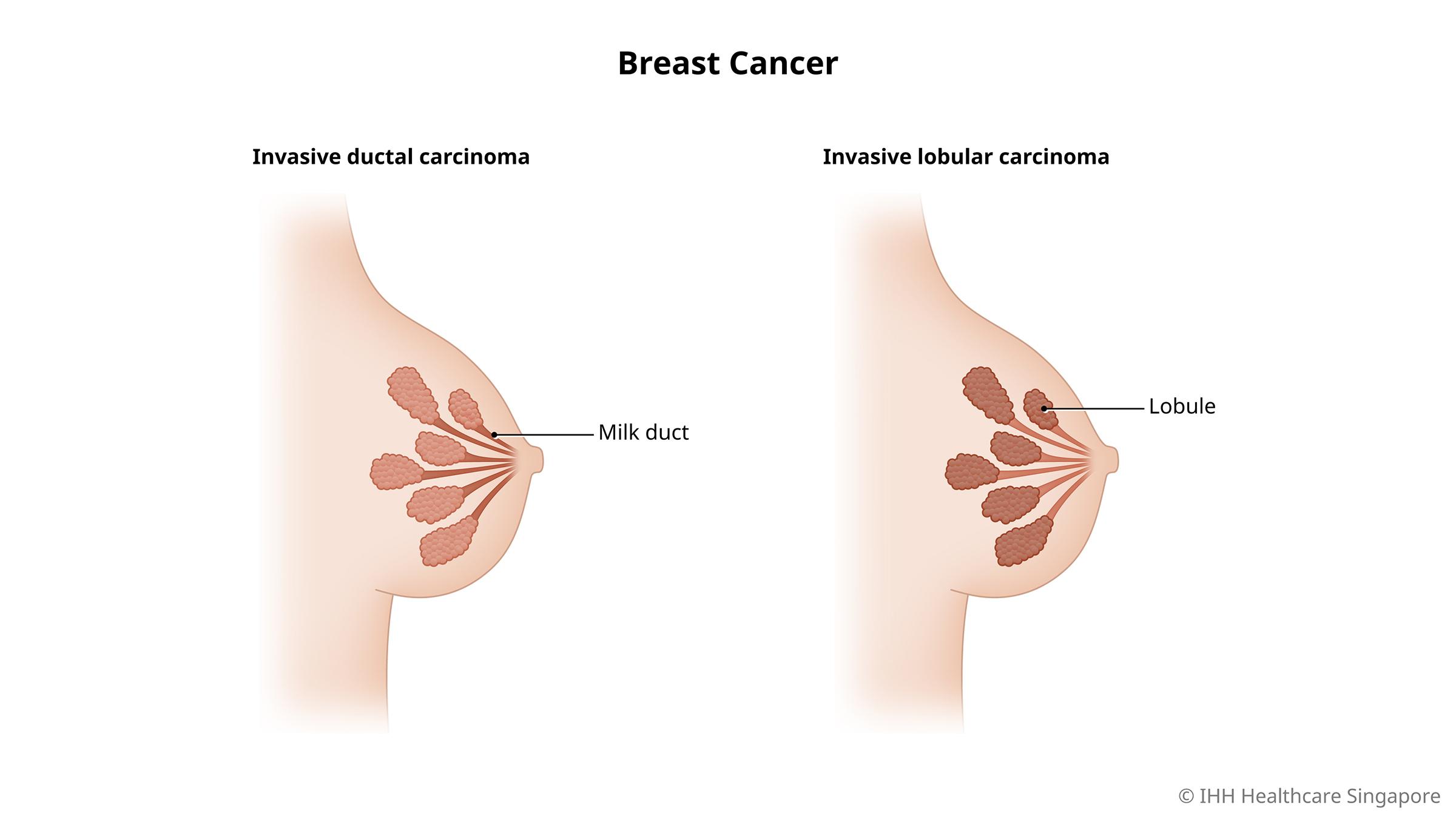
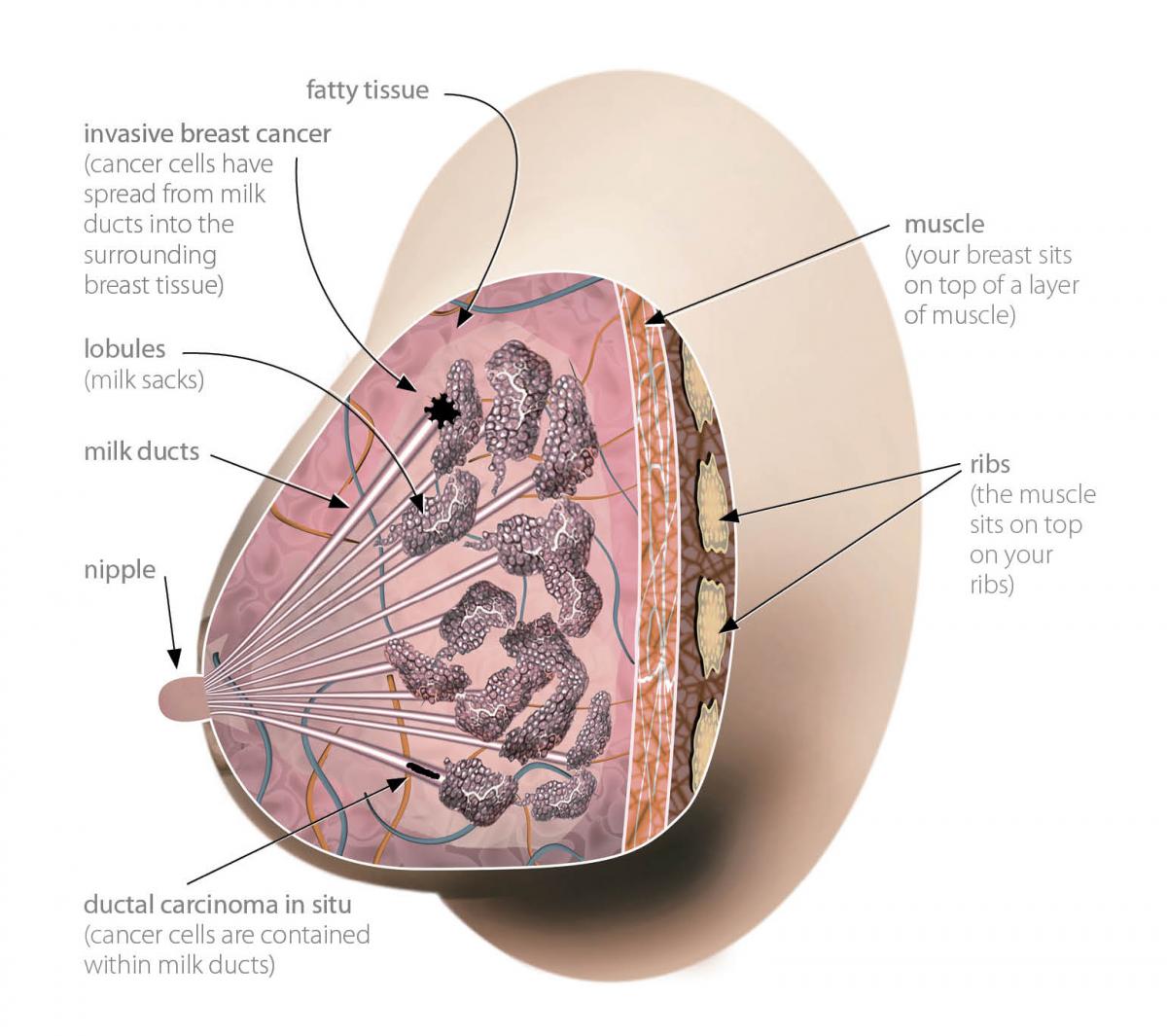
Some breast cancers, known as ‘pre-invasive’ or ‘carcinoma in situ’ breast cancers, appear inside the milk ducts or milk-producing lobules of the breast. Other ‘invasive’ breast cancers grow within normal breast tissue and may spread to elsewhere in the body. There are various types, including Paget’s disease, inflammatory breast cancer, ductal carcinoma, lobular carcinoma, hormone receptor positive breast cancer, HER-2 positive breast cancer and triple negative breast cancer (which tests negative for oestrogen, progesterone and HER-2).
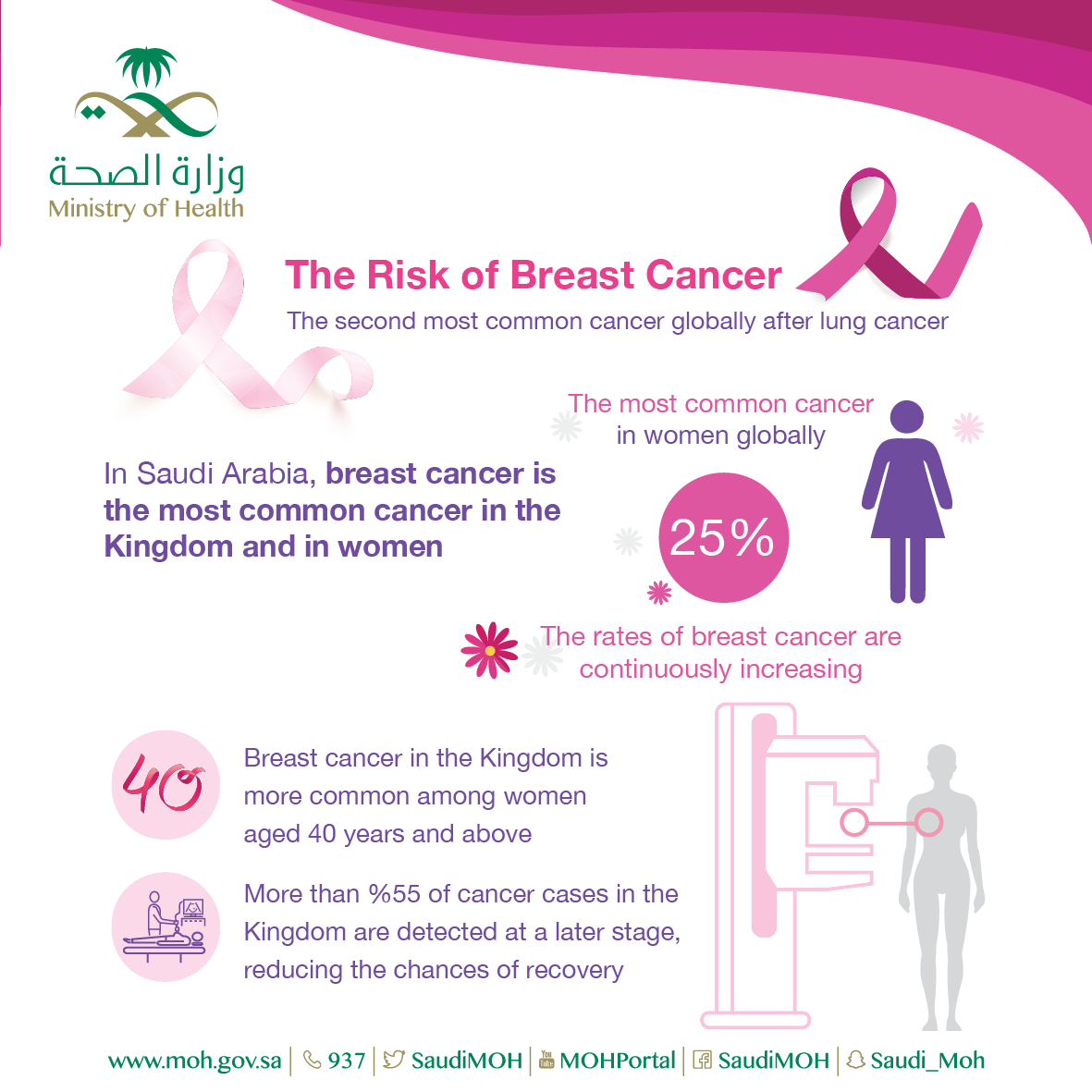
Breast cancer is the most commonly-diagnosed cancer in women, and it’s estimated that 8 Australians die from the disease each day. Thankfully, with prompt detection and treatment, 9 in 10 women with breast cancer survive at least 5 years, and many live much longer.
What are the symptoms of breast cancer?
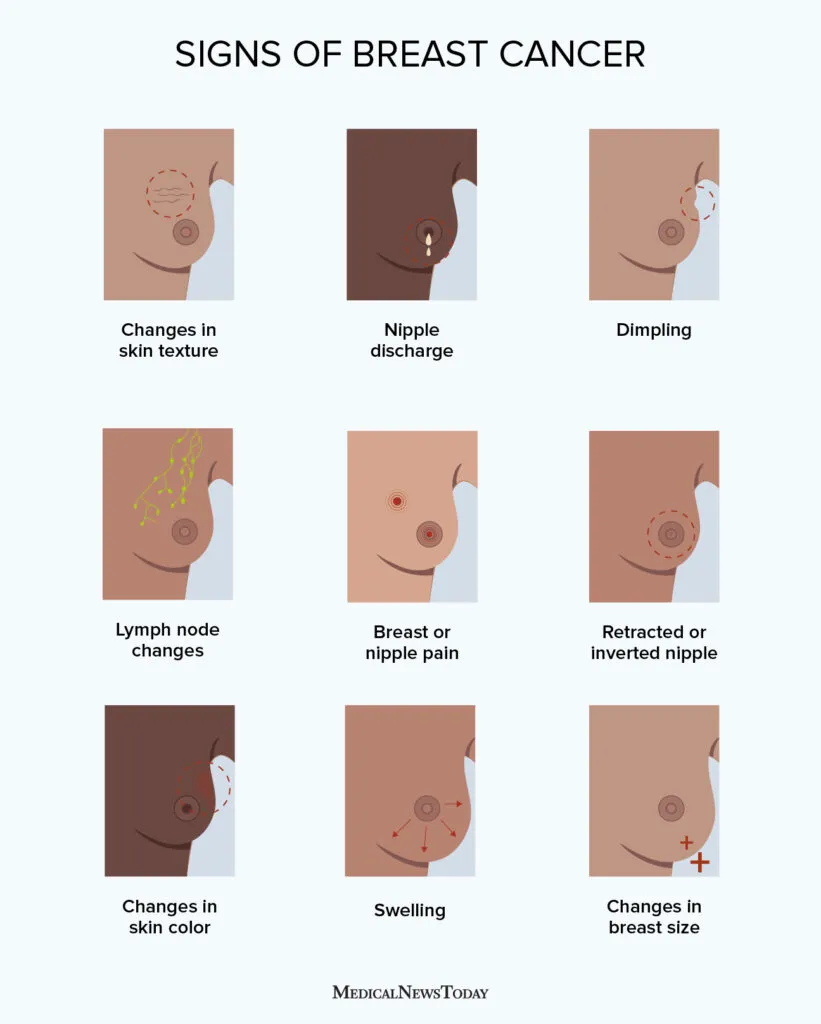
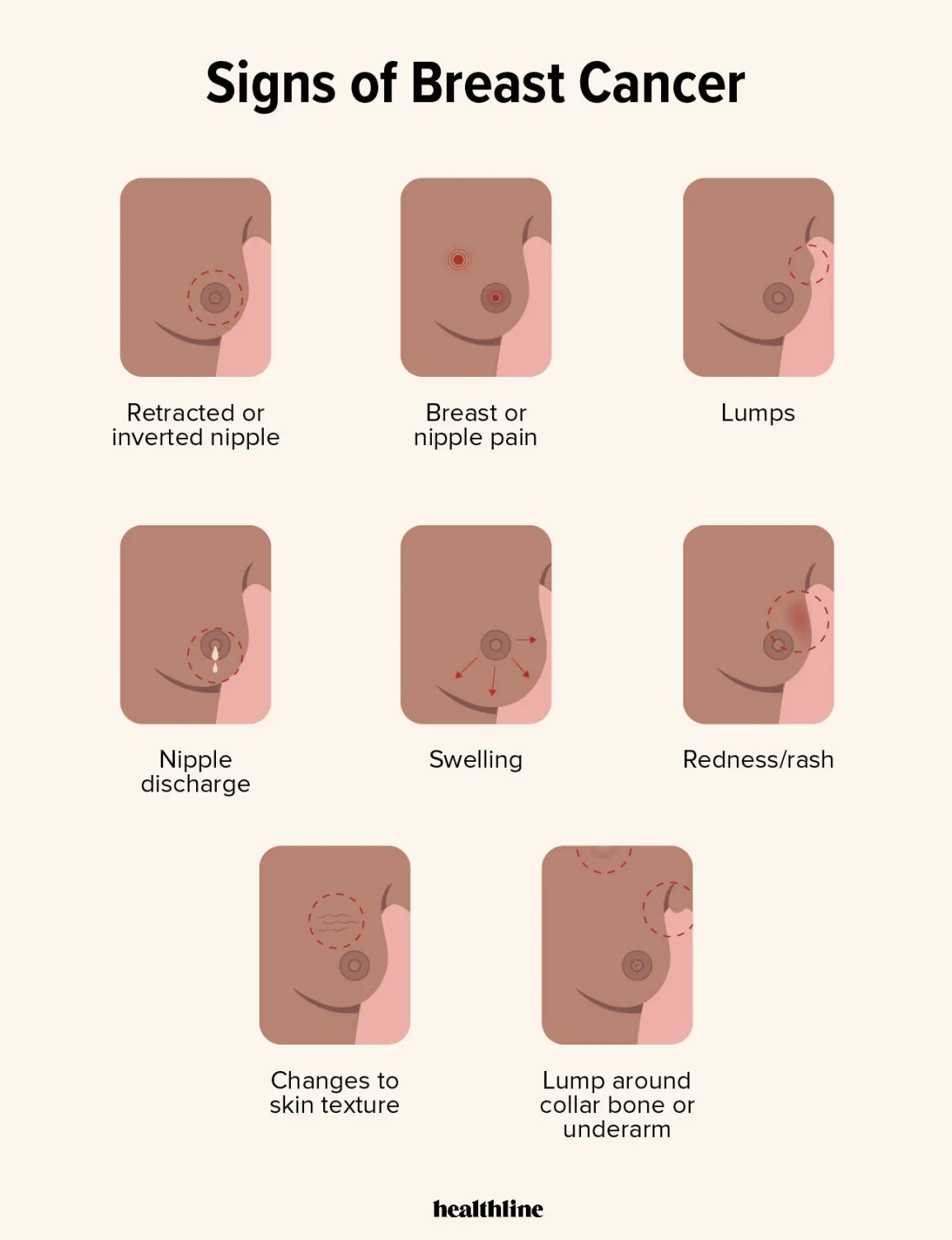
Symptoms of breast cancer can include:
- a lump or area of thickened tissue in the breast (especially if only on one side)
- a change in the size or shape of one or both breasts
- a change in the shape or appearance of the nipple, such as crusting, sores, redness or inversion (where the nipple turns in instead of pointing out)
- changes to the skin of the breasts, such as dimpling (looking like an orange peel), rash, or redness
- discomfort or swelling in either armpit
Symptoms of breast cancer in men are similar to those that women experience.
What causes breast cancer?
While there is no specific cause for breast cancer, some lifestyle factors are associated with a higher risk of developing the condition:
- Drinking alcohol may raise oestrogen levels in the body and is associated with a 30 to 50% increased risk of breast cancer.
- Unhealthy weight — Being obese is associated with a 20 to 40% increased risk of breast cancer in post-menopausal women.
- Smoking, particularly if you started as a teenager, increases your breast cancer risk.
Other factors that can’t be changed also impact your likelihood of getting breast cancer:
- Your age — The older you get, the more likely it is your cells become damaged and progress to cancer. Nearly 4 in 5 new breast cancers are diagnosed in women over 50 years.
- Your family history — Women with a first-degree relative with breast cancer are twice as likely to get it themselves than women without one.
- Having BRCA1, BRCA2 or other gene mutations — Up to 1 in 10 breast cancers are due to a strong family history of these genetic mutations.
- Dense breasts — Women with more dense tissue in their breasts (visible only using an X-ray or mammogram) may have a higher risk of breast cancer.
- Previous radiation exposure — Women who were exposed to radiation therapy in the chest region (for example, for childhood cancers) may have 5 times the risk of breast cancer as women who were not.
What’s your risk?
Click here to learn about iPrevent — a breast cancer risk assessment tool to help you start a discussion with your GP about your risk.
When should I see my doctor?
See your doctor or healthcare professional if you notice symptoms of possible breast cancer, such as a lump, pain, itch, nipple discharge or dimpling, or if you have any concerns about your breast cancer risk.
Can I be screened for breast cancer?
BreastScreen Australia offers a free screening program for women at risk of breast cancer:
- If you’re aged between 50 and 74 years, you’ll be invited to access a free mammograms every 2 years. This is because nearly 4 in 5 breast cancers occur in women aged over 50.
- If you’re aged between 40 and 49 years or over 75 years, you are also eligible but won’t be contacted about it.
- Women under 40 years of age are usually not offered breast screening because the density of their breast tissue makes it harder to detect cancers on mammograms.
Younger women with a strong family history of breast or ovarian cancer, or women with breast cancer diagnosed in the last 5 years may also benefit from breast screening. For more details, call BreastScreen Australia on 13 20 50 or visit their website.
How is breast cancer diagnosed?
Tests to find breast cancer
To find the cause of a breast change, your doctor will typically use an approach called the ‘triple test’, which includes:
- a medical history and clinical breast examination
- imaging tests, such as a diagnostic mammogram or ultrasound
- a biopsy, which involves taking a sample of tissue cells from the breast and testing them for signs of cancer.
Most women don’t show any abnormal results in these tests.
Staging and further tests
If breast cancer is confirmed, you will be referred for further tests, such as a CT scan, blood tests, bone scans or a PET scan, to see what stage your cancer is at.
Your healthcare team may use a 4 stage system:
- Stage 0 (in situ) refers to pre-invasive breast cancer that’s only in the milk ducts or lobules of the breast.
- Stage I to IIB (early) refer to early breast cancer of a small size (5cm or less).
- Stage IIB to Stage IIIC cancers (advanced, localised) have spread to nearby lymph nodes in the breastbone or armpit.
- Stage IV cancer (advanced, metastatic) have spread to other parts of the body.
There may also be further tests for hormone receptors (to see if your cancer cells have receptors for estrogen or progesterone), HER-2 (a protein that promotes cancer cell growth) or other genetic markers. These tests help decide the best treatment for your type of breast cancer.
How is breast cancer treated?
Depending on the features of the breast cancer, there are several treatment options.
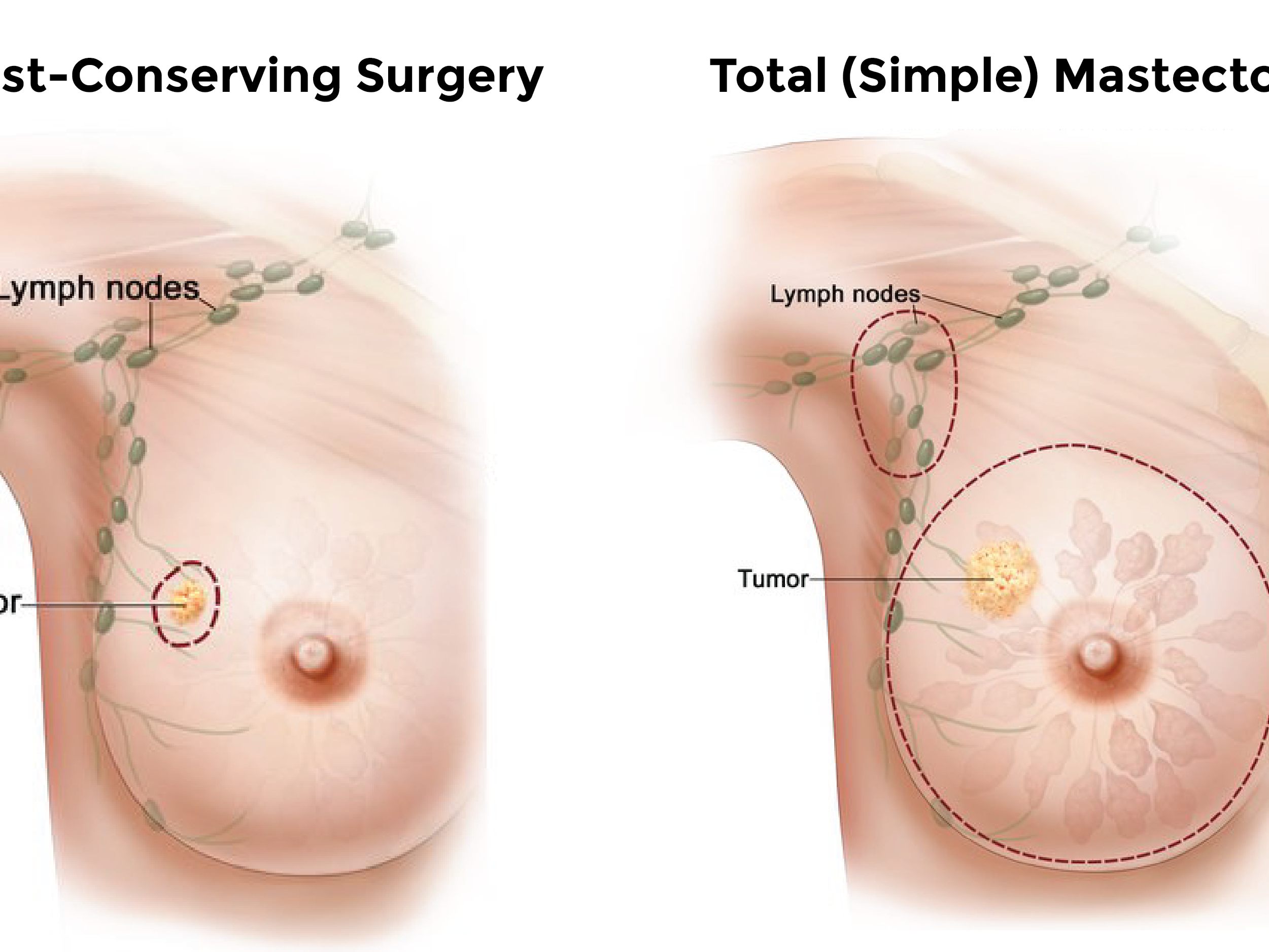
Surgery
This treatment involves removing localised cancer from the breast. A lumpectomy (“breast conserving surgery”) involves removing the cancer and some healthy tissue but keeping the breast intact. A mastectomy involves removing the whole breast affected by cancer. During breast surgery, lymph nodes under the arm may also be removed.
Radiation therapy
Radiotherapy is often used to destroy any breast cancer cells left following a lumpectomy or lymph node removal. It is sometimes used after a mastectomy if there is a risk of cancer recurring in the chest area.
Chemotherapy
Chemotherapy involves using anti-cancer drugs to kill the remaining cancer cells in the body. It may be used before or after surgery or radiation therapy, or together with radiation therapy.
Hormone therapy
Hormone therapy involves drugs that reduce your body’s oestrogen and progesterone levels, to stop or slow hormone receptor positive cancer cells.
Palliative care
In some cases, the medical team will talk to a patient about palliative care. Palliative care aims to improve your quality of life by alleviating symptoms of cancer.
Who provides breast cancer treatment?
A medical team may involve several different health professionals. It may include a GP, a radiologist, an oncologist, a breast care nurse, a surgeon and other allied health professionals such as counsellors and therapists. Having a multi-disciplinary team means a patient can receive the best care possible.
Can breast cancer be prevented?
Unfortunately, there isn’t a way to prevent breast cancer completely. However, lifestyle choices such as maintaining a healthy weight and lowering alcohol consumption can help to reduce your risk of breast cancer.
If you are at high risk of developing breast cancer, your doctor may suggest hormone treatments (such as tamoxifen), or a pre-emptive mastectomy.
Are there complications of breast cancer?
Possible complications from breast cancer treatment include:
- Lymphoedema — in some cases, removing your lymph nodes may cause swelling, discomfort and pain in the arm, shoulder and upper body.
- Early menopause — certain treatments, especially chemotherapy and hormone therapy, can cause menopause symptoms, such as hot flushes, joint pain, or a change in sex drive, to occur earlier than usual.
- Anxiety and depression — research shows that anxiety and depression are common among women with breast cancer. One study found that up to 50 per cent of women with early breast cancer may experience anxiety and/or depression in the year after diagnosis.
Living with breast cancer
Breast cancer can be incredibly challenging to deal with and to recover from, so it’s important to give yourself time to come to terms with it if you receive a breast cancer diagnosis and have treatment.