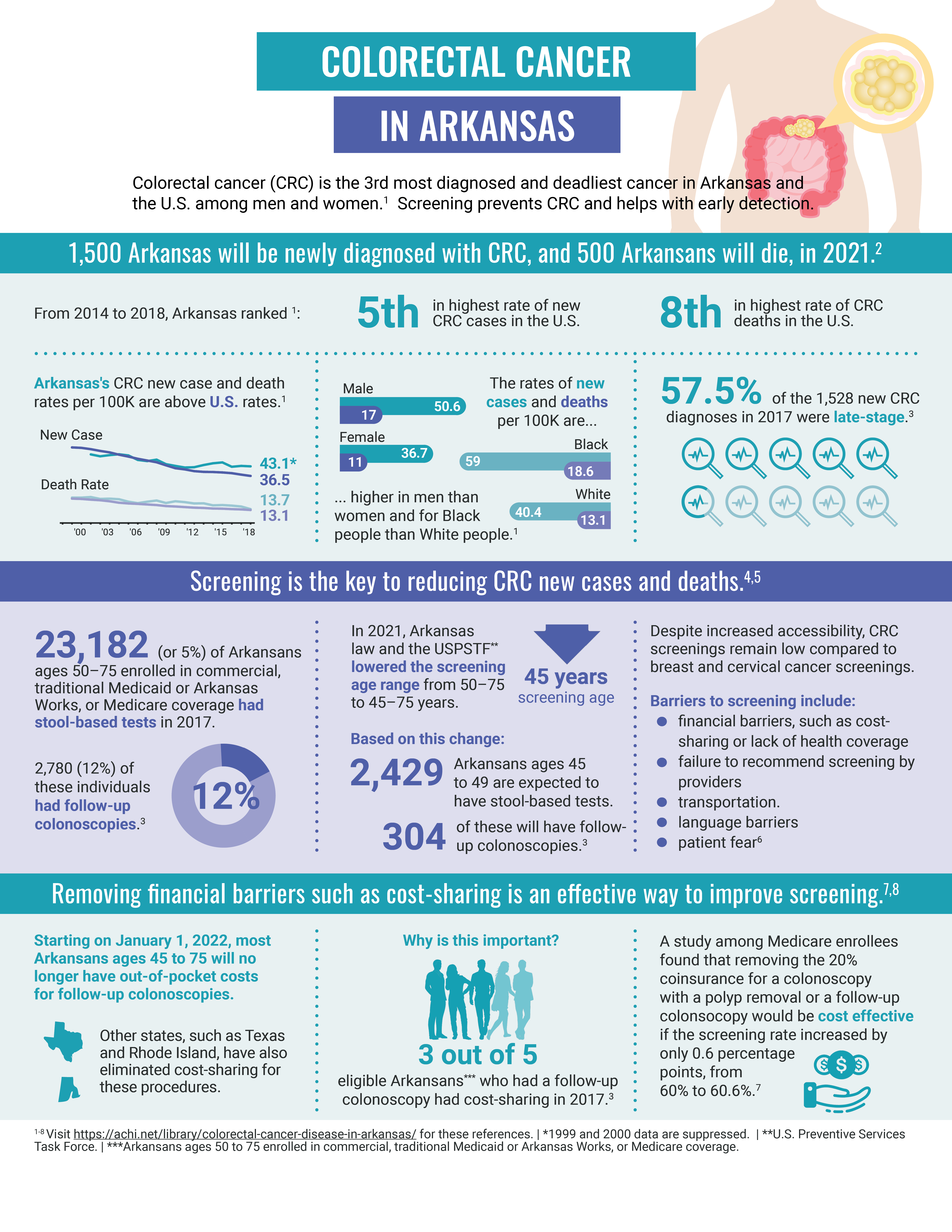
Key facts
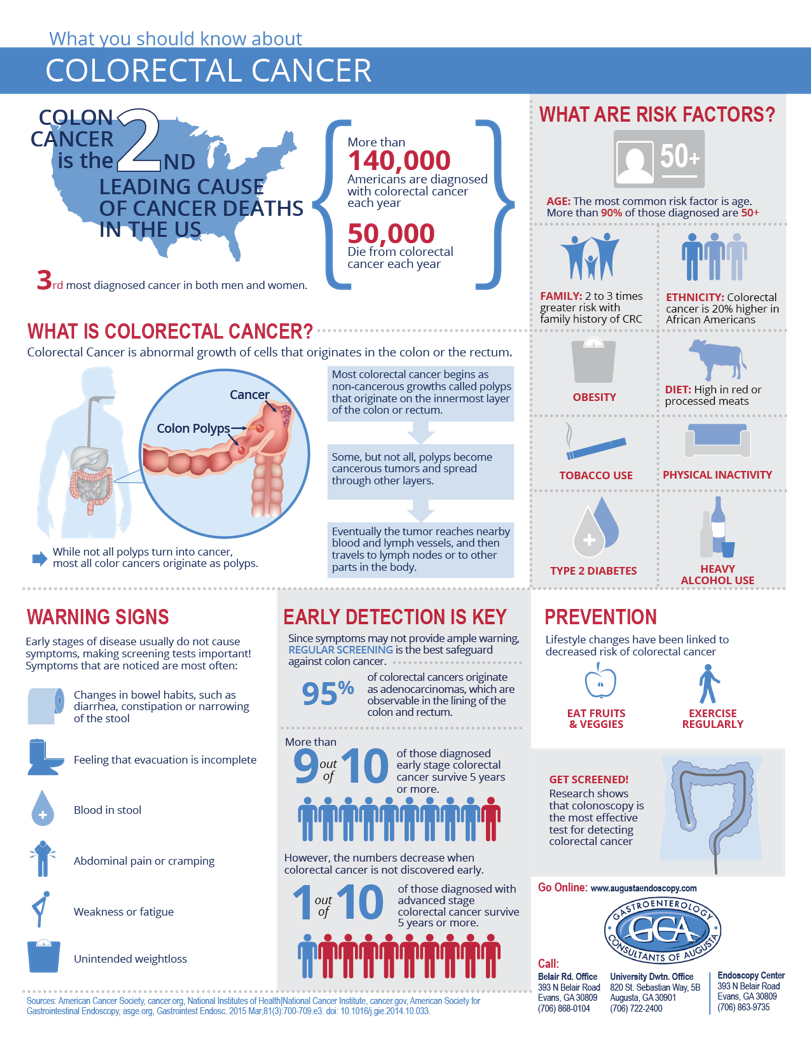
- Bowel (colorectal) cancer occurs when cells in the wall of the large bowel grow abnormally and form a tumour.
- See your doctor if you develop any of the symptoms of bowel cancer, including bleeding from the rectum, bloody stools or changes in bowel habits.
- The treatment for bowel cancer depends on the stage, location and severity of the disease, and may involve surgery, chemotherapy and/or radiotherapy.
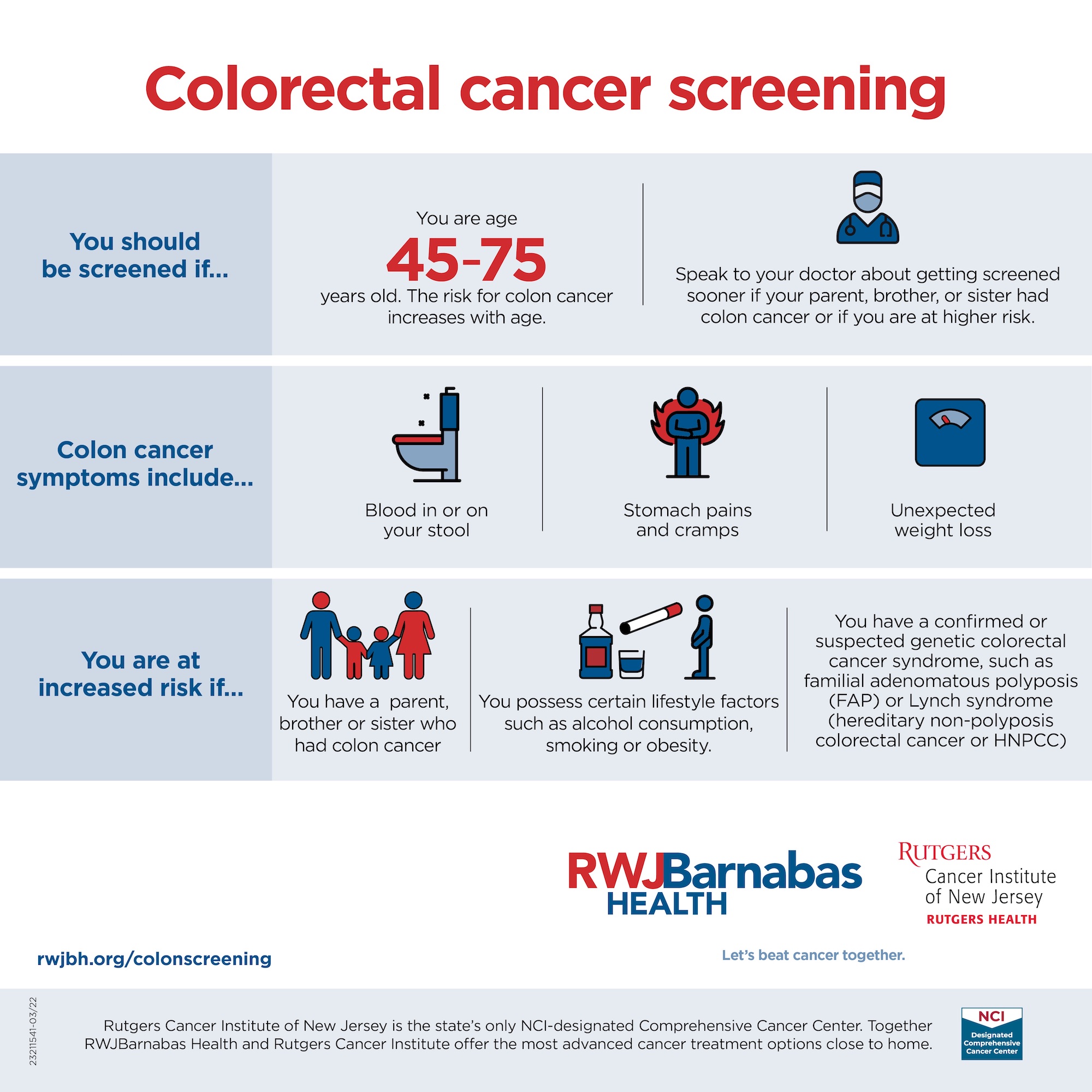
- The National Bowel Cancer Screening Program is free for Australians aged 50 to 74 years and can help detect signs of bowel cancer early on.
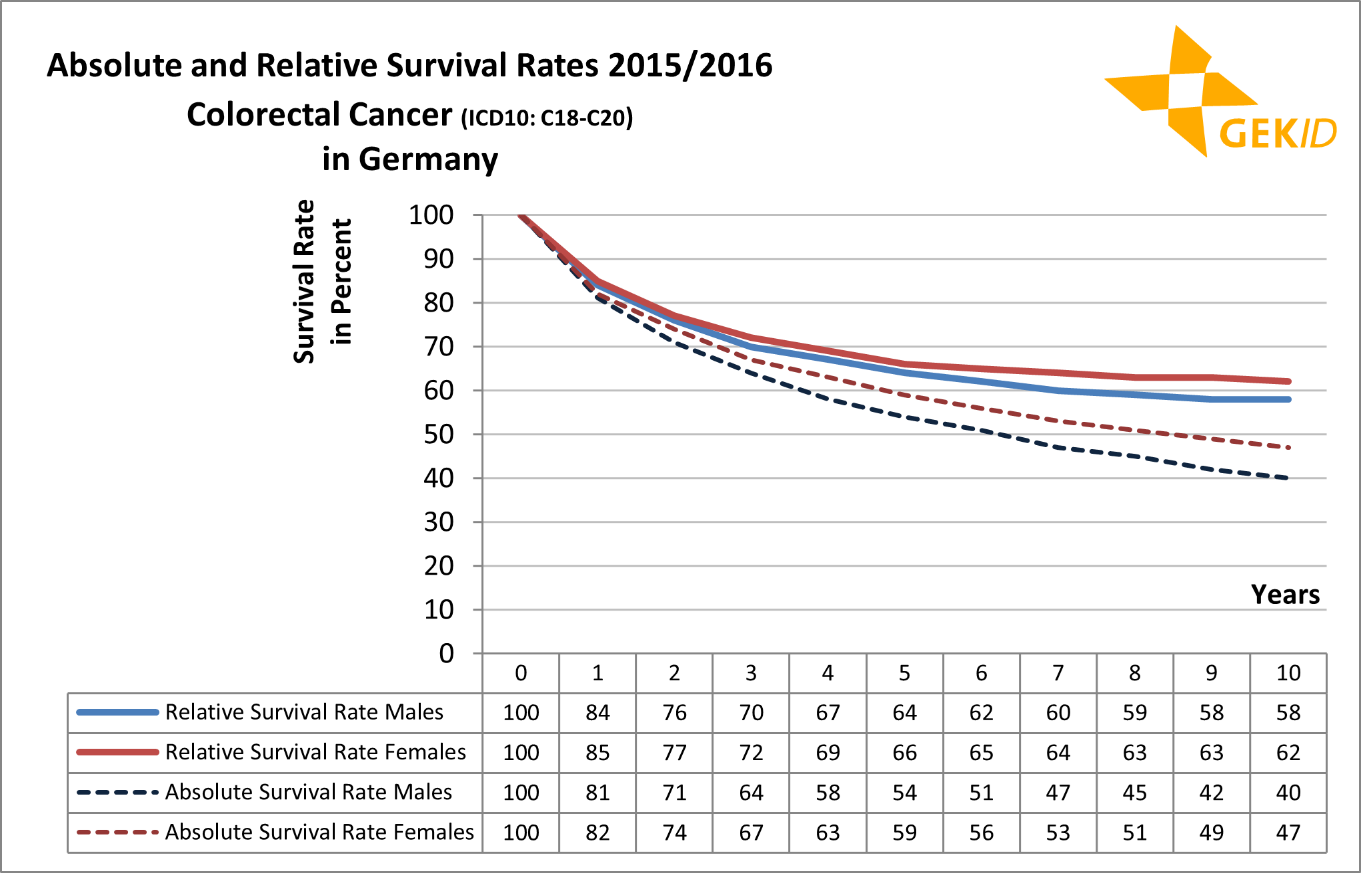
- Late detection is one of the main reasons people die from bowel cancer.
Bowel cancer (colon and rectal cancer)

What is bowel cancer?
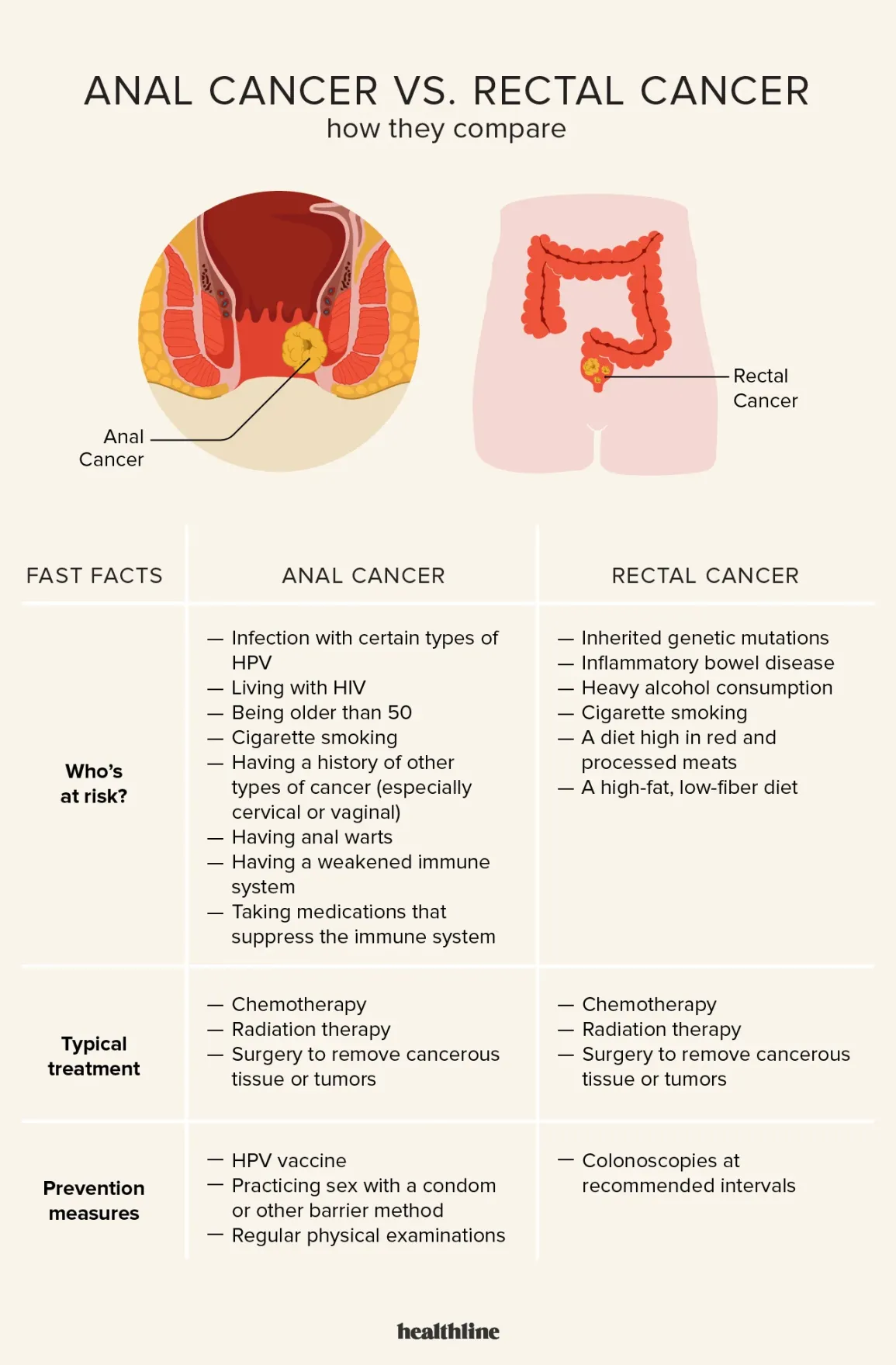
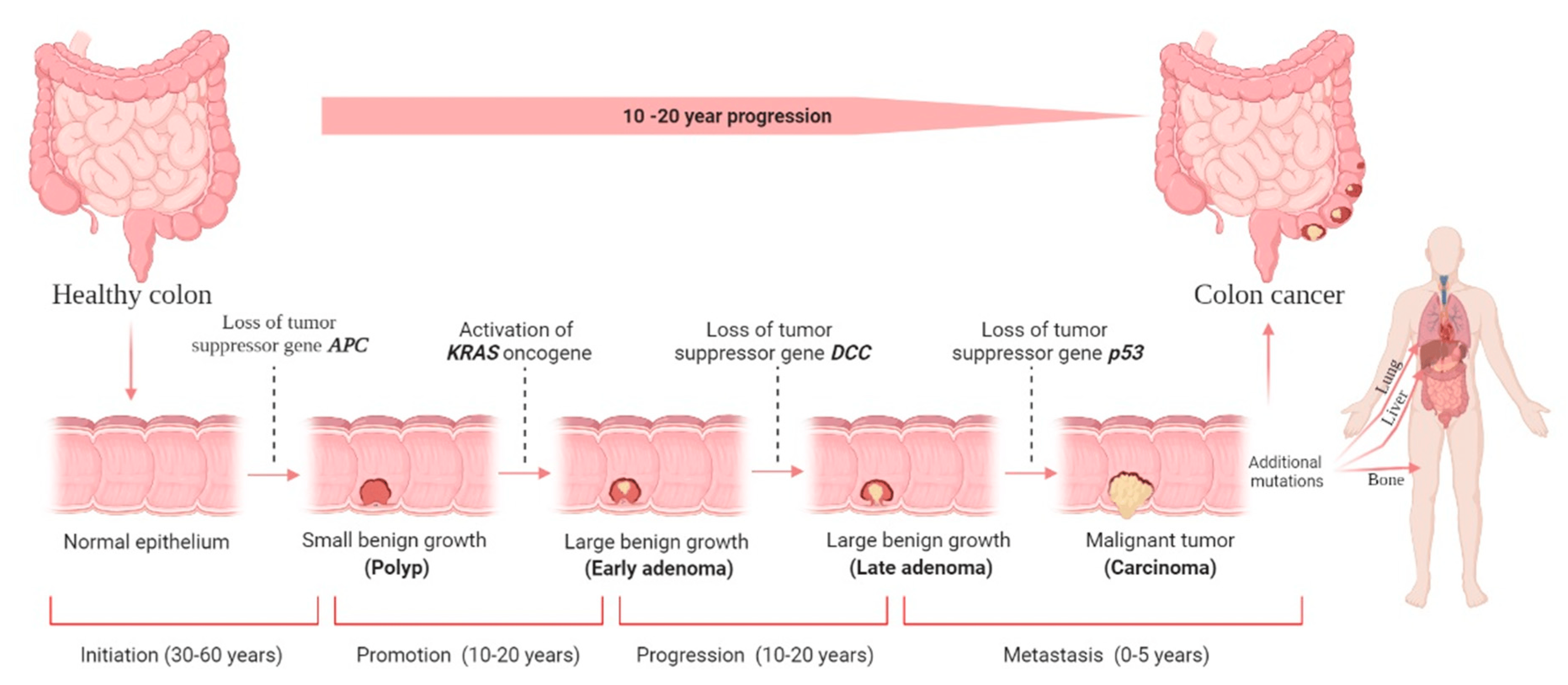
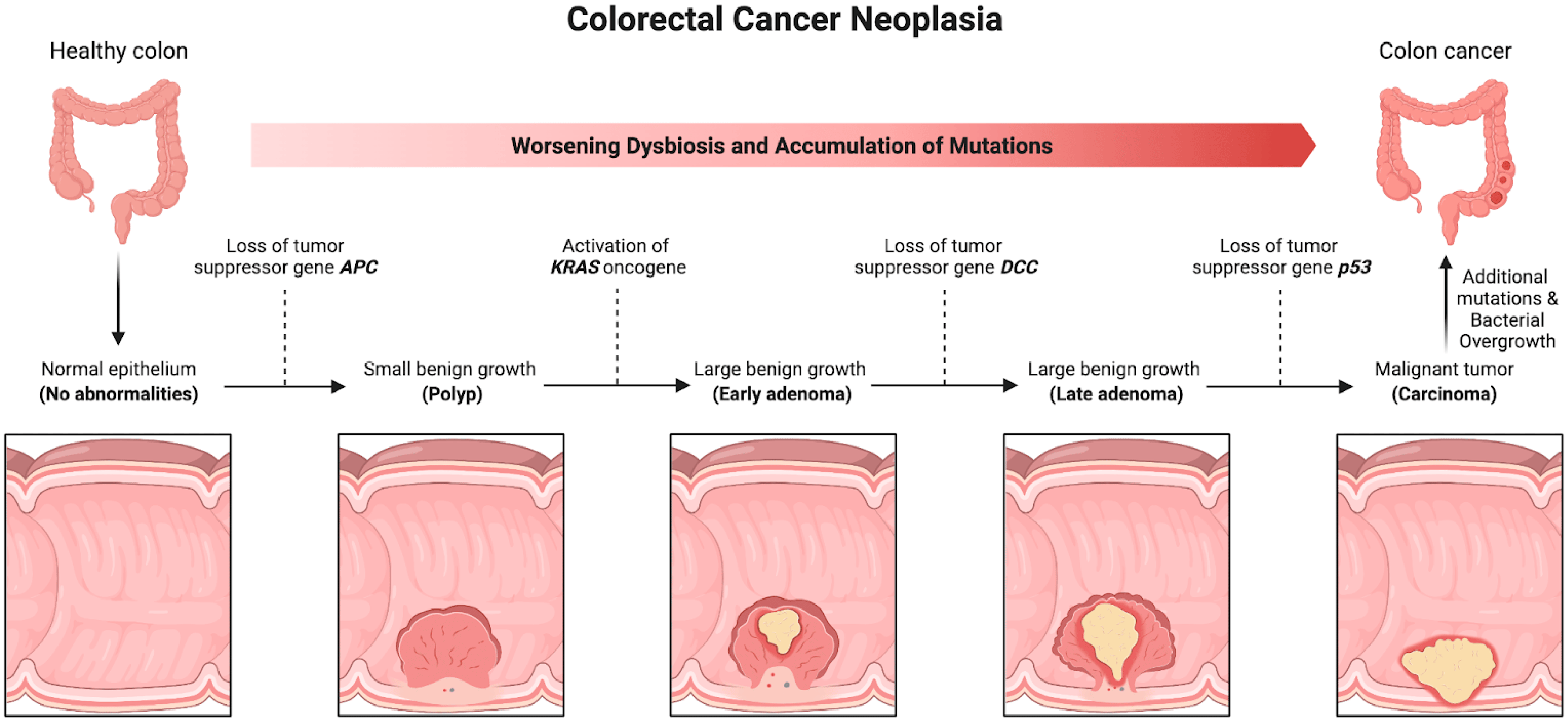
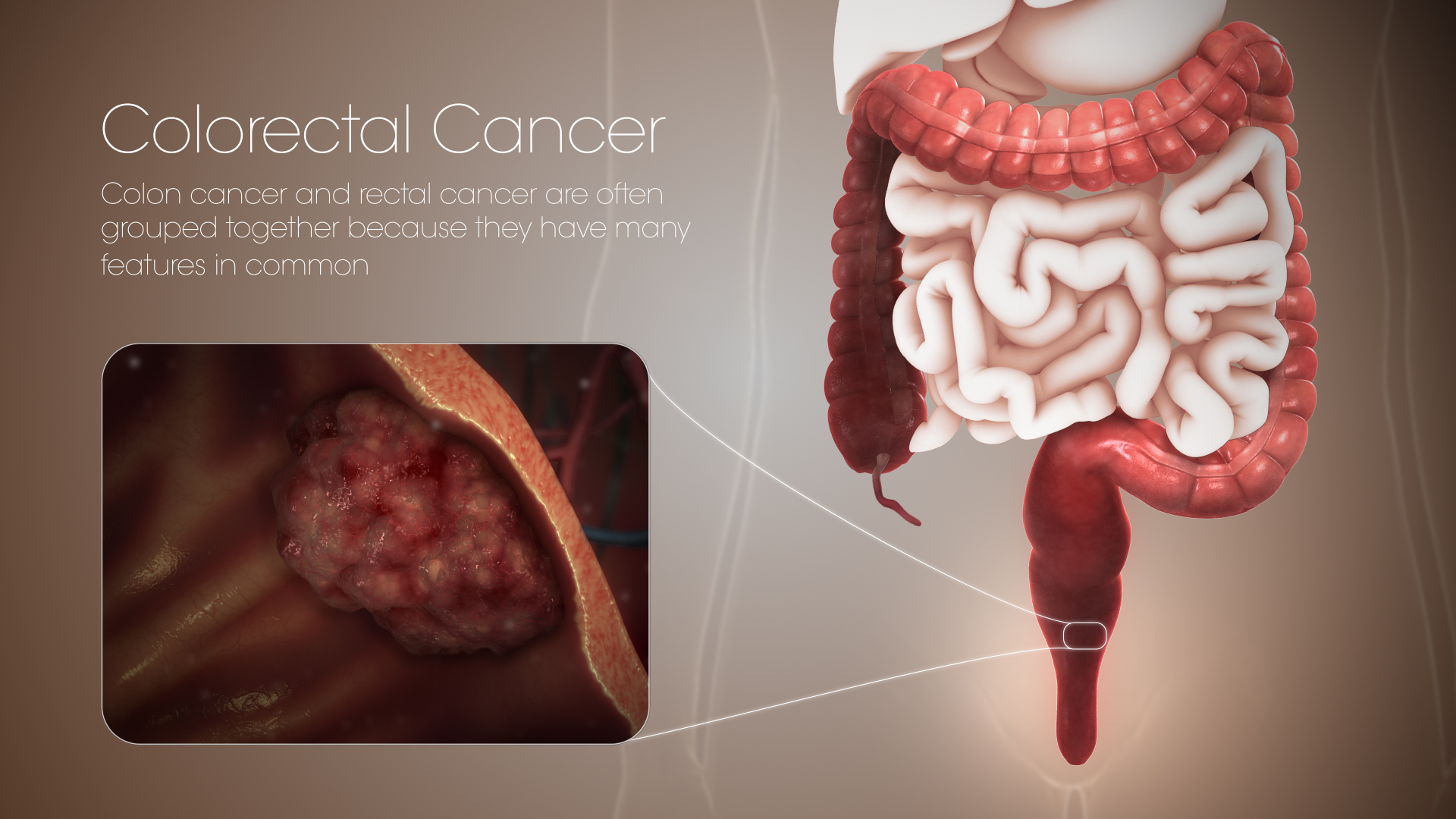
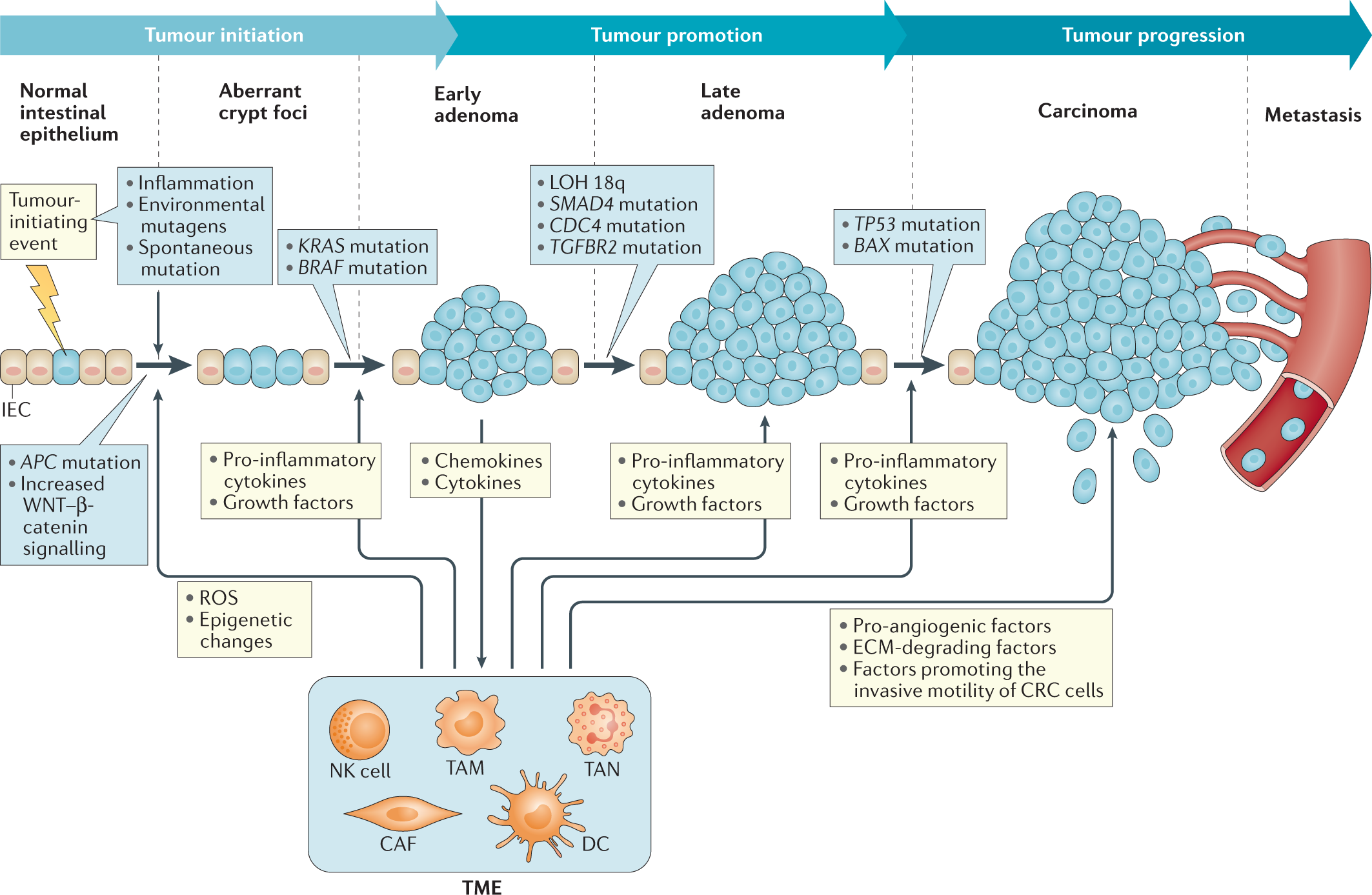
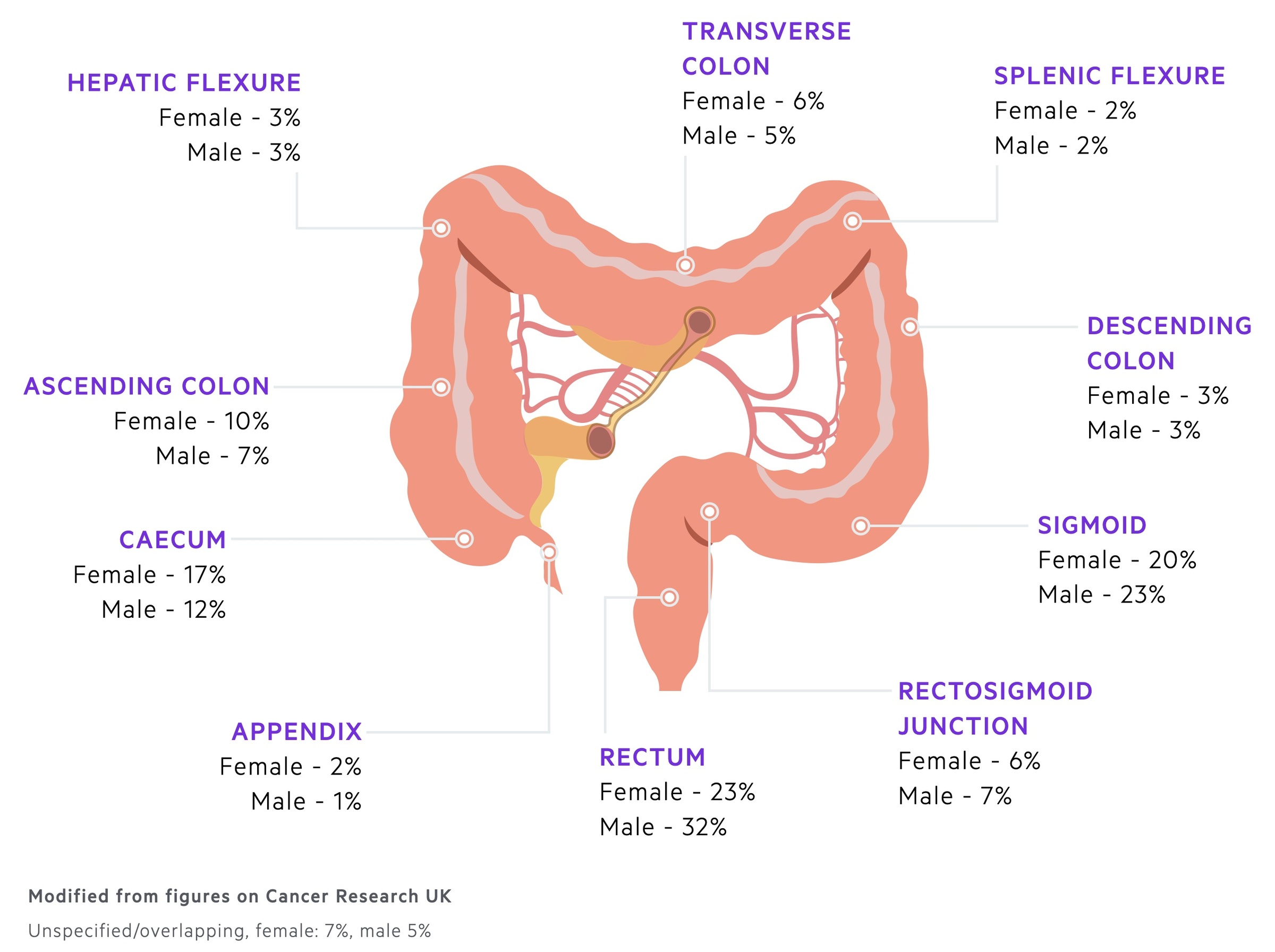
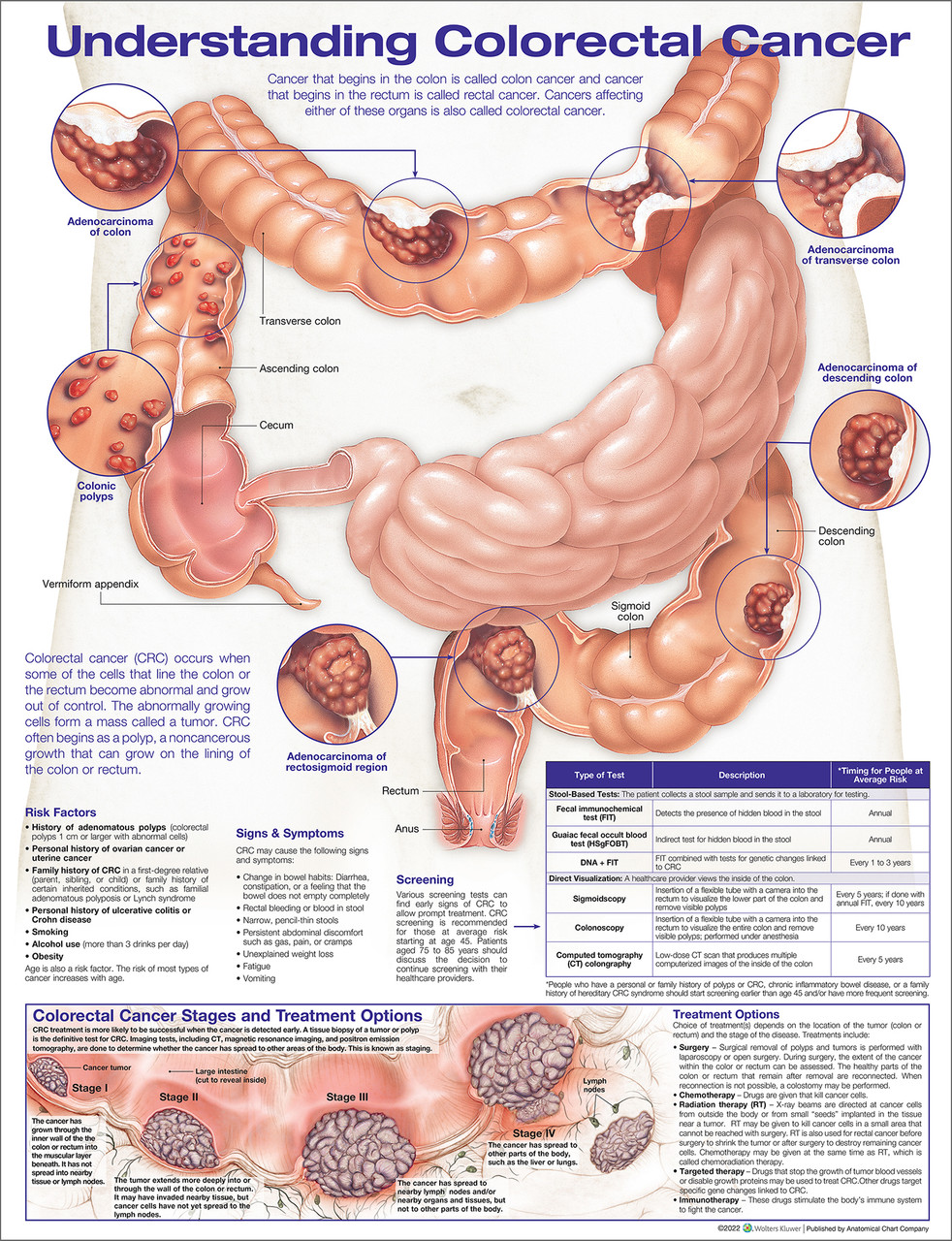
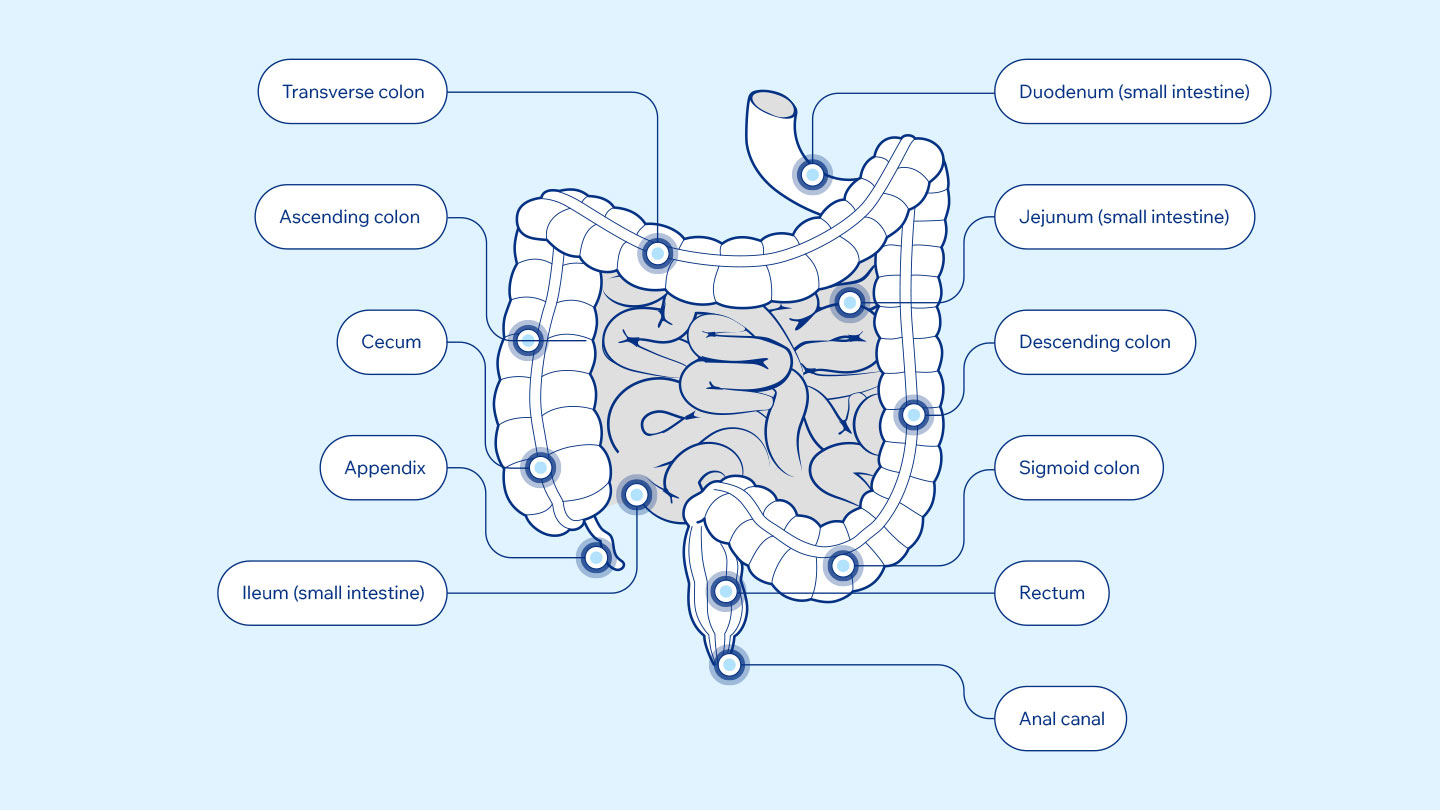
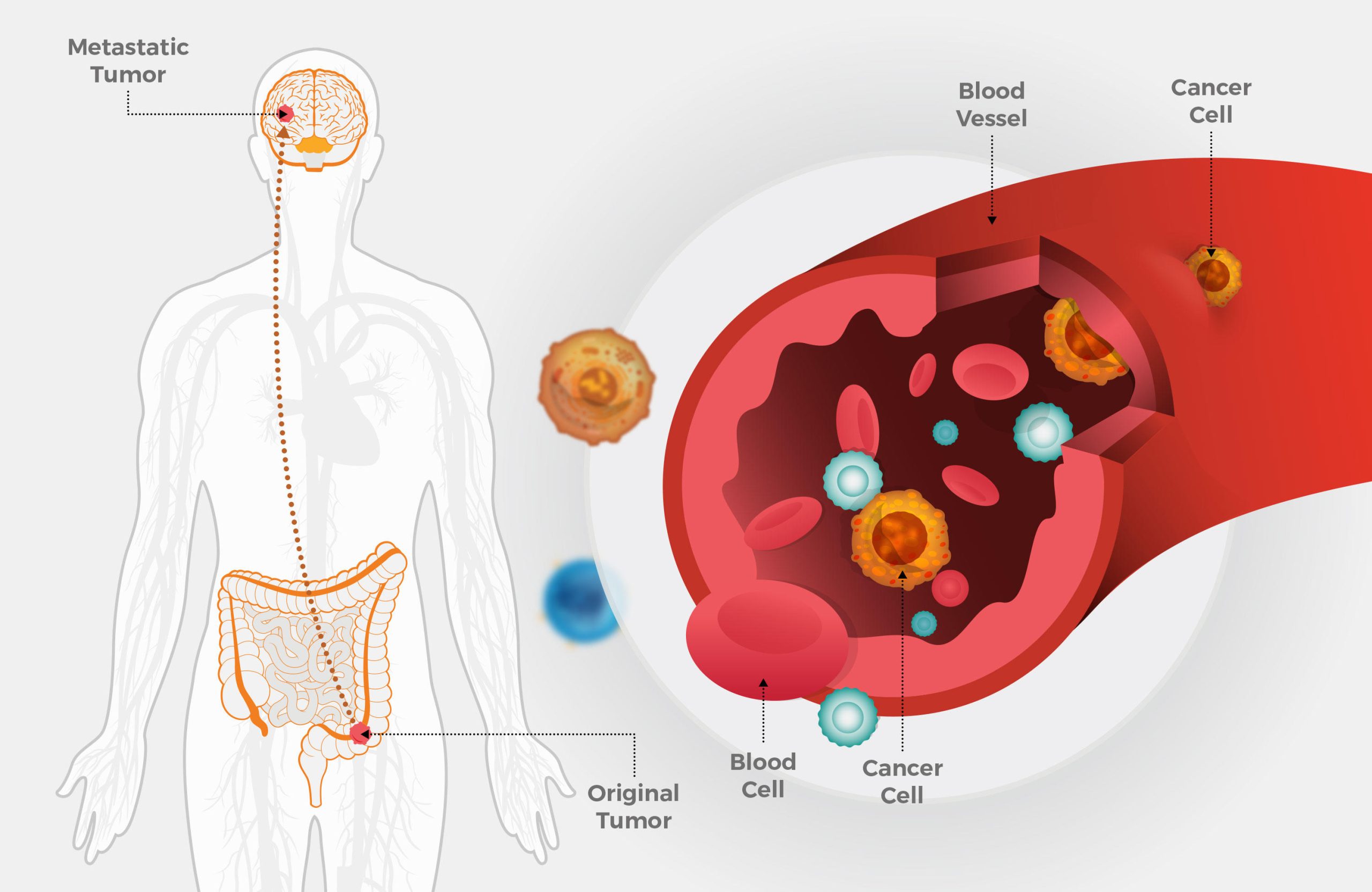
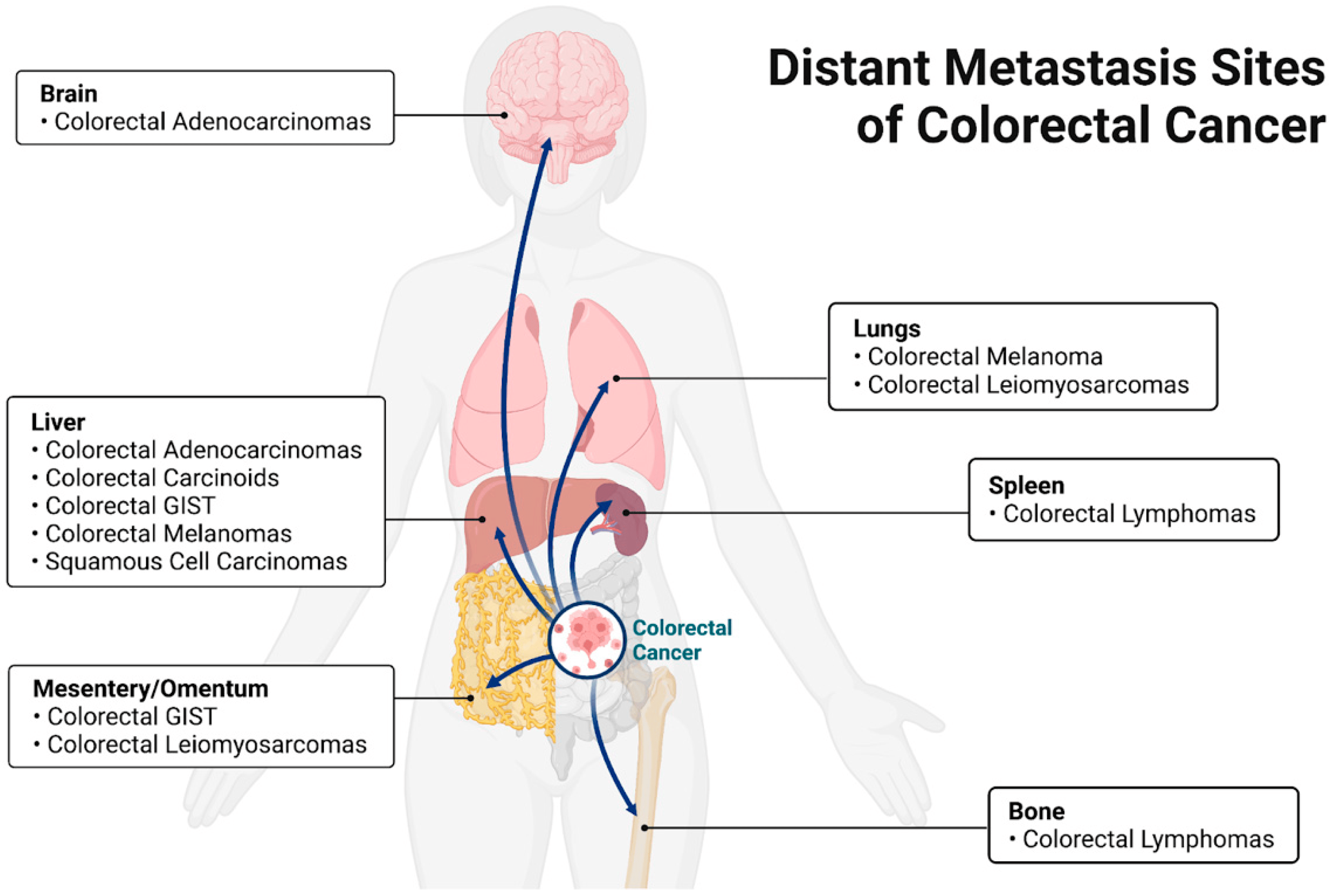
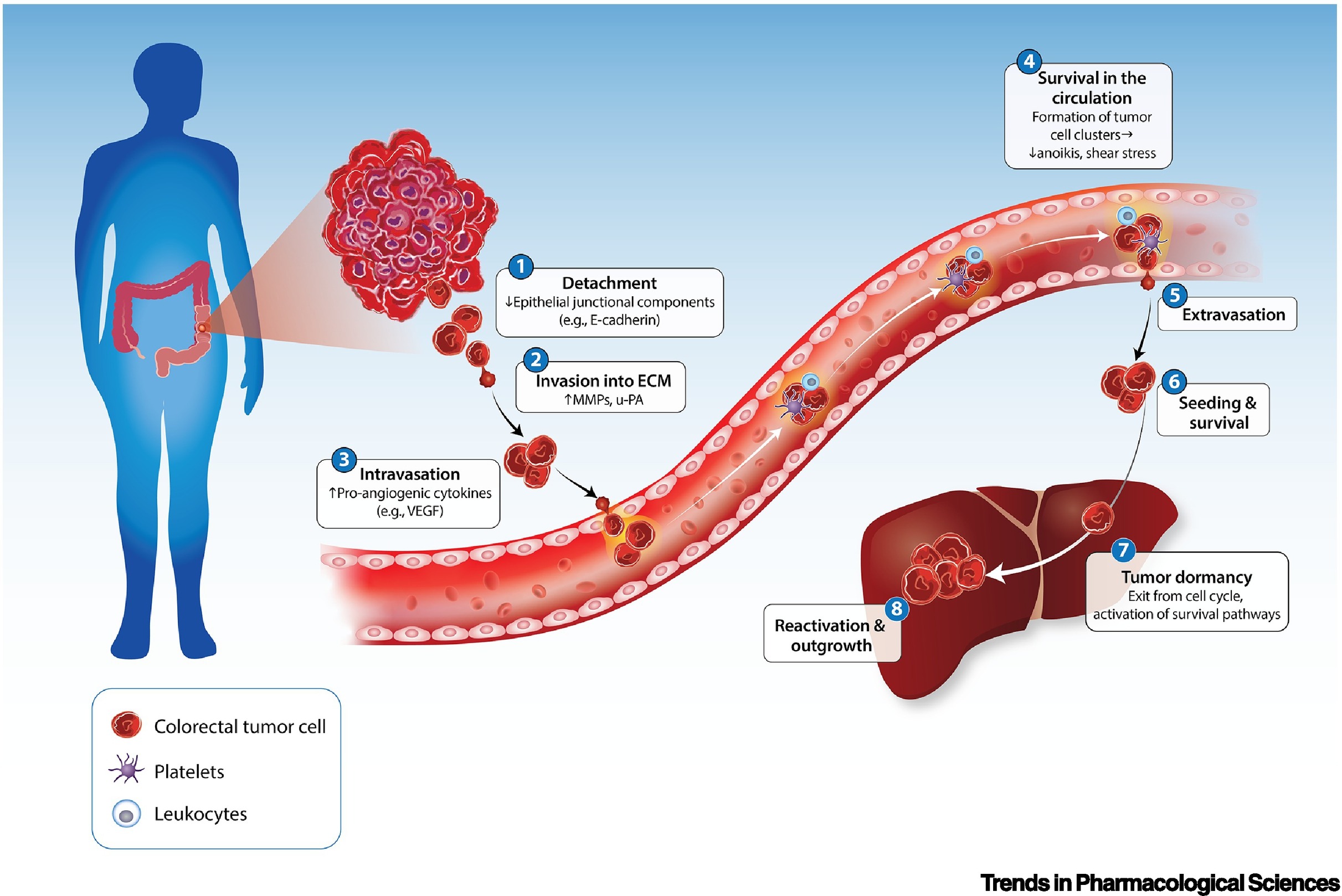
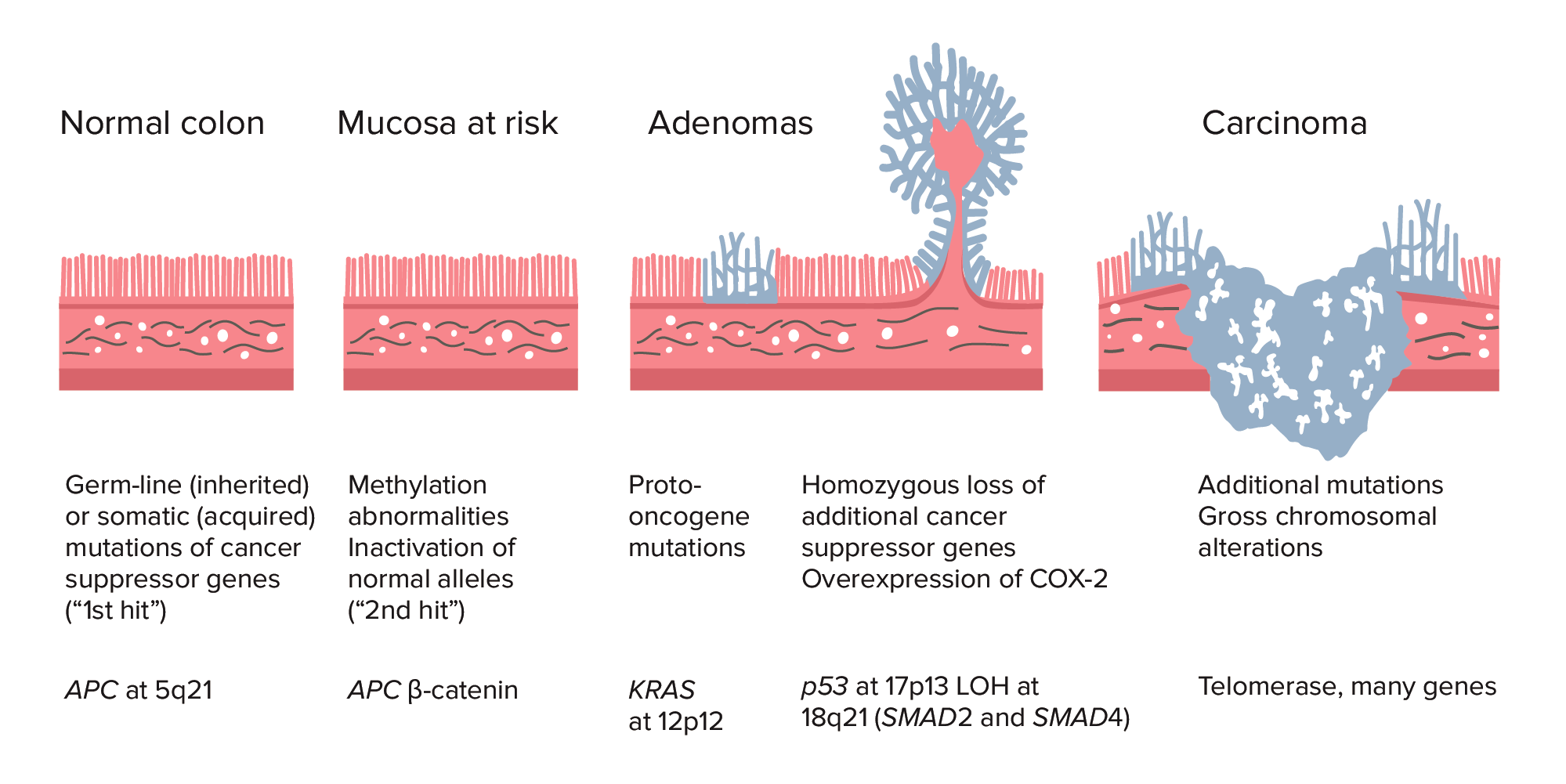
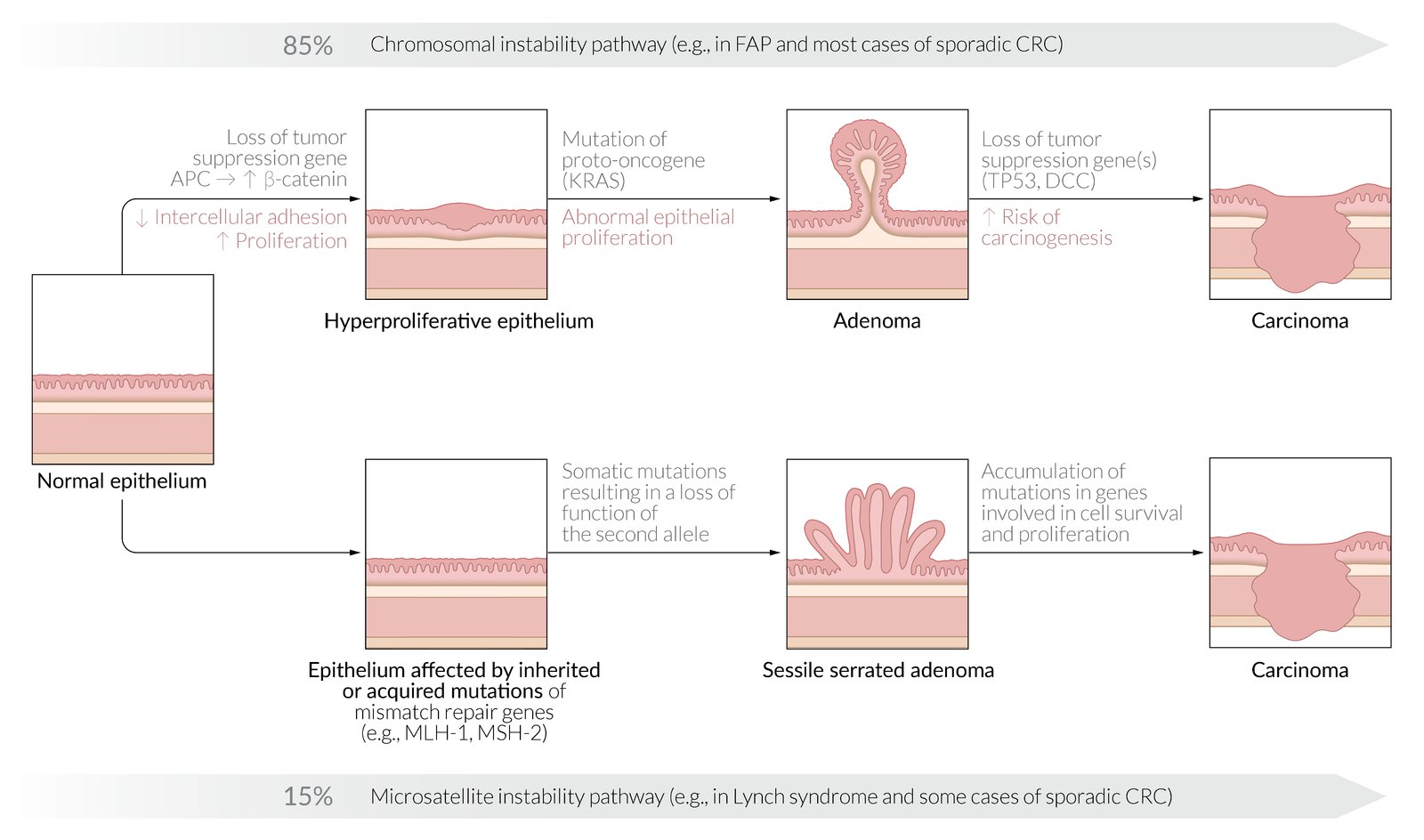
Bowel cancer, also known as colorectal cancer, develops when cells in the wall of the large bowel grow in an abnormal and uncontrolled way. Bowel cancer can occur anywhere along the large bowel, which includes the large intestine, rectum and anal canal. It typically begins growing from the inner lining of the bowel or from small growths on the bowel wall called polyps (adenomas). If left untreated, these cells can spread along the wall of the bowel, to lymph nodes and to elsewhere in the body.
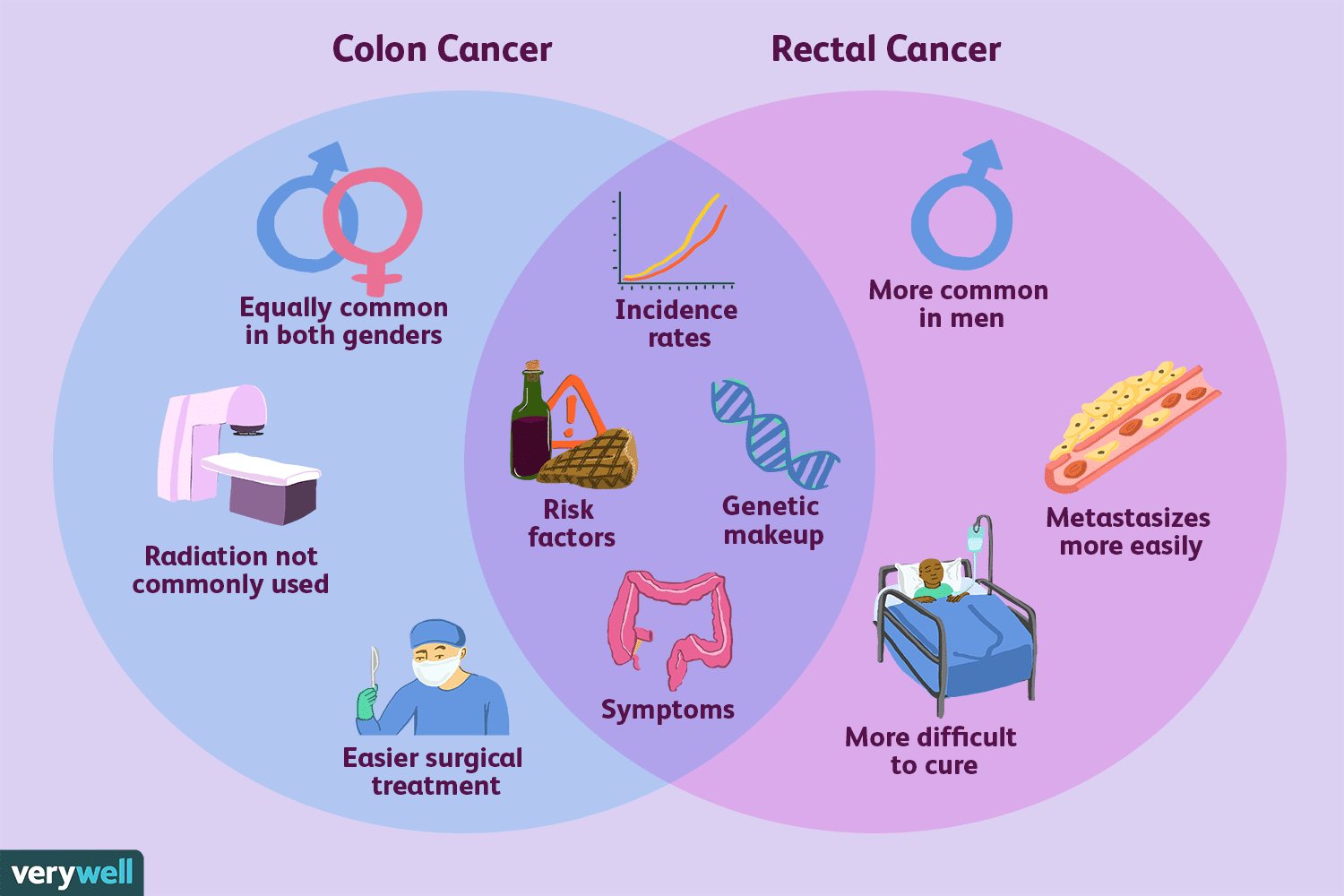
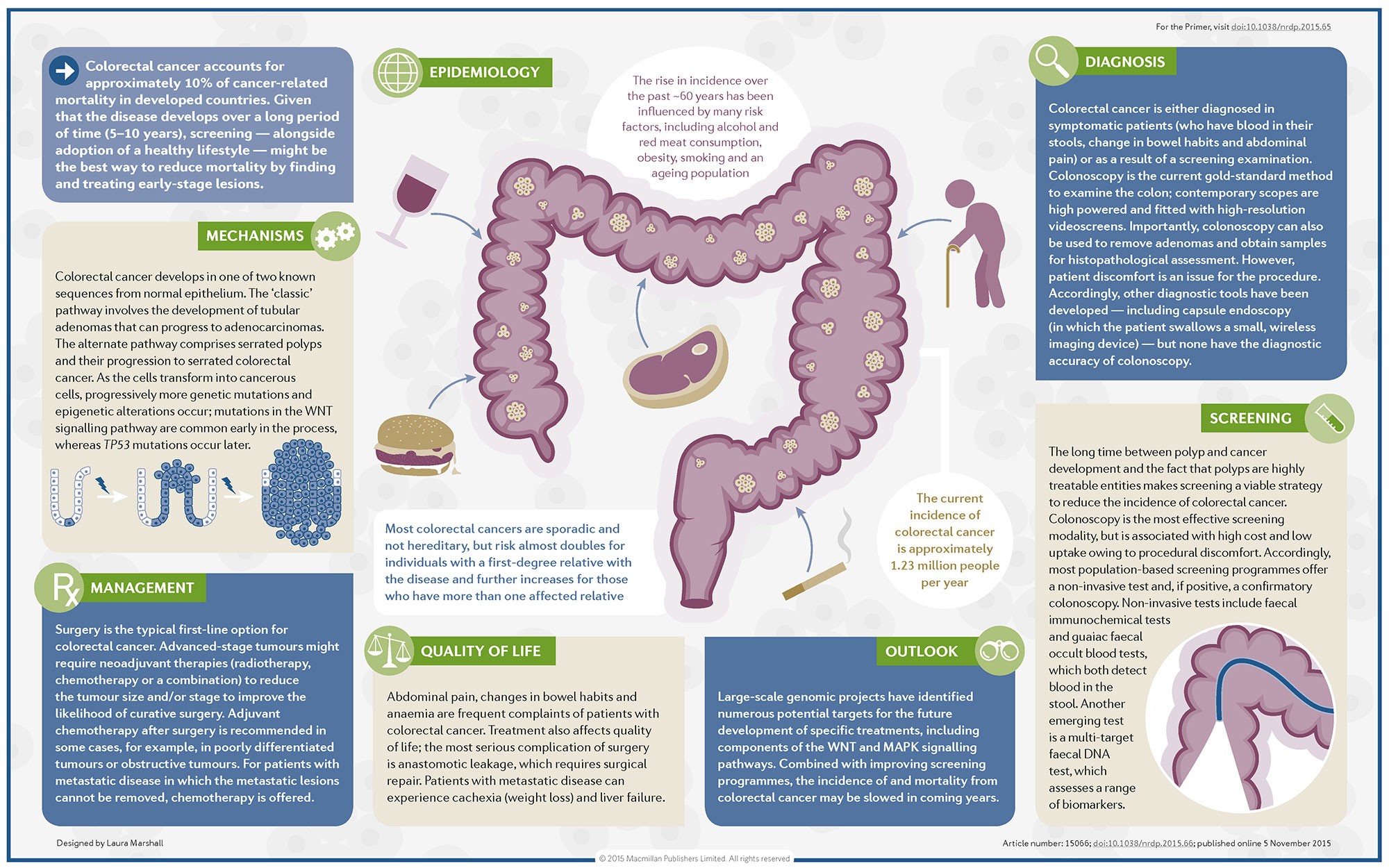
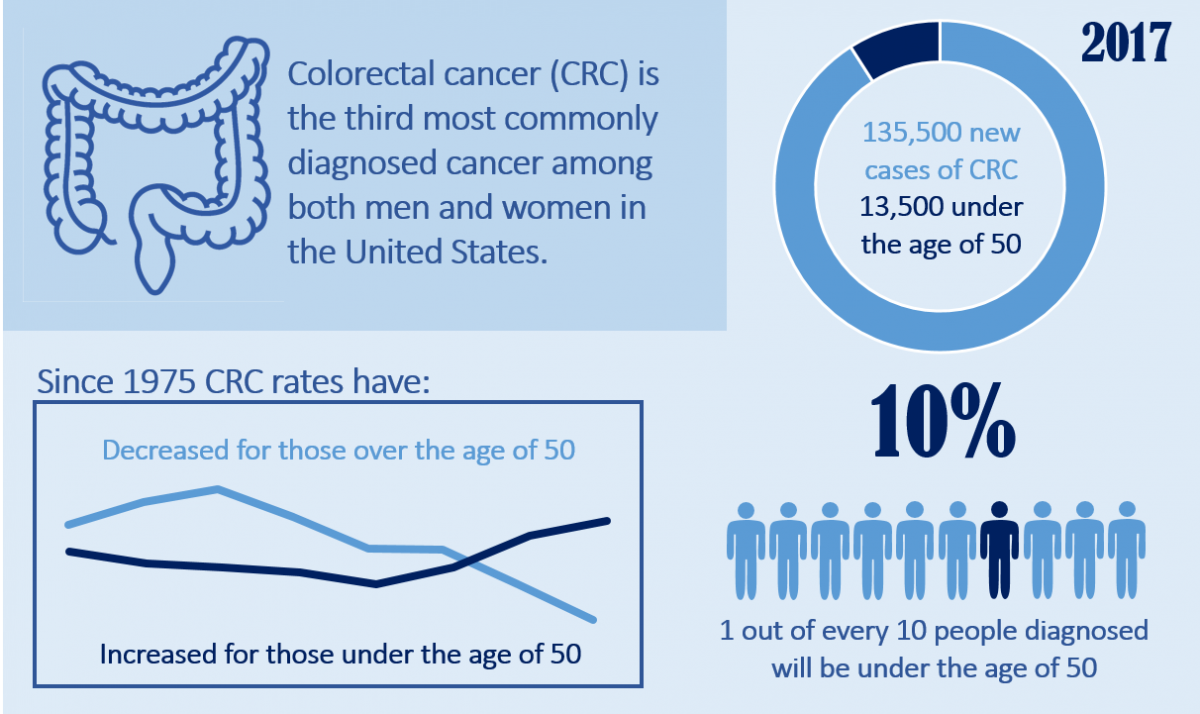
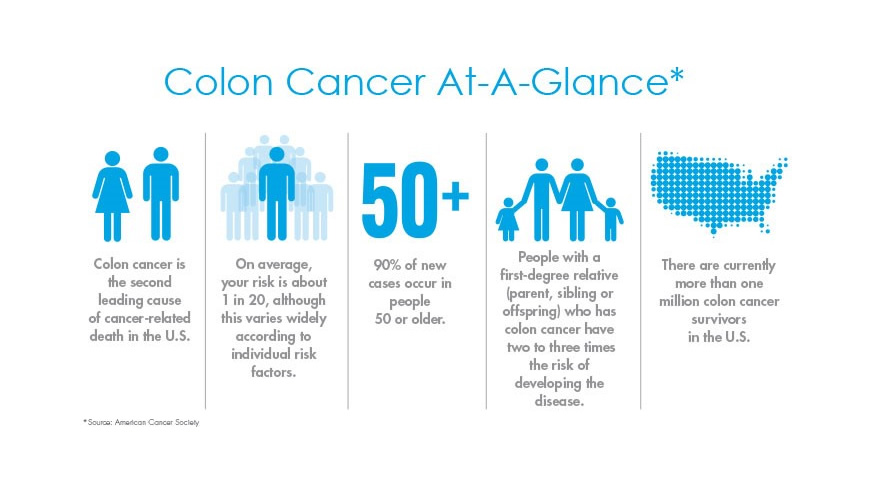
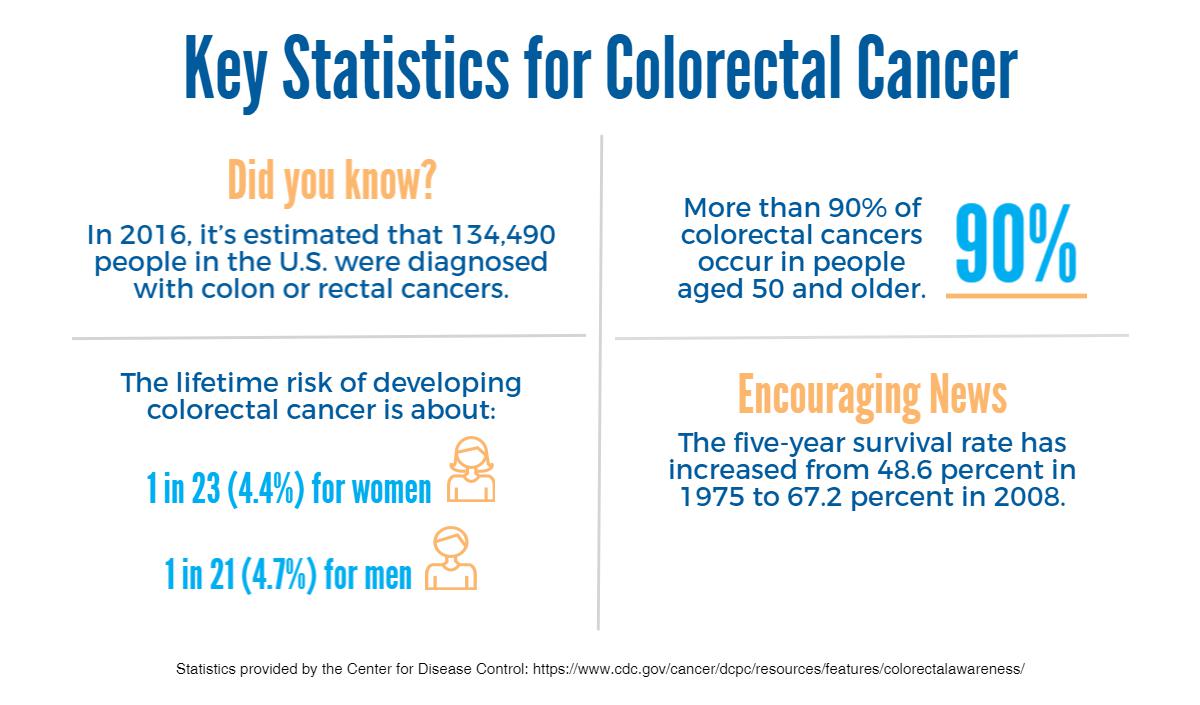
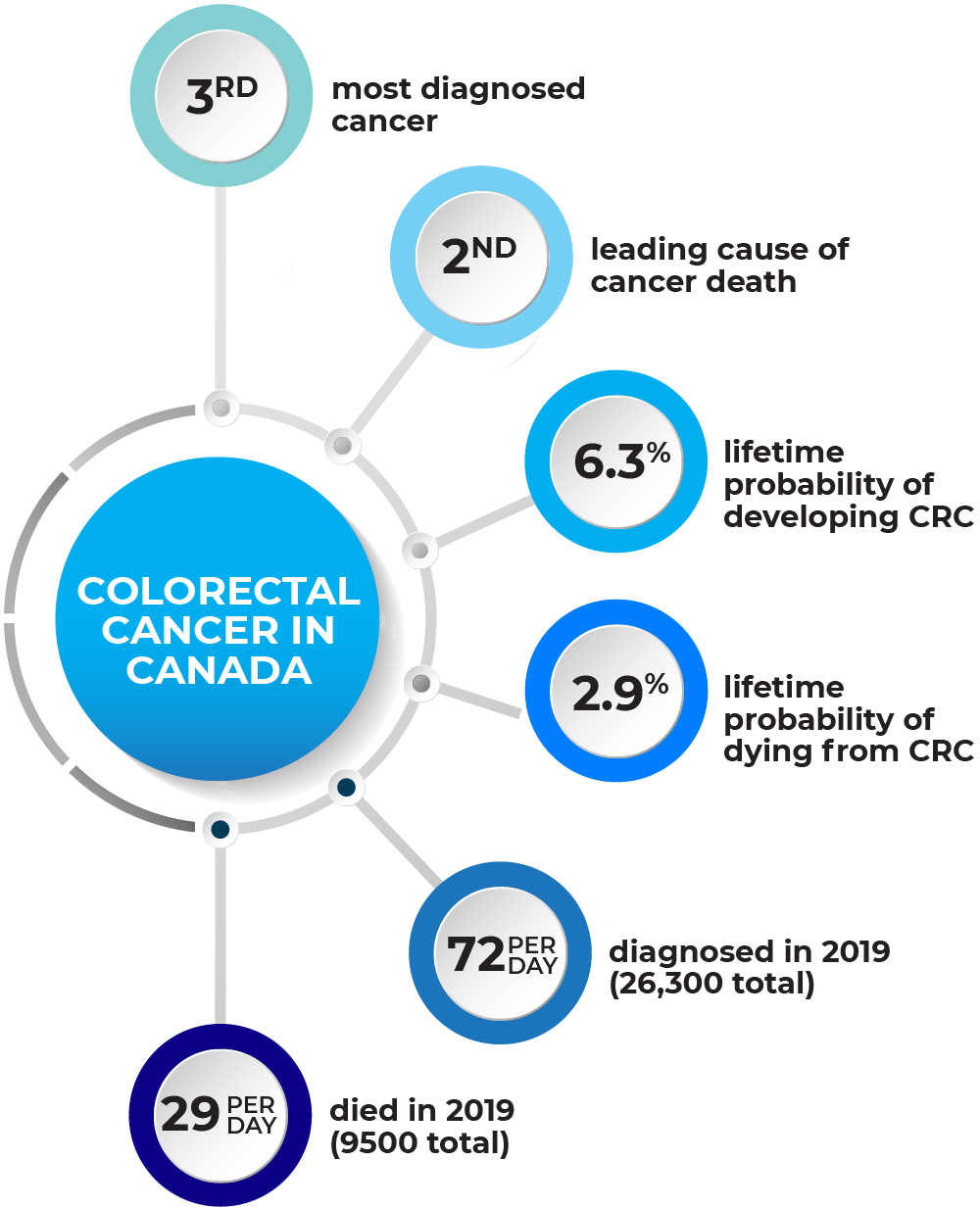
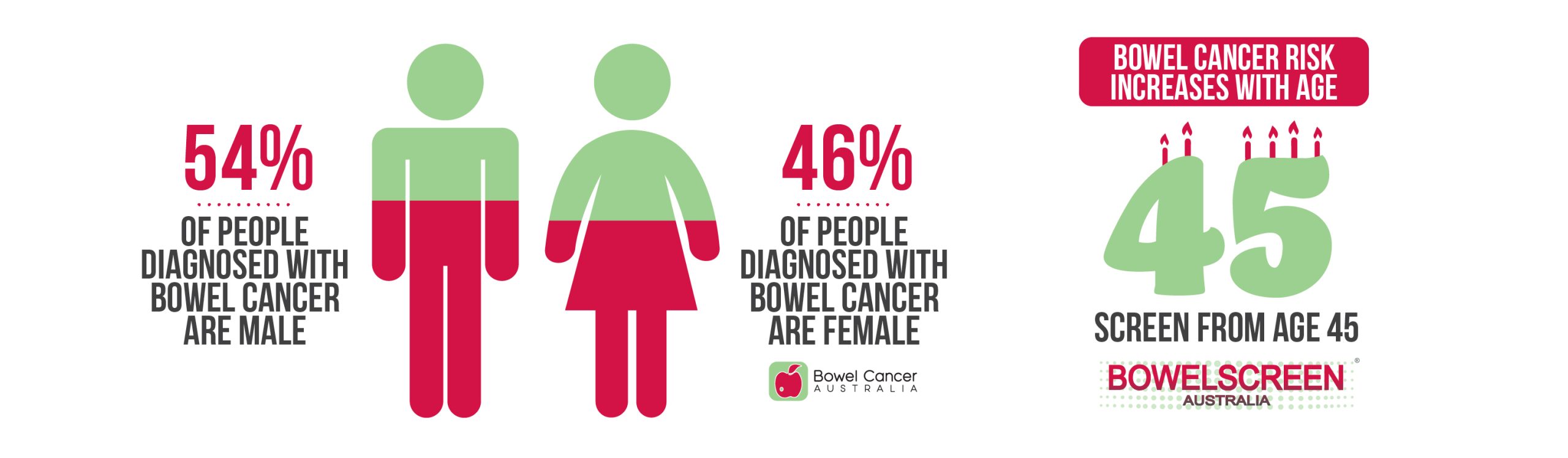
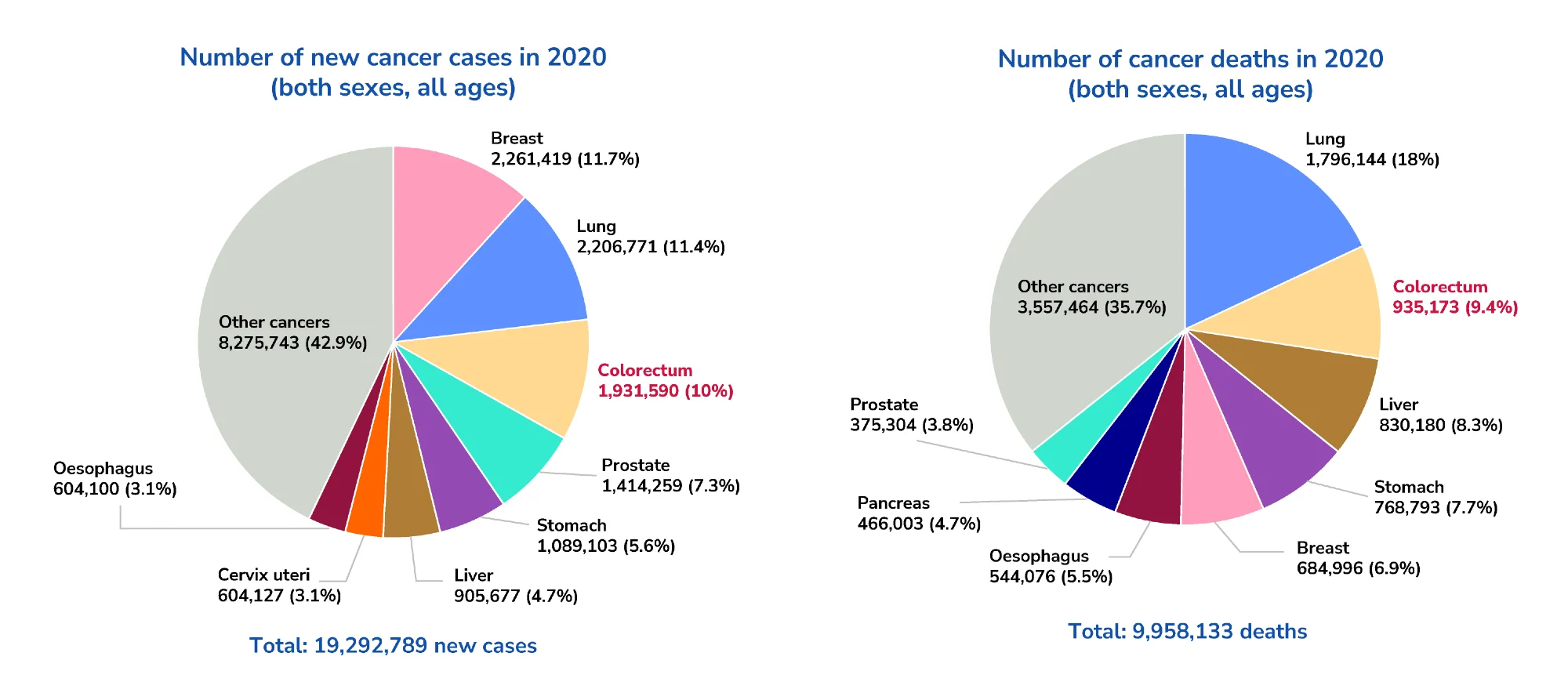
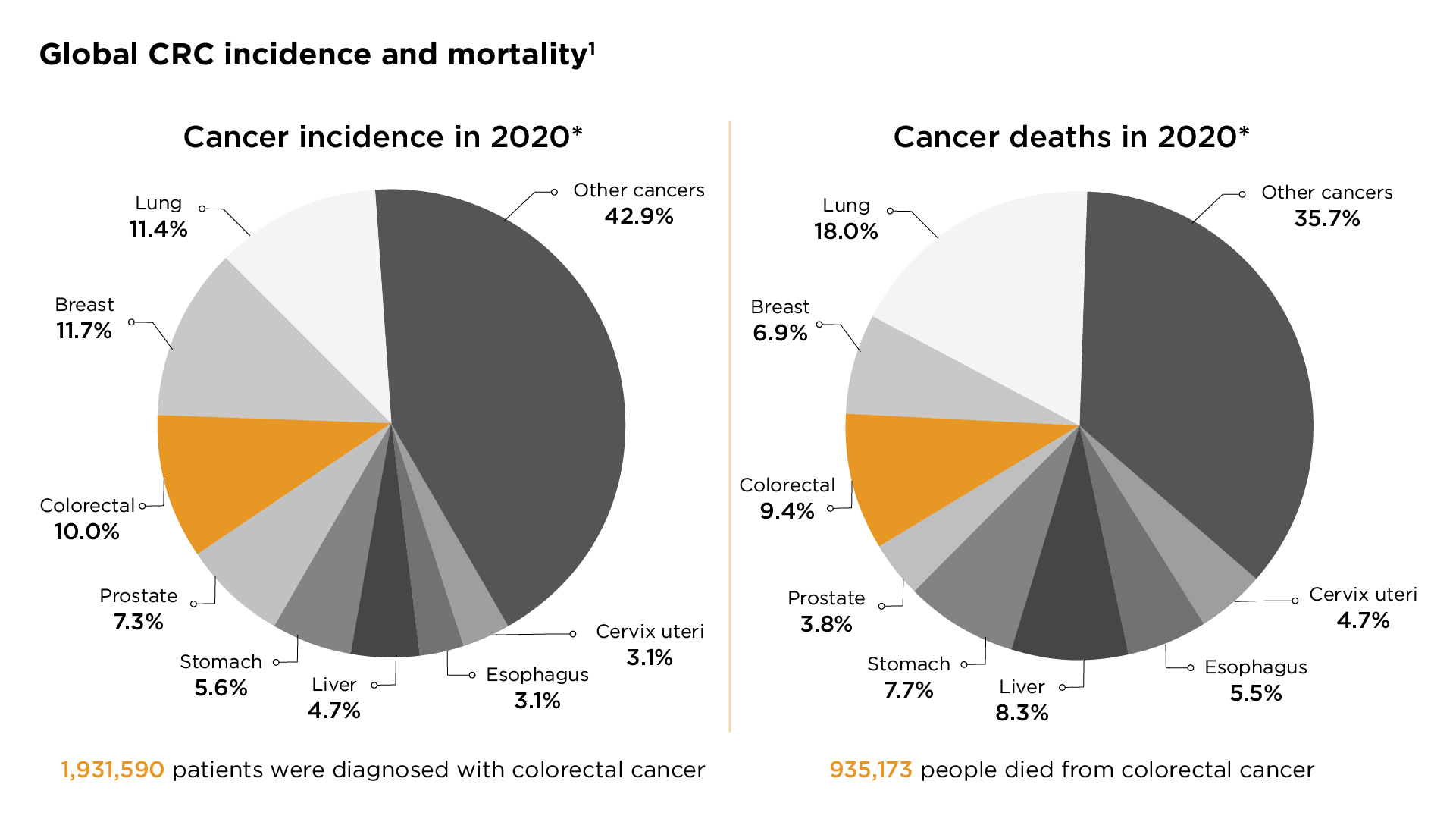
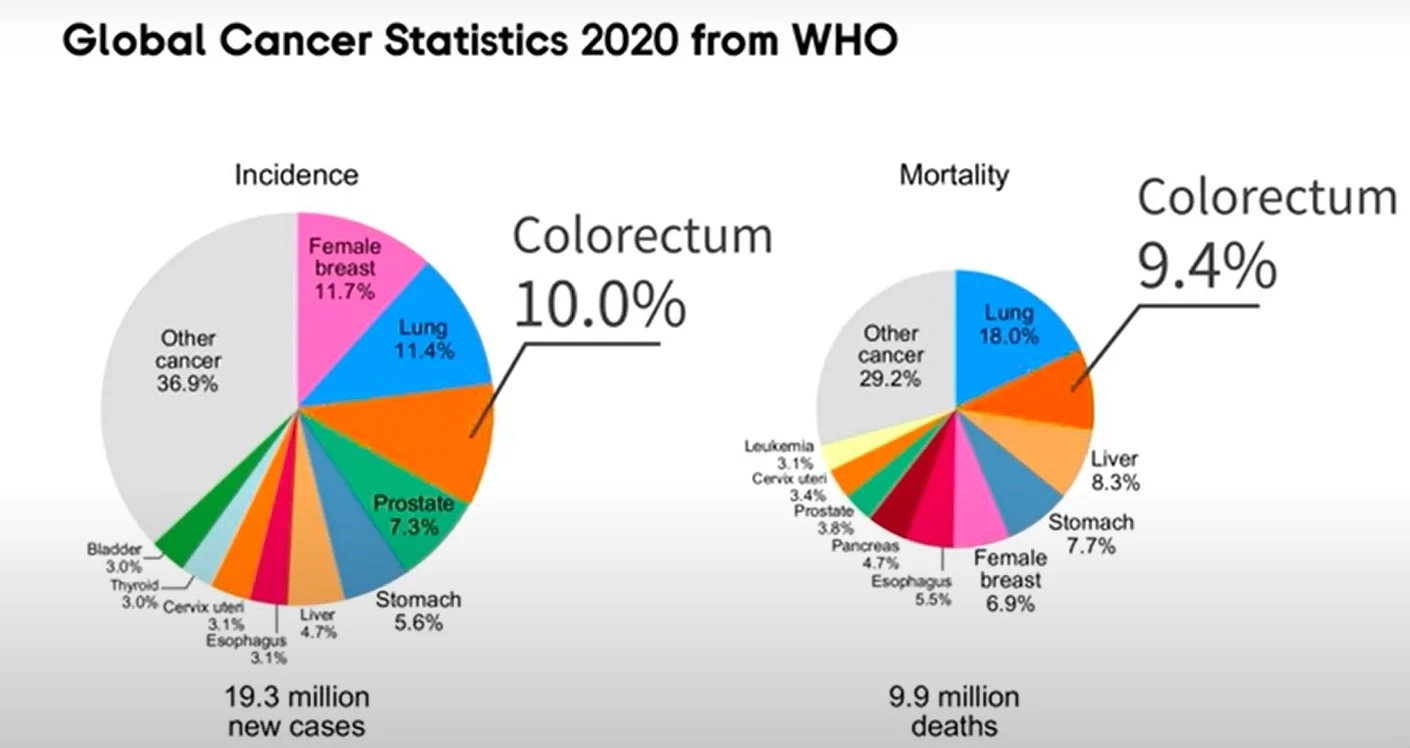
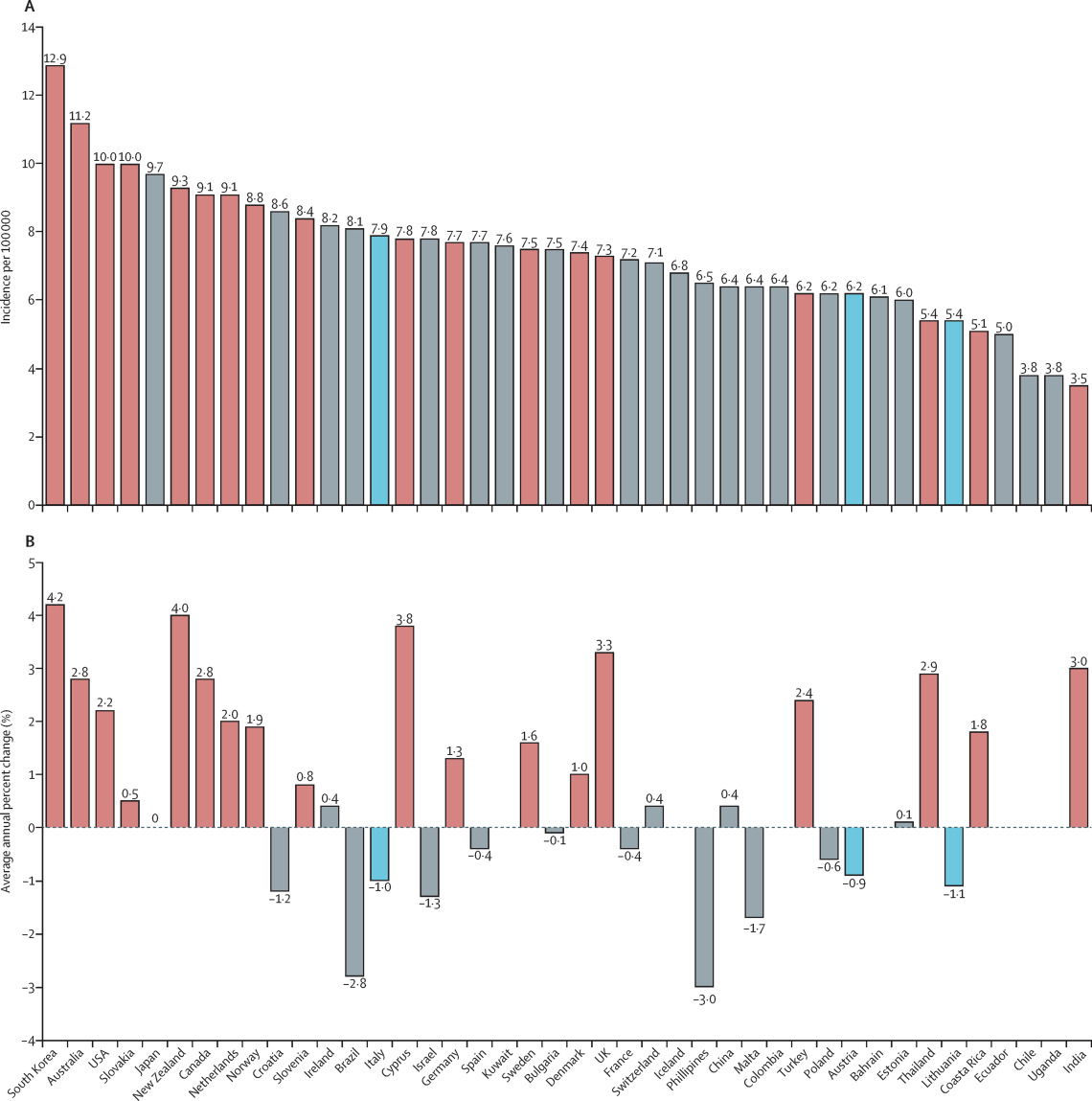
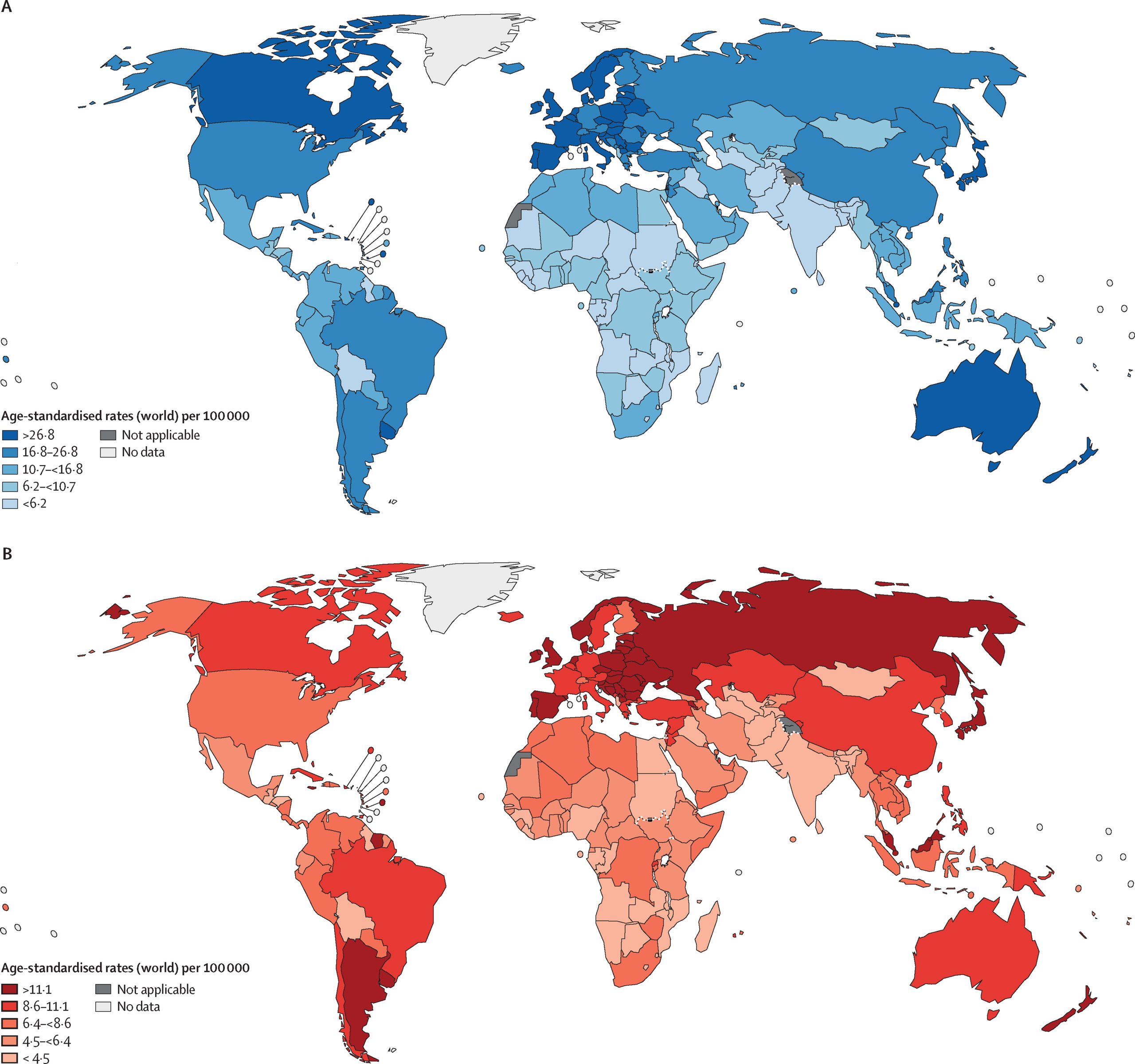
Bowel cancer is the second biggest cause of cancer deaths in Australia, and will affect 1 in 14 people by the time they reach 85. While it affects people of different ages, those aged between 50 and 74 are at a higher risk. The condition affects both men and women.
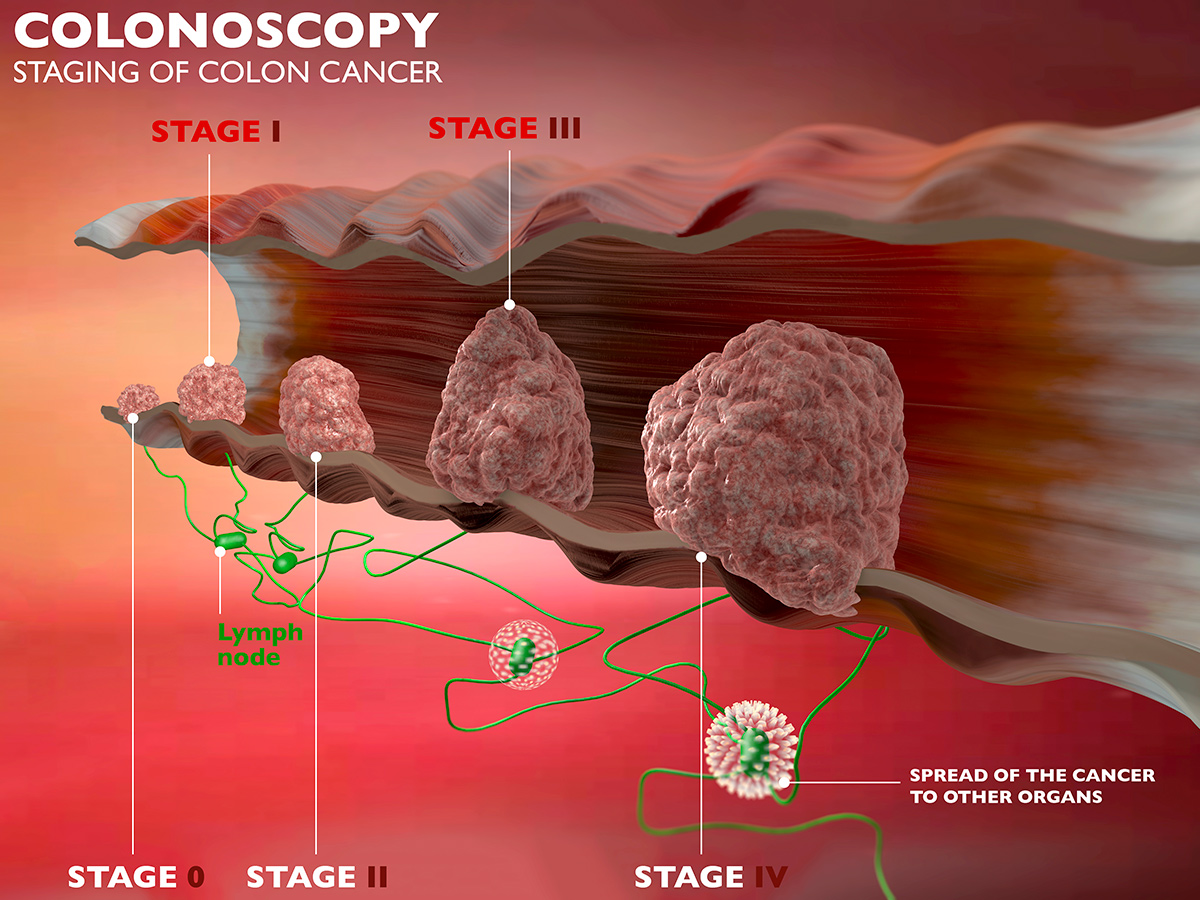
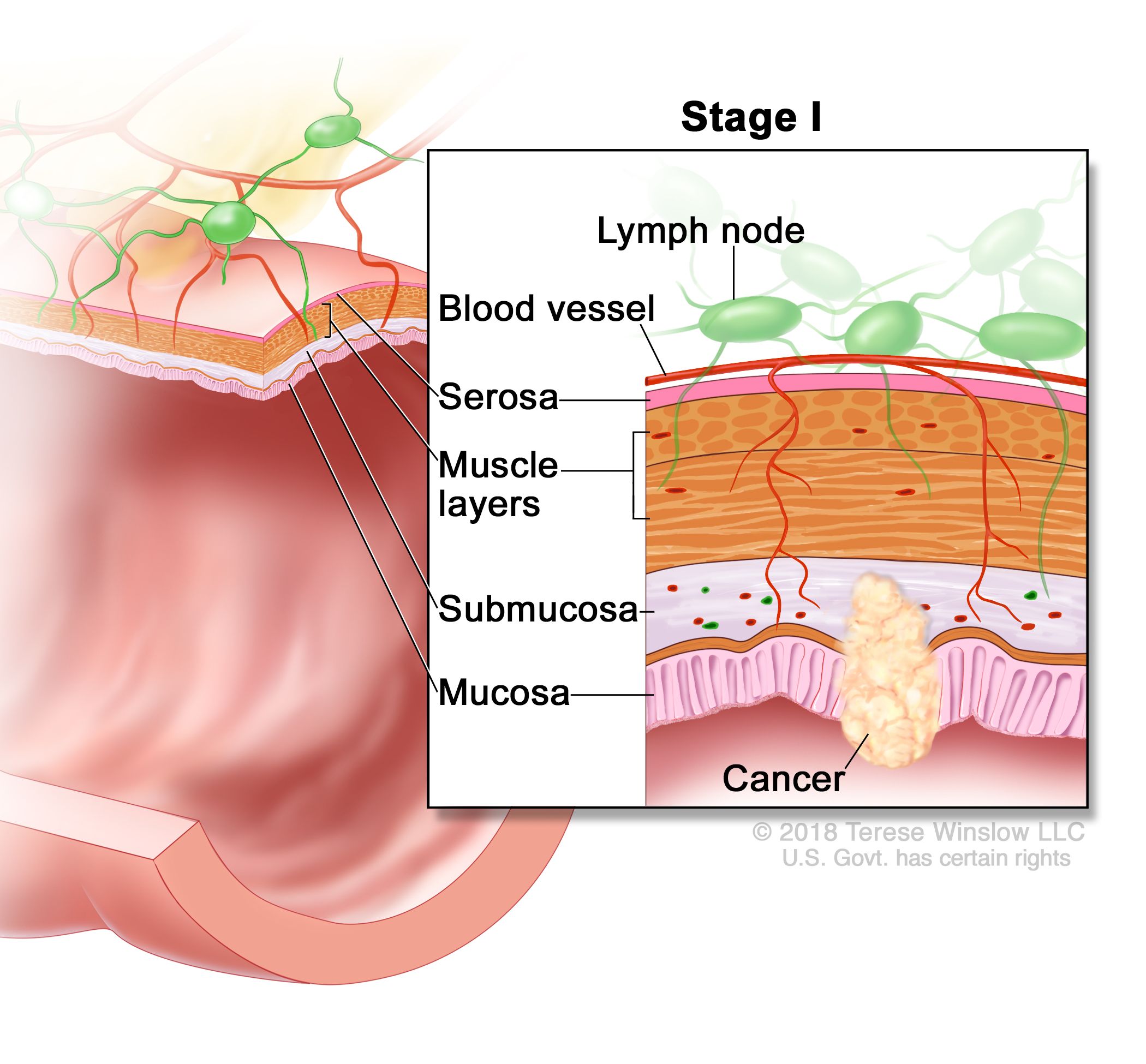
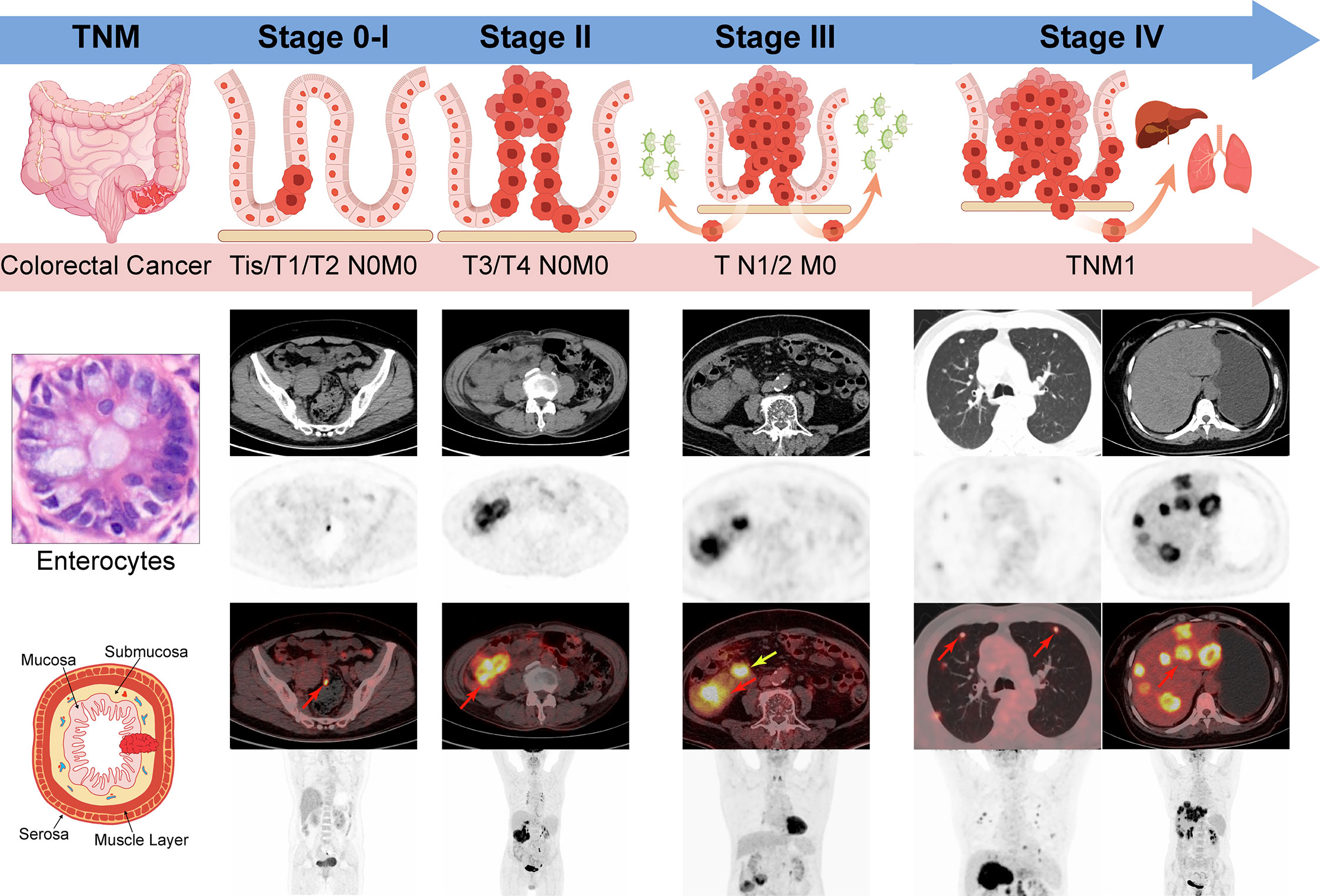
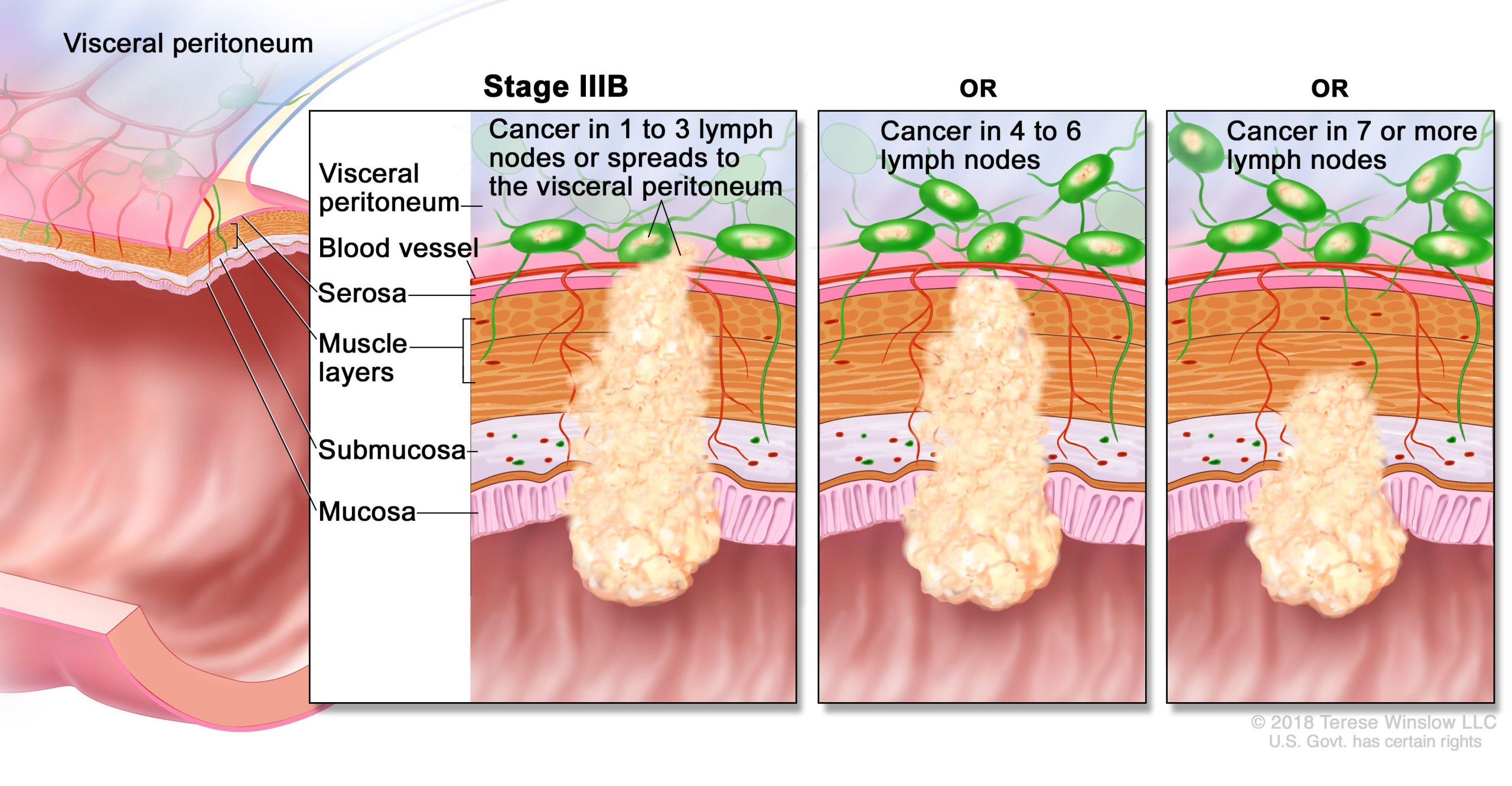
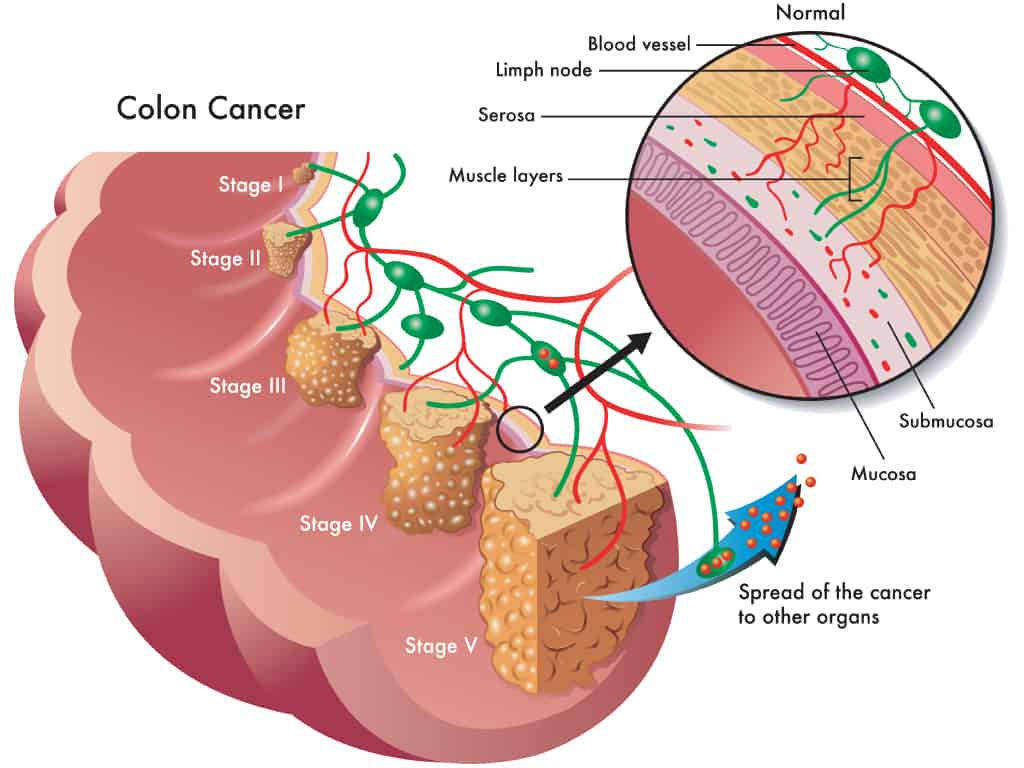
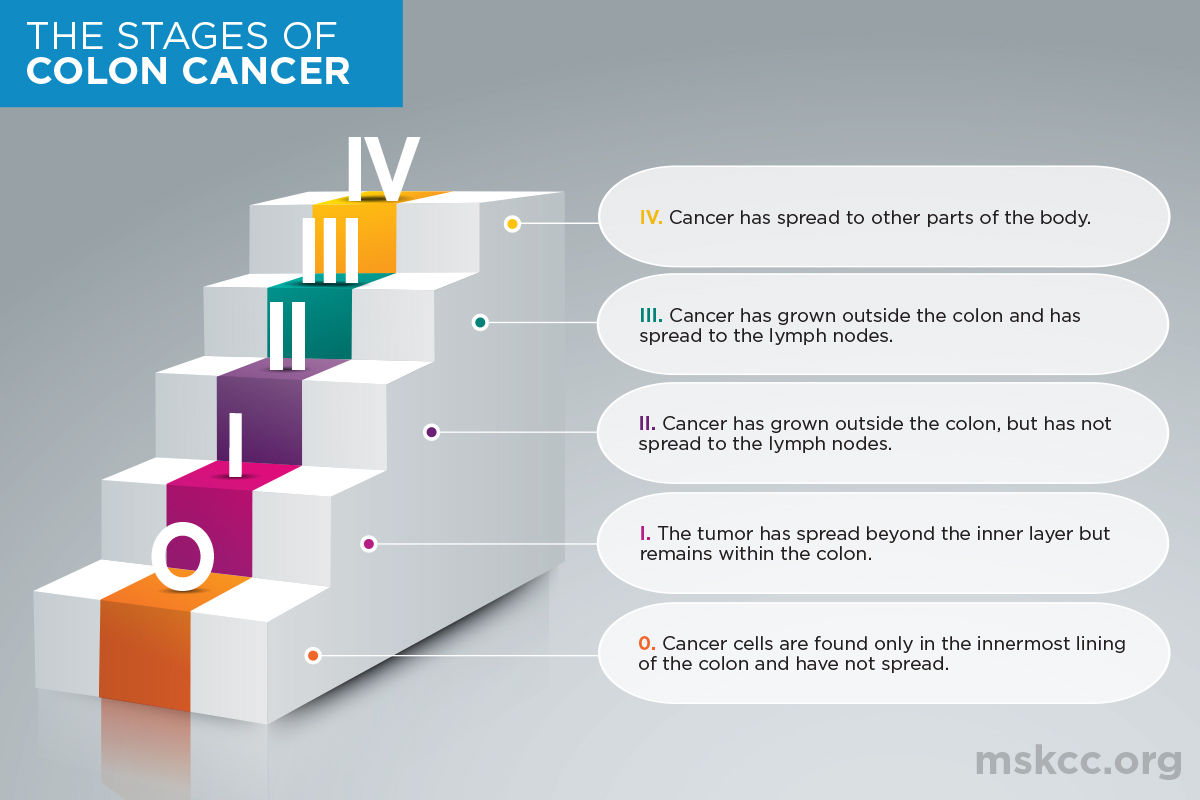
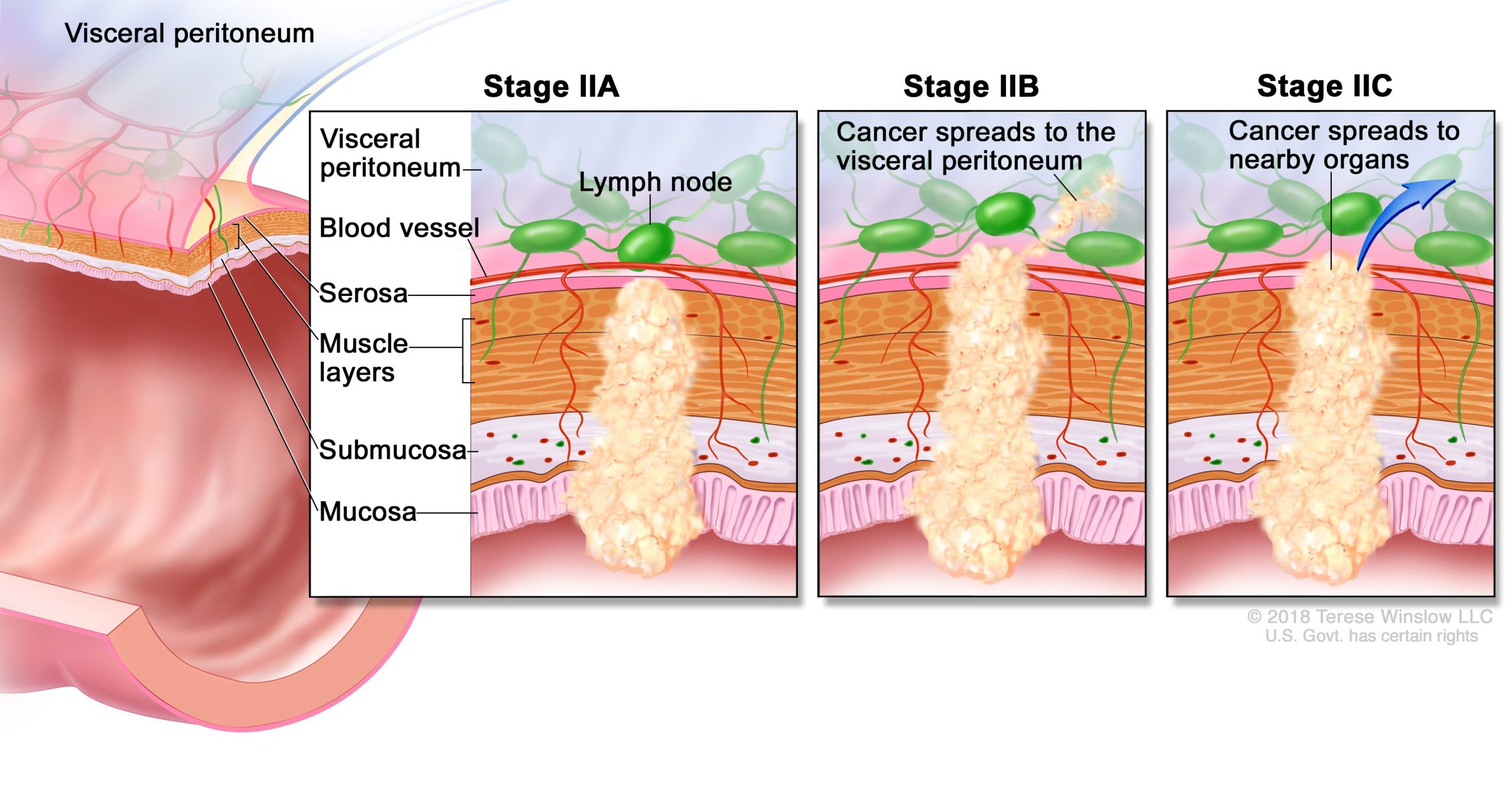
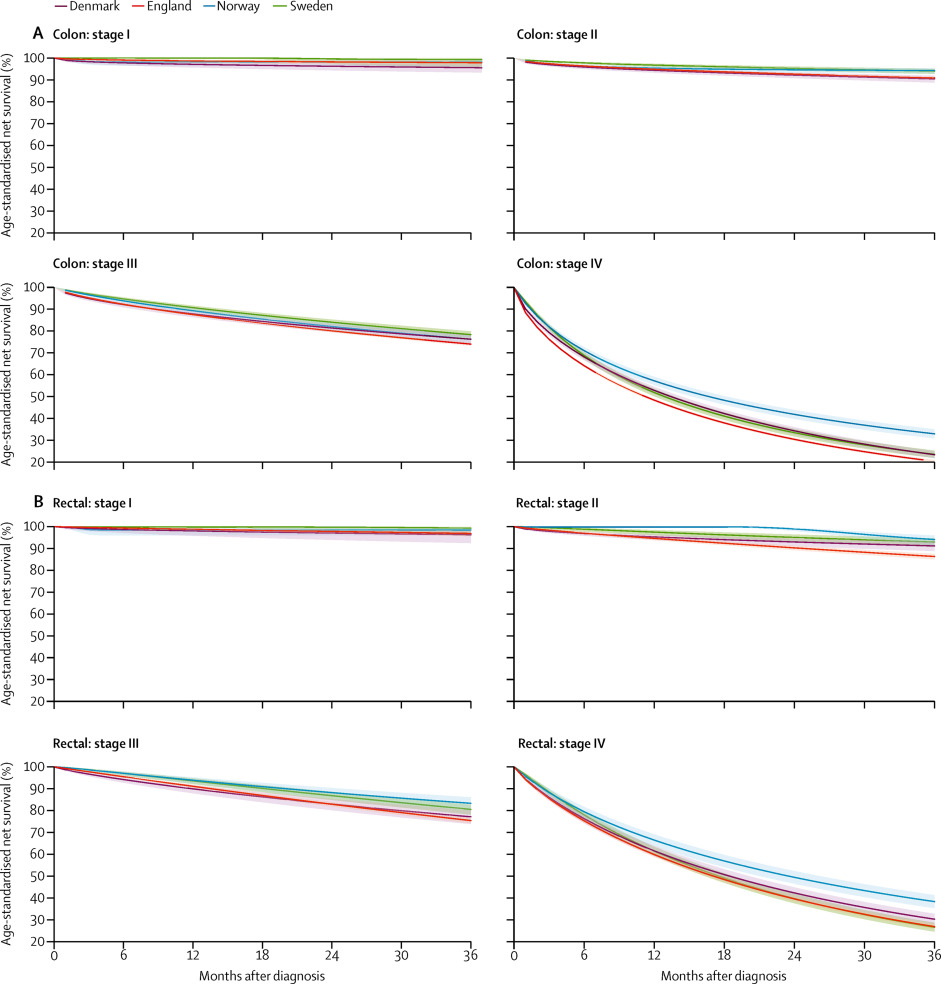
Bowel cancer is categorised into 4 stages, depending on where and how far it has spread through the body:
| Stage 0 (carcinoma in situ) | There are abnormal cells in your bowel lining that aren’t cancerous, but may become so. |
| Stage I | Cancer cells have spread deeper into your bowel wall (submucosa or muscle). |
| Stage II | Cancer has spread through the muscle of your bowel wall and perhaps into other organs. |
| Stage III | Cancer has spread to lymph nodes and organs nearby. |
| Stage IV | Cancer has spread further to other parts of your body (for example, the lungs or liver). |
Bowel cancer generally does not spread quickly. Any small growths or polyps in your bowel wall may take several years to become cancerous.
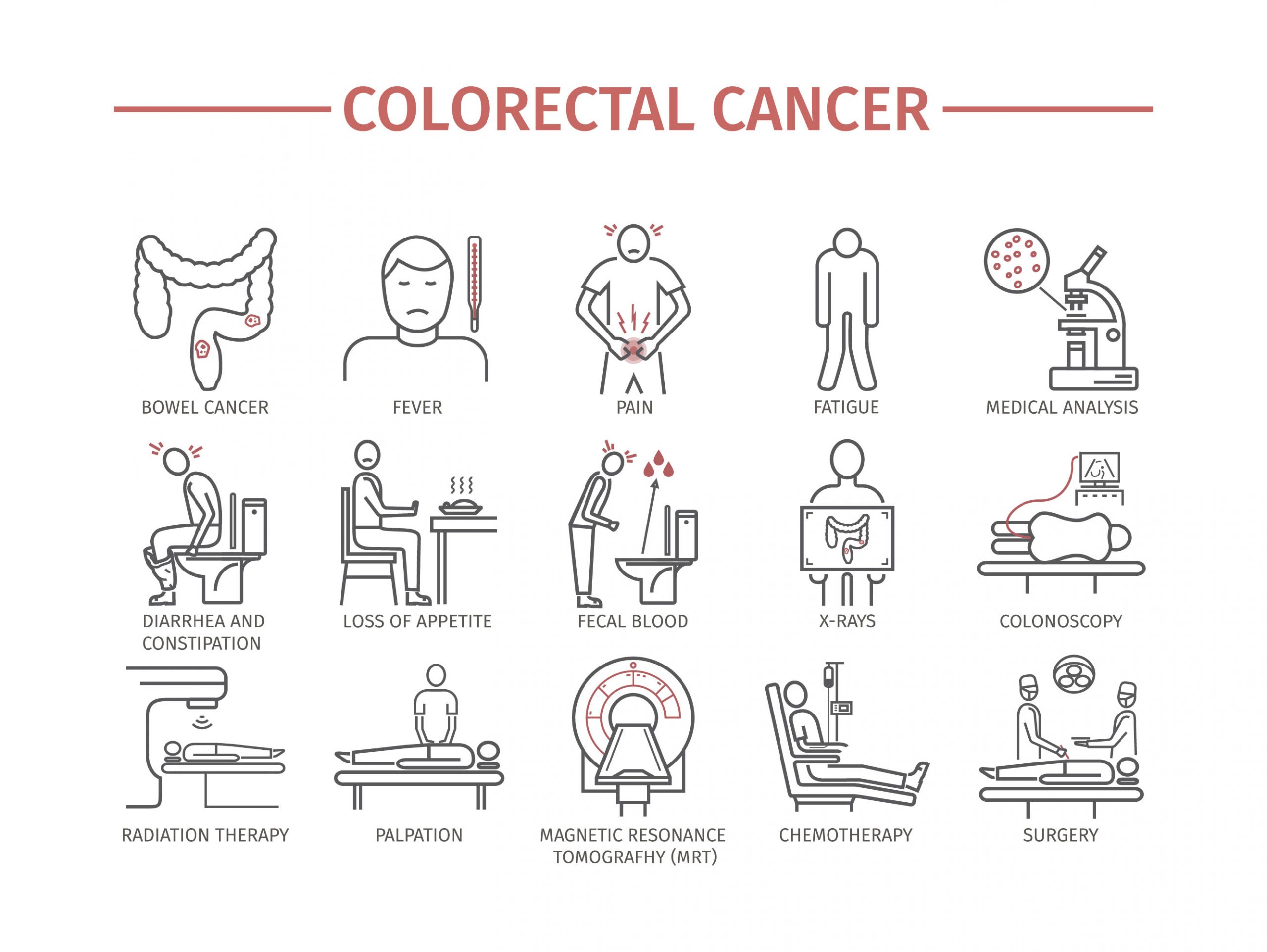
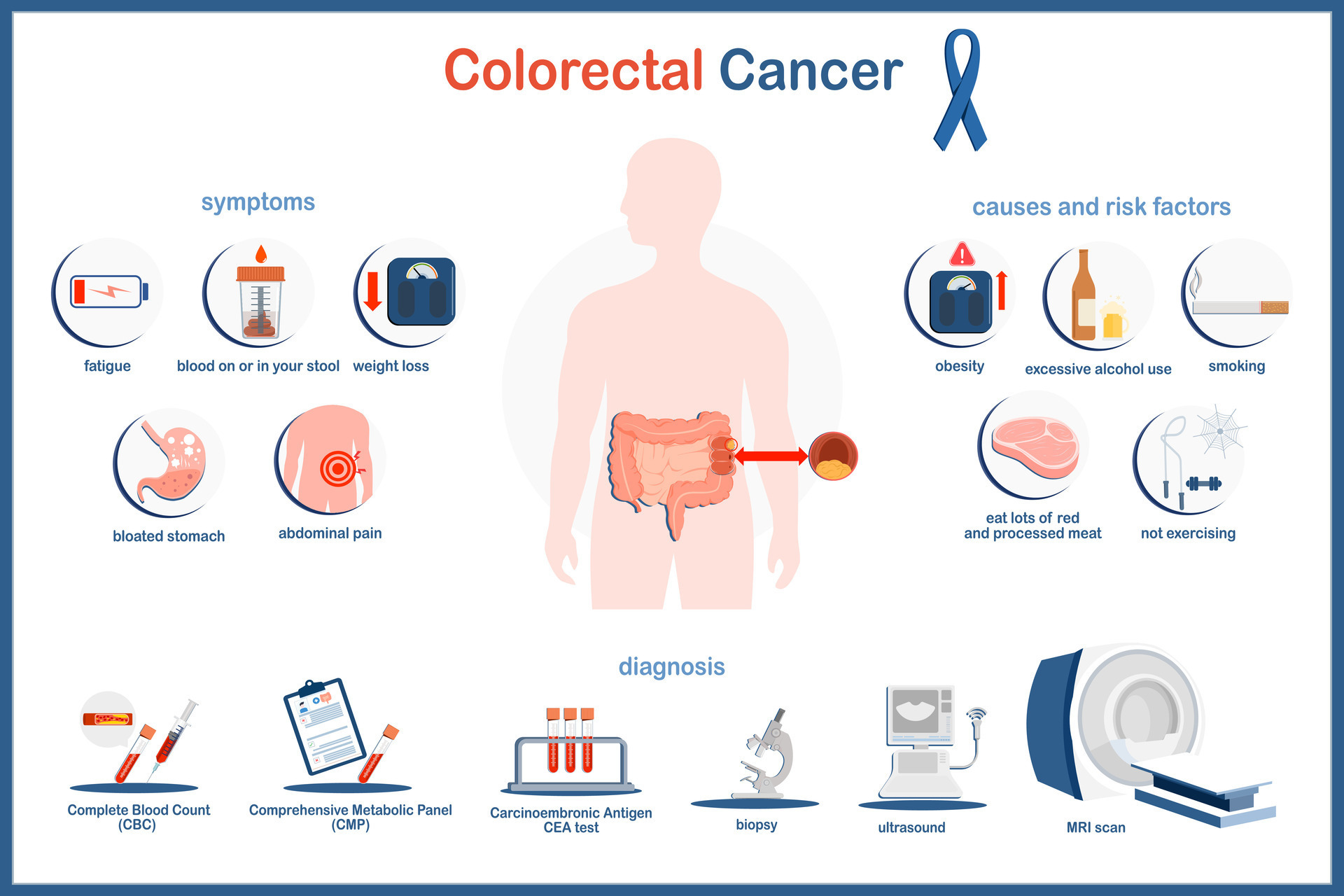
What are the symptoms of bowel cancer?
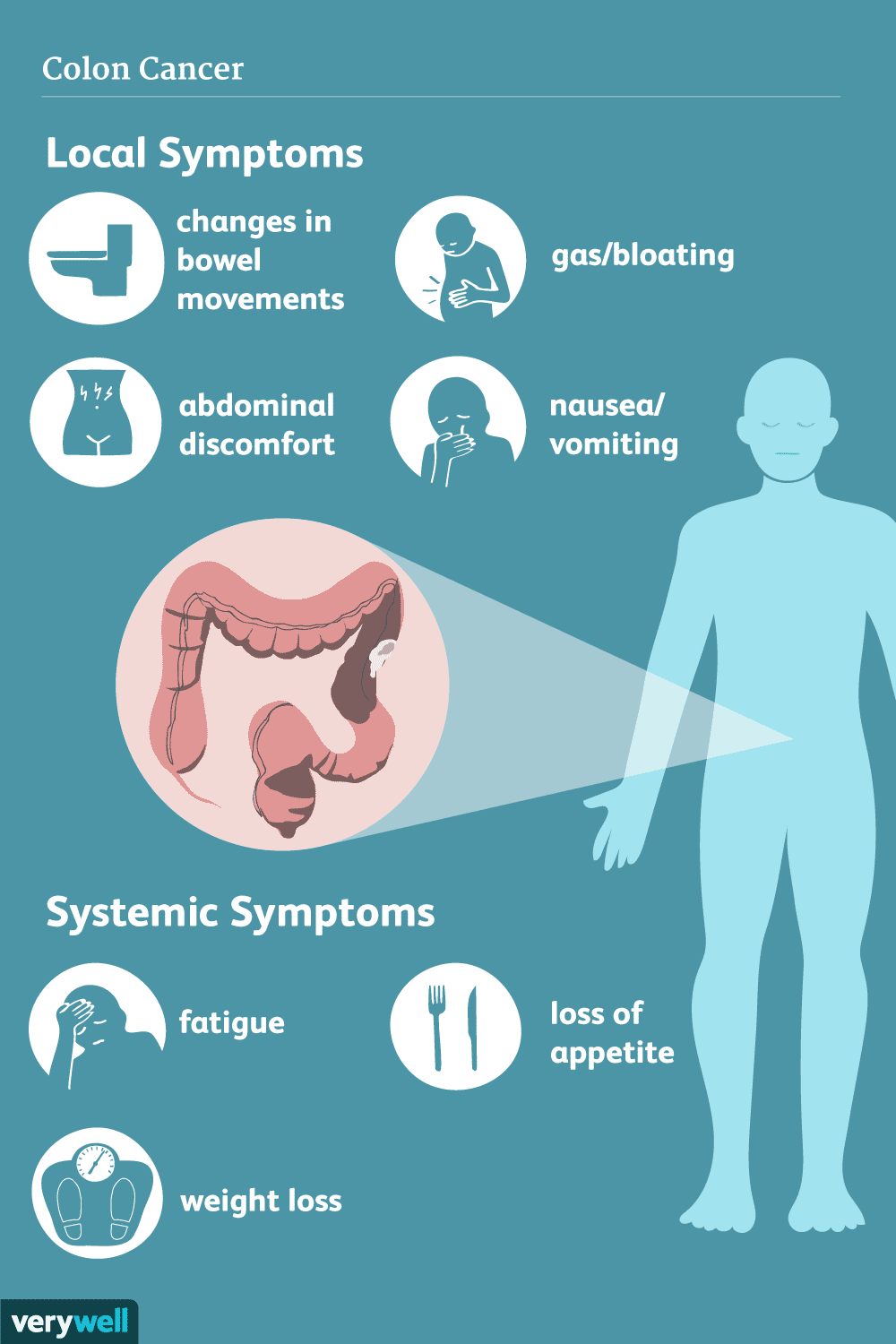
The early signs and symptoms of bowel cancer can be easy to miss, but they may include:
- bleeding from the rectum (back passage), or blood in your stools (faeces or poo)
- a recent, ongoing change in bowel habits — for example, looser stools, constipation, more frequent trips to the toilet, or stools that are narrower than usual
- abdominal pain, cramping or bloating
- unexplained weight loss
- unexplained tiredness (which may also be due to anaemia)
What causes bowel cancer?
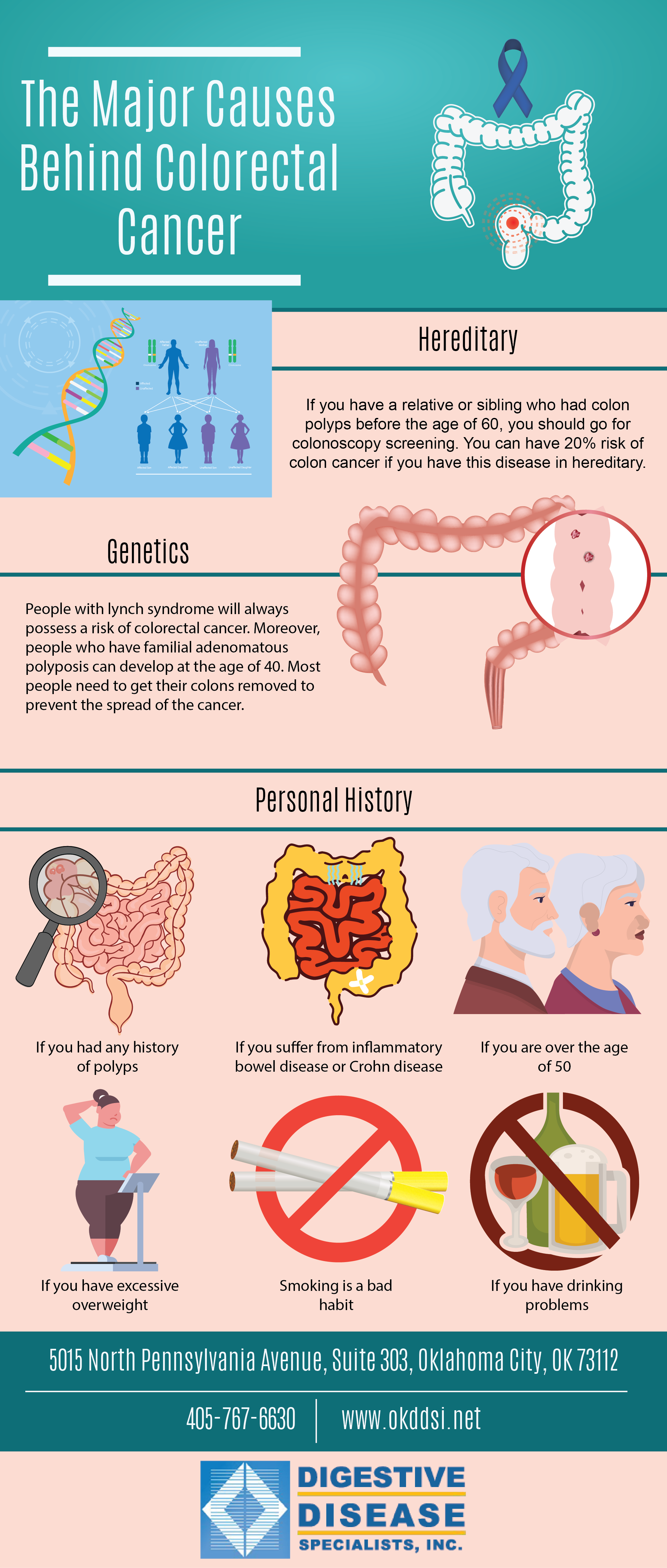
Several lifestyle factors can increase your risk of bowel cancer:
- eating too much processed meat (for example, bacon, ham, salami, sausages)
- eating too much red meat (for example, beef, lamb, pork)
- drinking too much alcohol, especially if you drink more than two standard drinks per day
- unhealthy weight (being overweight or obese)
- smoking, especially if you smoke more than 2 packs a day
- not enough physical activity
Other factors that can’t be changed may also increase your chances of bowel cancer, including:
- Your age — From age 50, your risk increases.
- Your family history — Around 3 in 10 cases of bowel cancer have a strong family link. The more members of your family affected by bowel cancer, and the younger they were when diagnosed, the more likely it is that you will also develop bowel cancer.
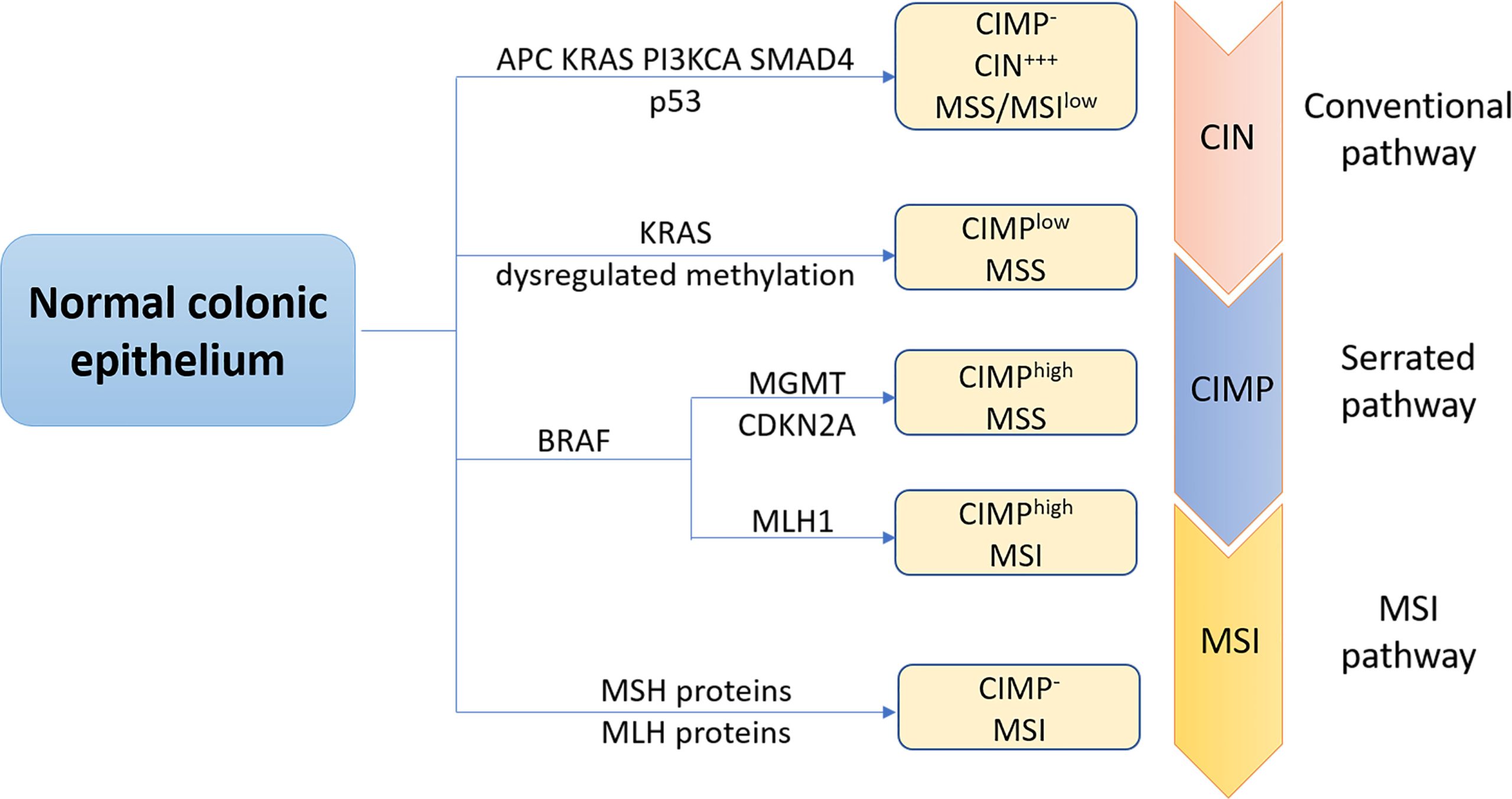
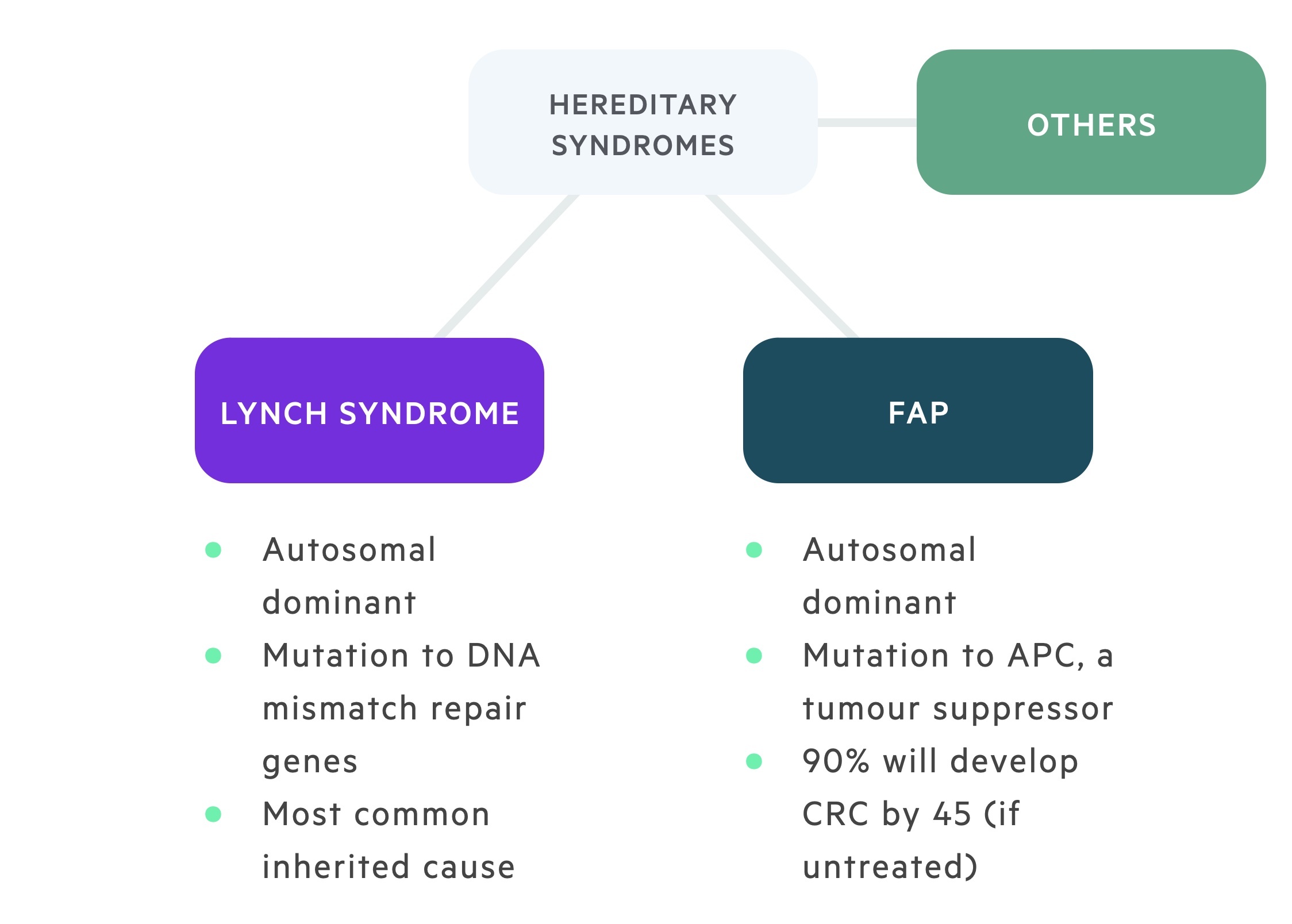
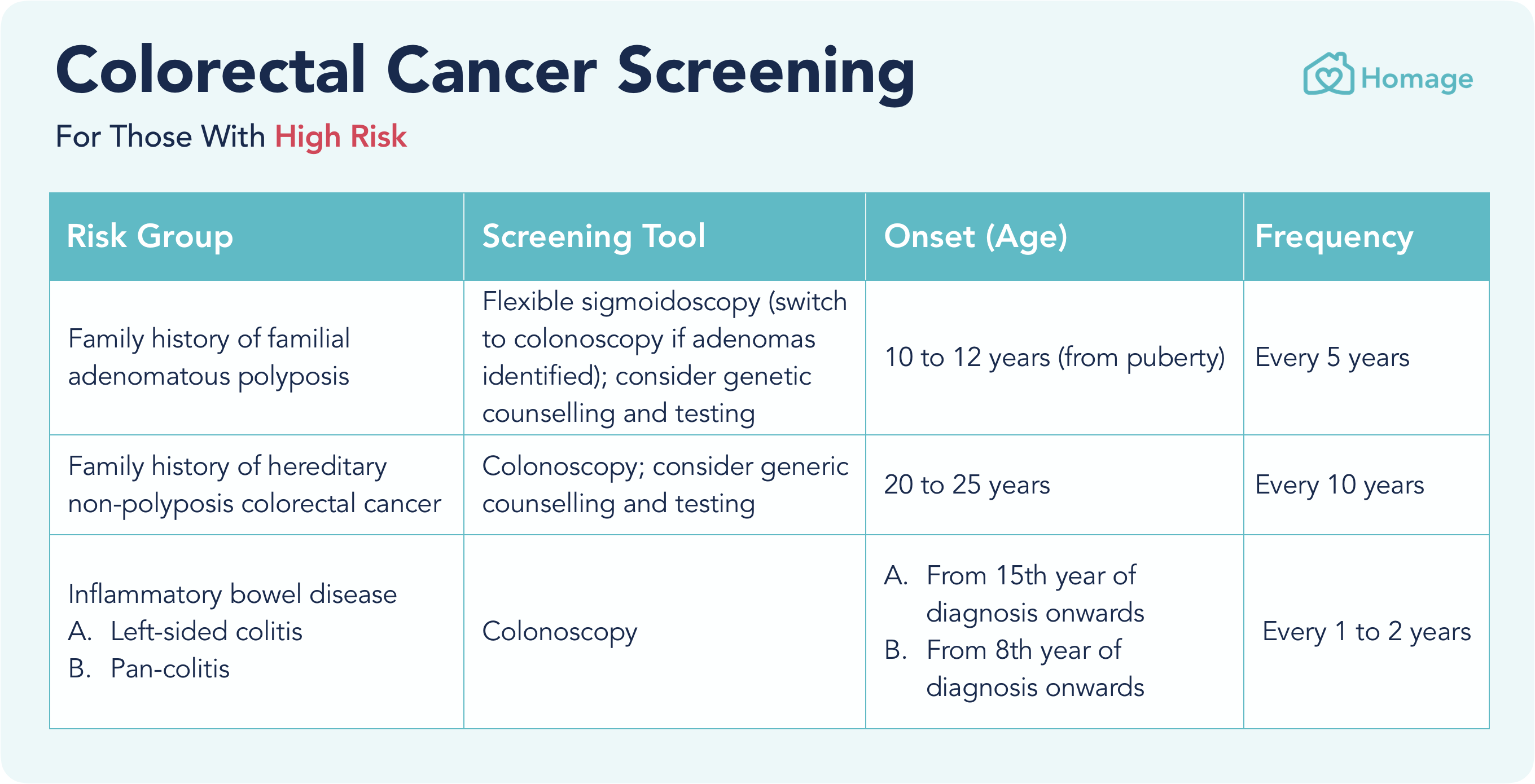
- Genetic mutations — Up to 1 in 10 cases of bowel cancer are due to rare genetic mutations. These either remove your protection against getting cancer (Lynch Syndrome), or cause hundreds of polyps to grow in your large bowel (familial adenomatous polyposis, MYH-associated polyposis).
- Inflammatory bowel disease (IBD) — People with Crohn’s disease and ulcerative colitis have a higher risk of developing bowel cancer over time, and experience similar symptoms.
What’s your risk?
Check your cancer risk with Cancer Australia’s calculator.
When should I see my doctor?
See your doctor or healthcare professional if you have blood in your stool, unexplained changes in your bowel habits, tiredness, abdominal pain or any other symptoms that may indicate bowel cancer.
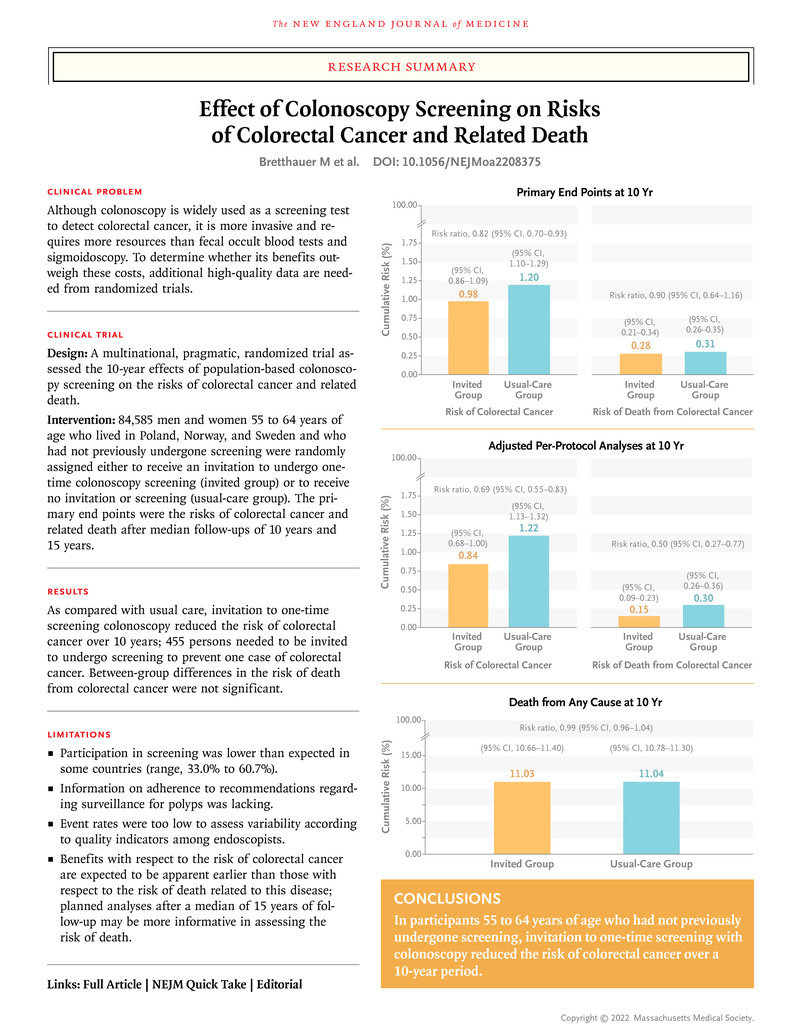
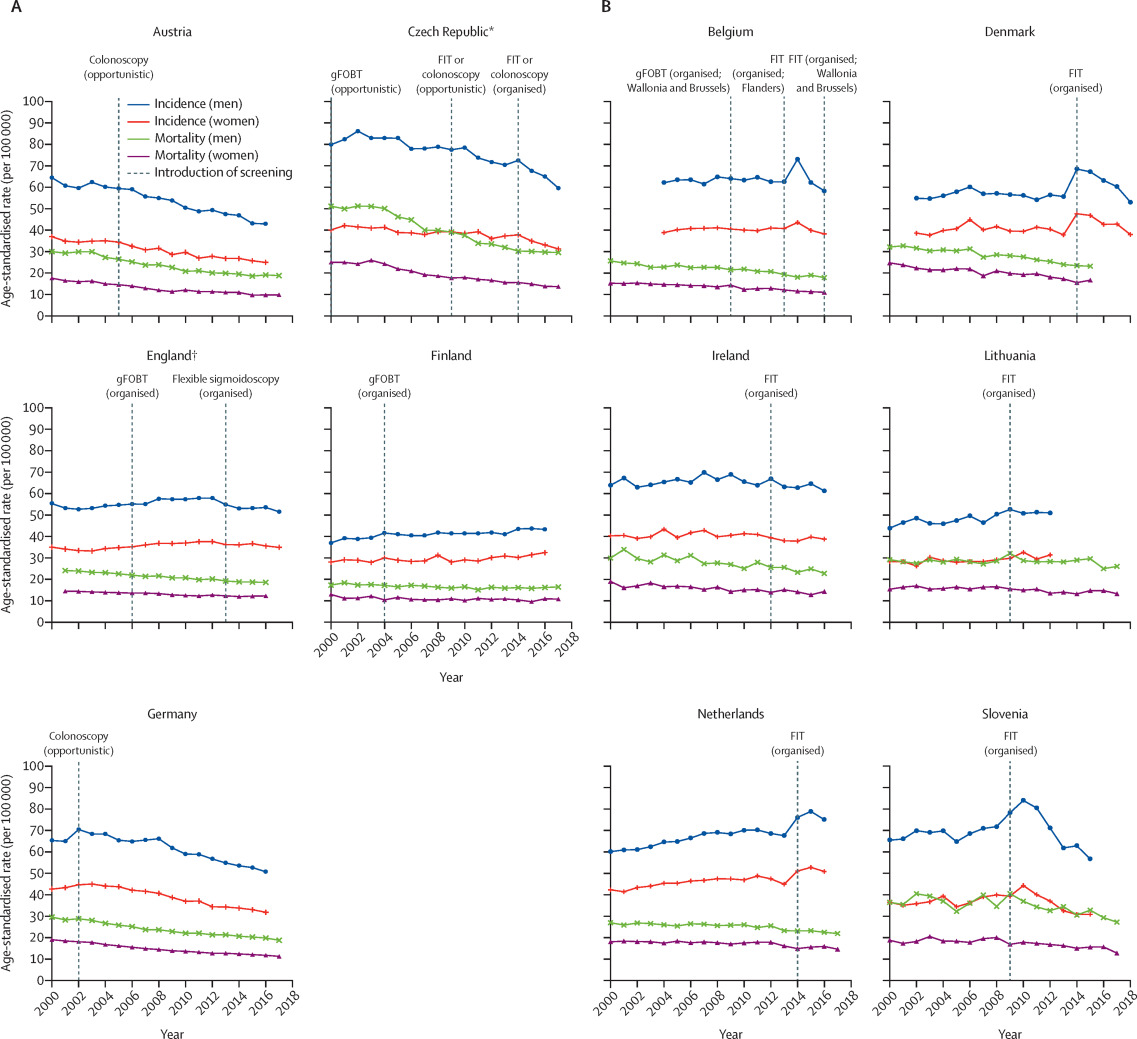
Can I be screened for bowel cancer?
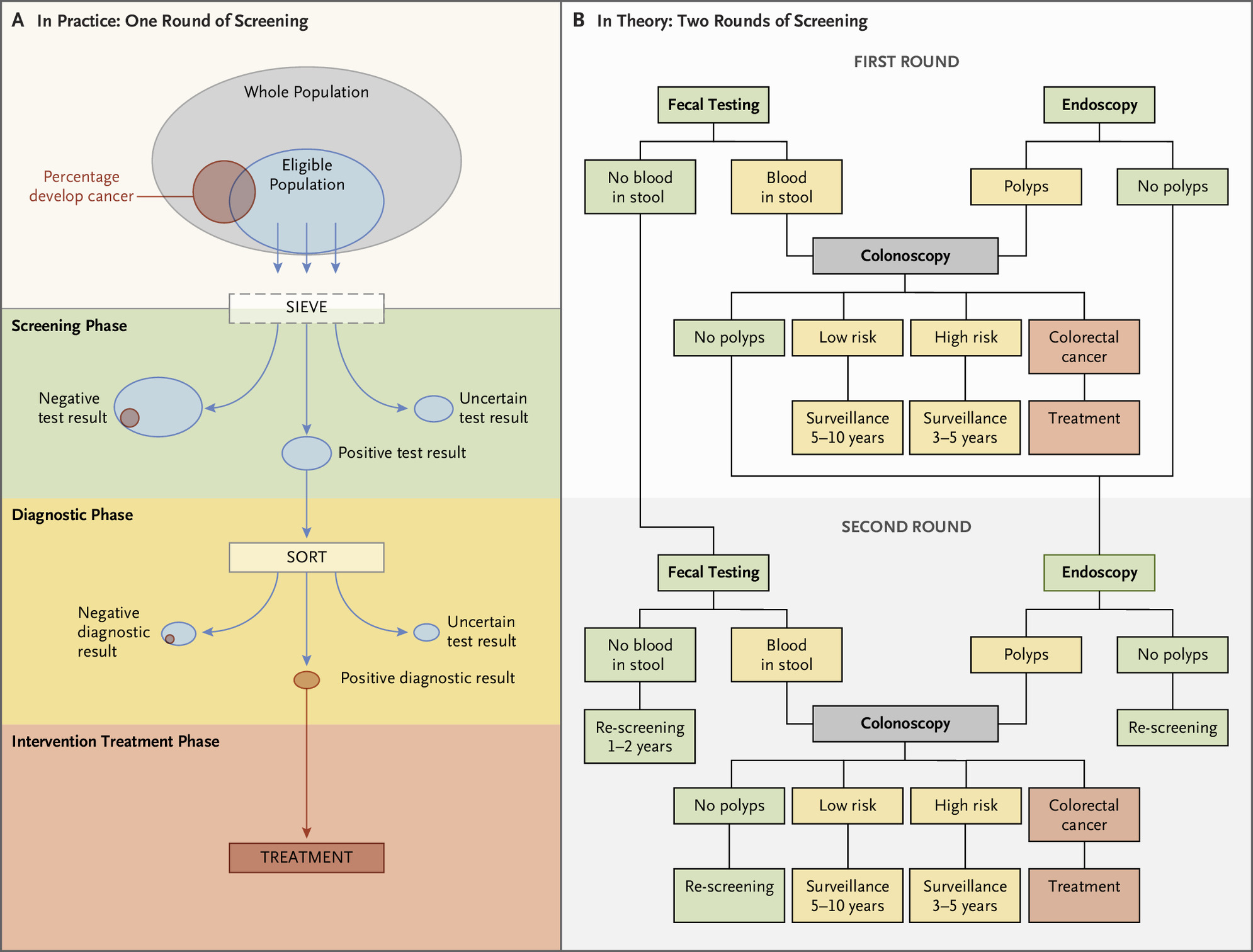
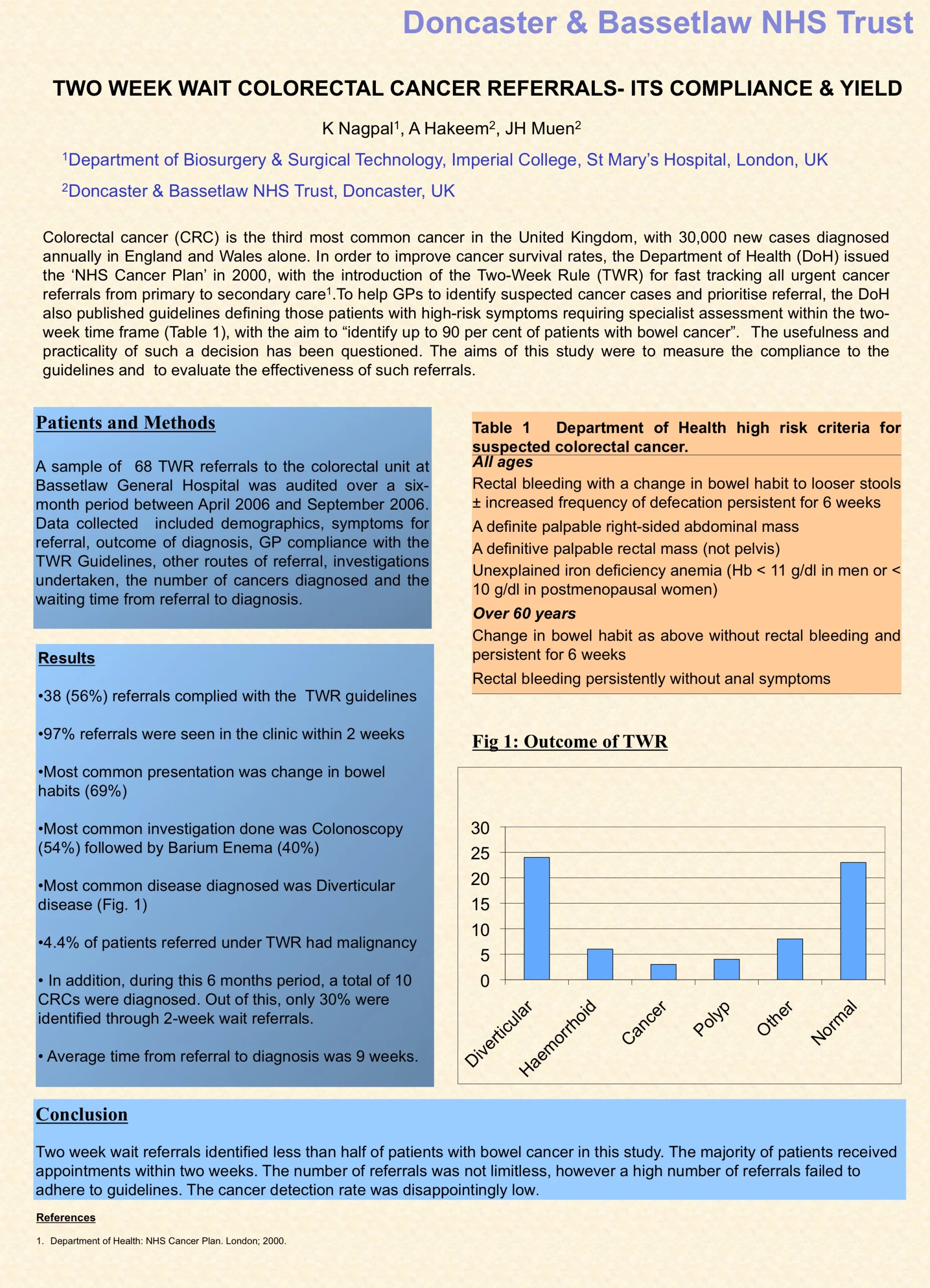
One of the main reasons people die from bowel cancer is late detection: 1 in 2 cases are not detected early enough for successful treatment.
The National Bowel Cancer Screening Program (NBCSP) offers free screening to all Australians at risk of bowel cancer. If you’re aged between 50 and 74 years of age, you’ll be invited to have a simple, free test that you can complete at home. This can help reveal early signs of bowel cancer before noticeable ones emerge.
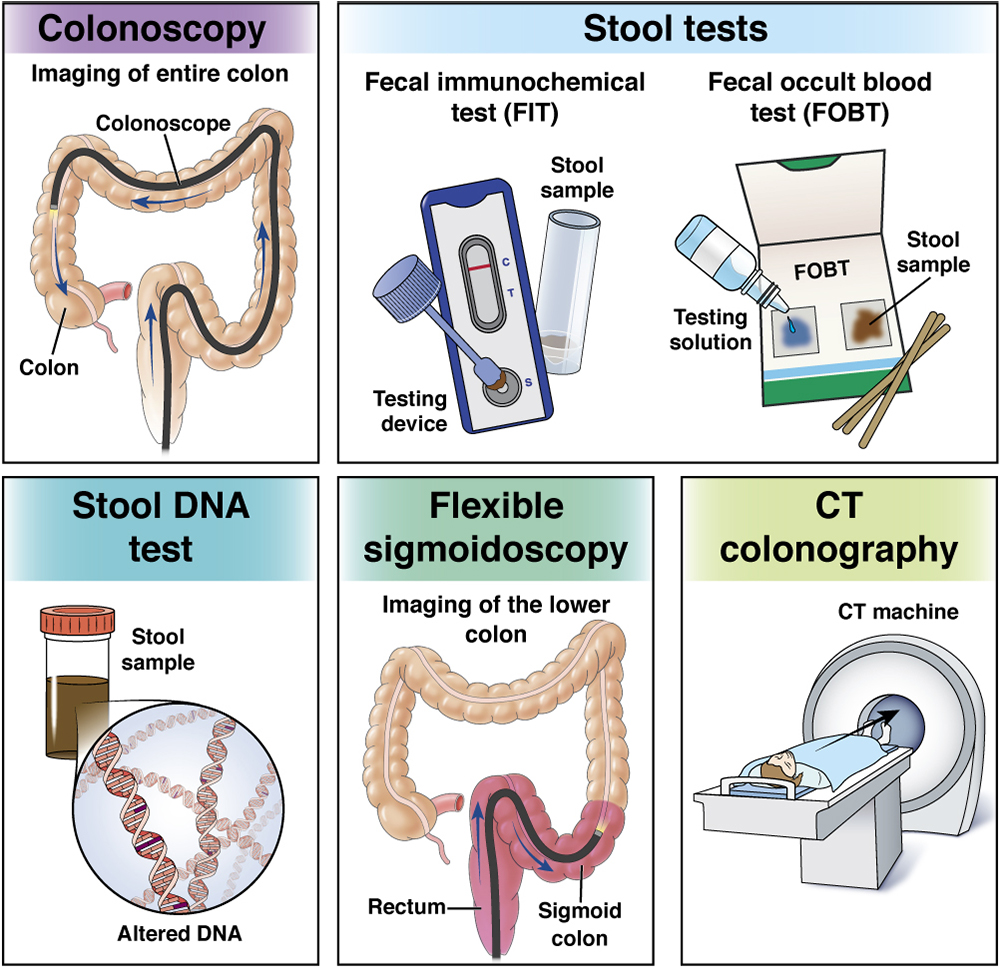
The screening test is the faecal immunochemical test (FIT or iFOBT), which can reveal non-visible blood in your stool sample which may signal bowel cancer. This test has superseded the faecal occult blood test (FOBT) for bowel cancer screening in Australia.
If you’re under 50 and concerned about your bowel cancer risk, or you have a significant family history of bowel cancer, speak with your doctor about your situation and what tests are appropriate for you.
How is bowel cancer diagnosed?
Tests for bowel cancer
If you are experiencing symptoms or return a positive test from bowel cancer screening, your doctor may conduct the following tests to confirm or rule out bowel cancer:
- a physical examination
- blood tests for anaemia
- a colonoscopy or sigmoidoscopy to see inside your colon, rectum and anal canal
- imaging scans of your bowel such as a barium enema (a colon x-ray), CT or MRI scan
- a biopsy to take a sample of tissue from your bowel wall
- a chest x-ray to see whether the cancer has spread to your lungs
- a lymph node biopsy
- an ultrasound
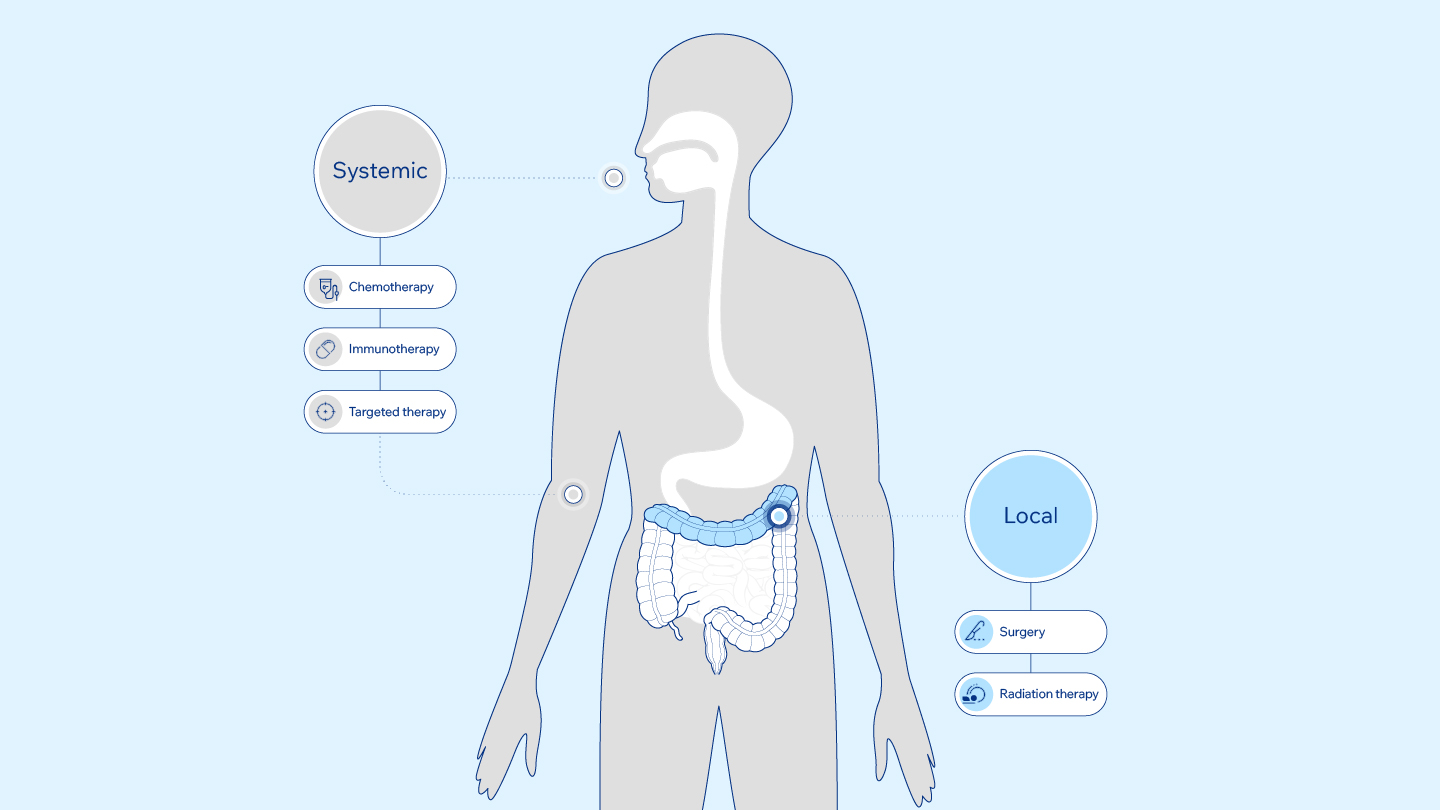
How is bowel cancer treated?
Depending on the stage of the bowel cancer, your current health and preferences, there are several different treatment options.
Surgery
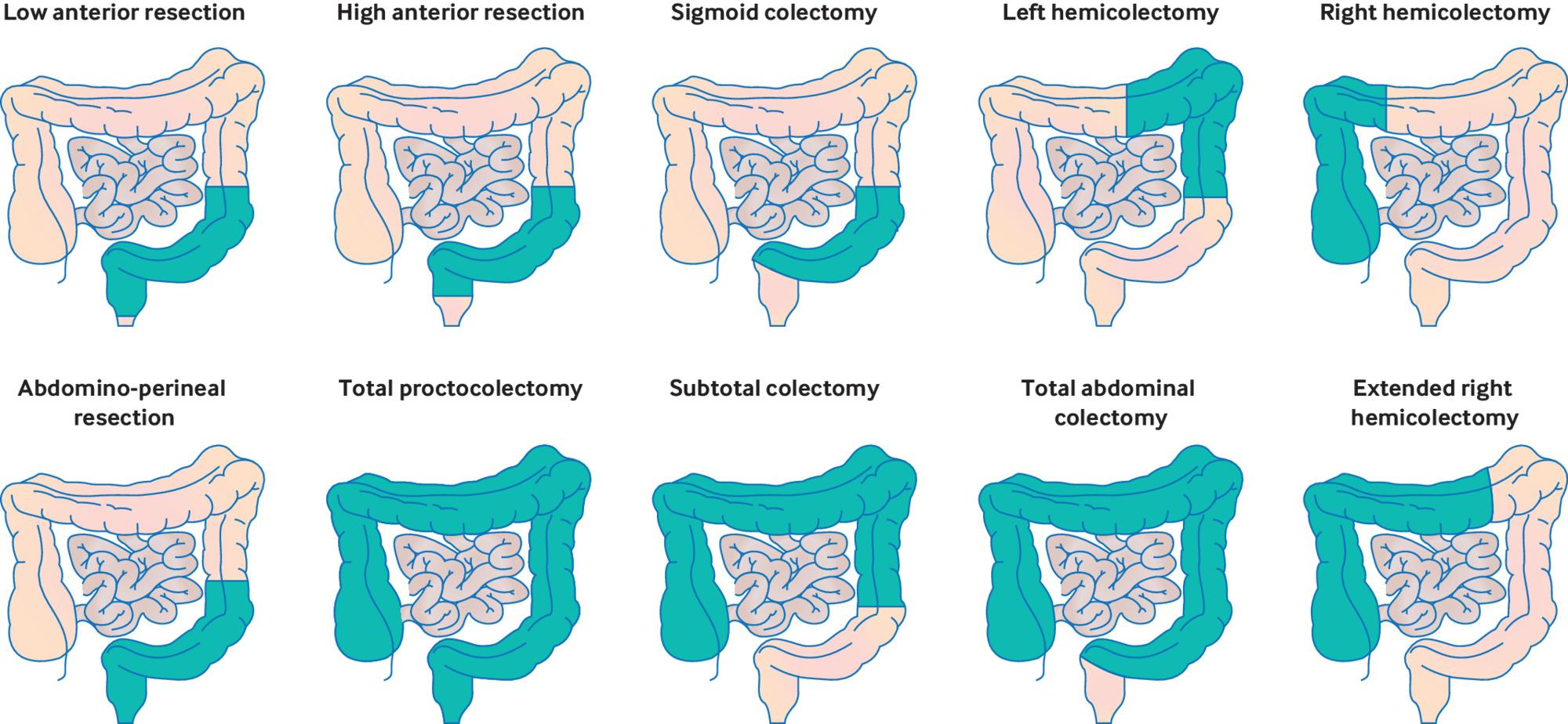
Polyps and in situ cancers (Stage 0) can often be removed during a colonoscopy. If a biopsy shows the cancer has not spread elsewhere then only a routine follow-up is needed.
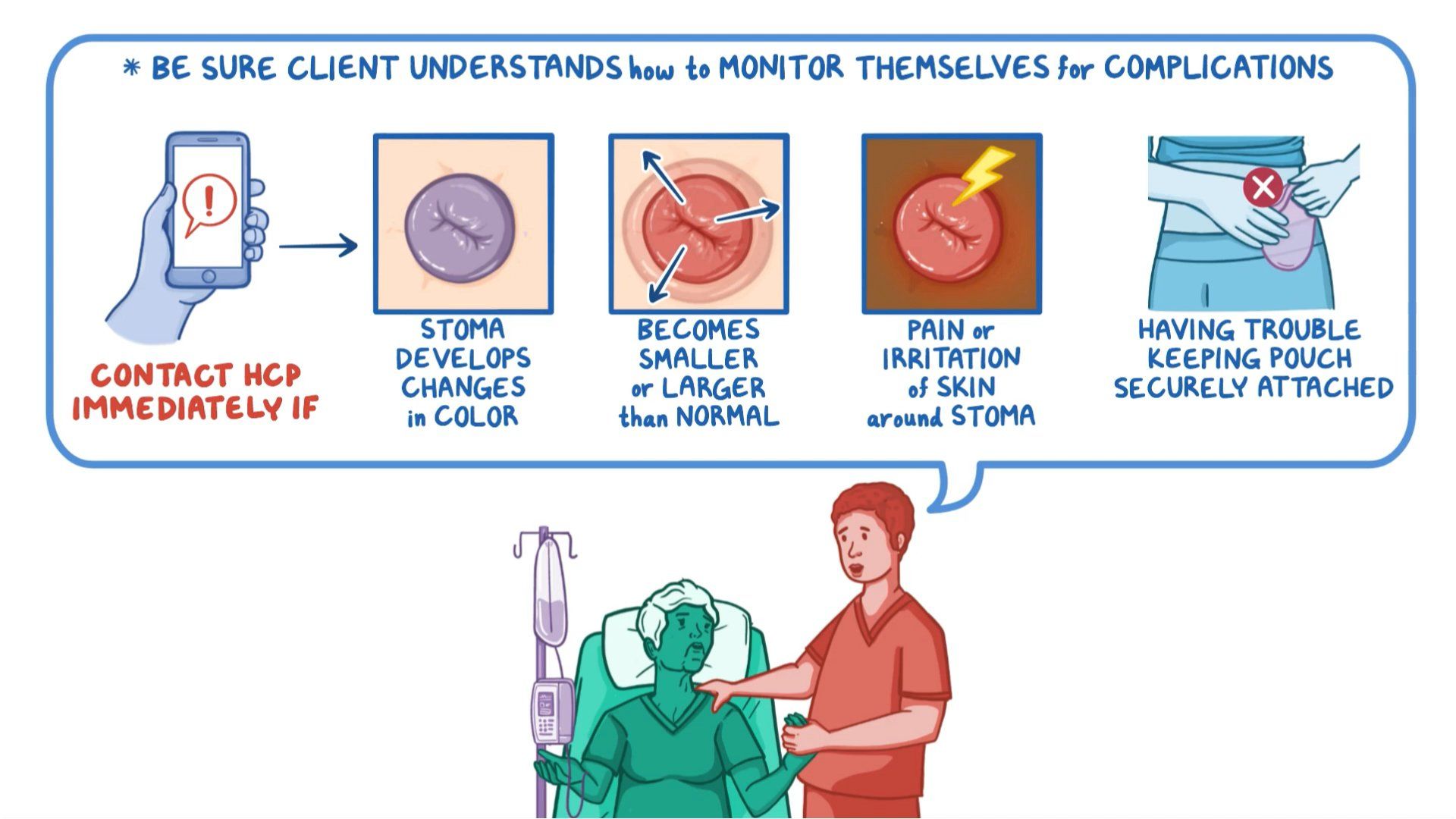
For more advanced bowel cancer (Stages I to III), surgery usually involves removing the cancerous portion of the bowel, some nearby tissue, and joining the remaining ends of the bowel together. If the 2 ends of the bowel can’t be reconnected, the surgeon will create an opening to the outside of the body, known as a stoma, from which waste can leave the body. This is known as resection with colostomy.
Radiotherapy
Radiotherapy involves destroying the cancer cells with radiation. It may be combined with bowel surgery.
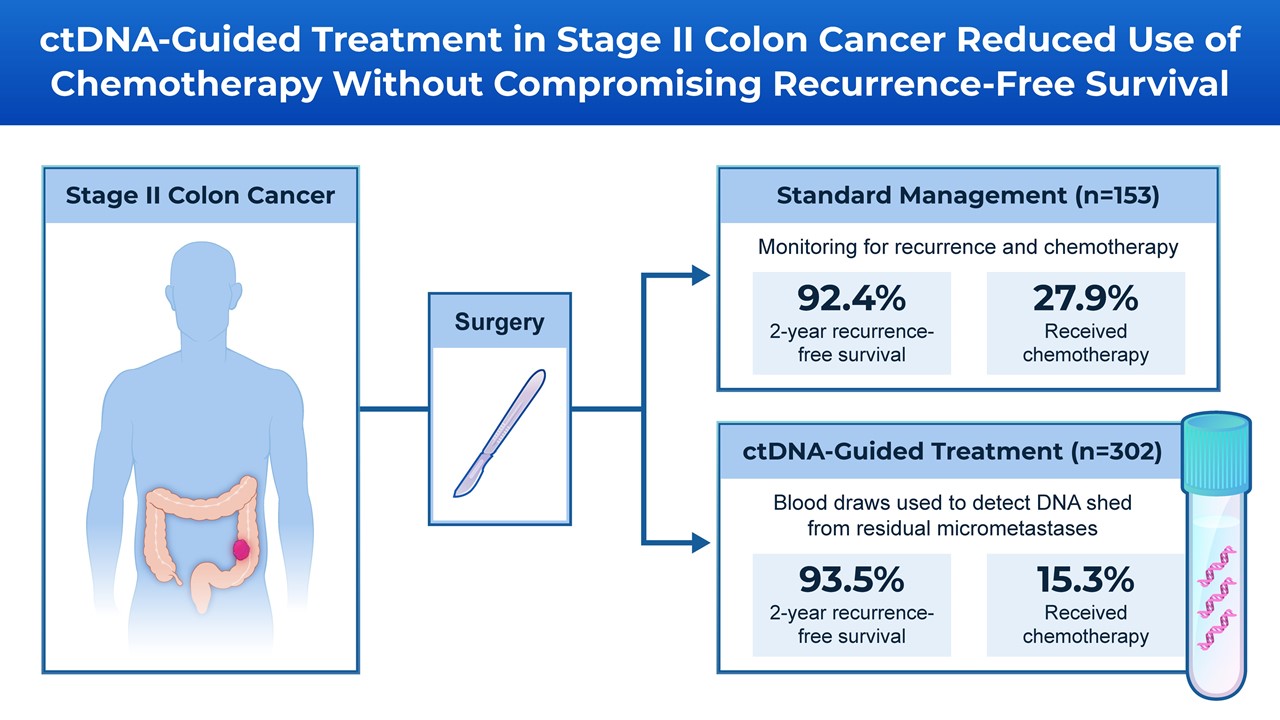
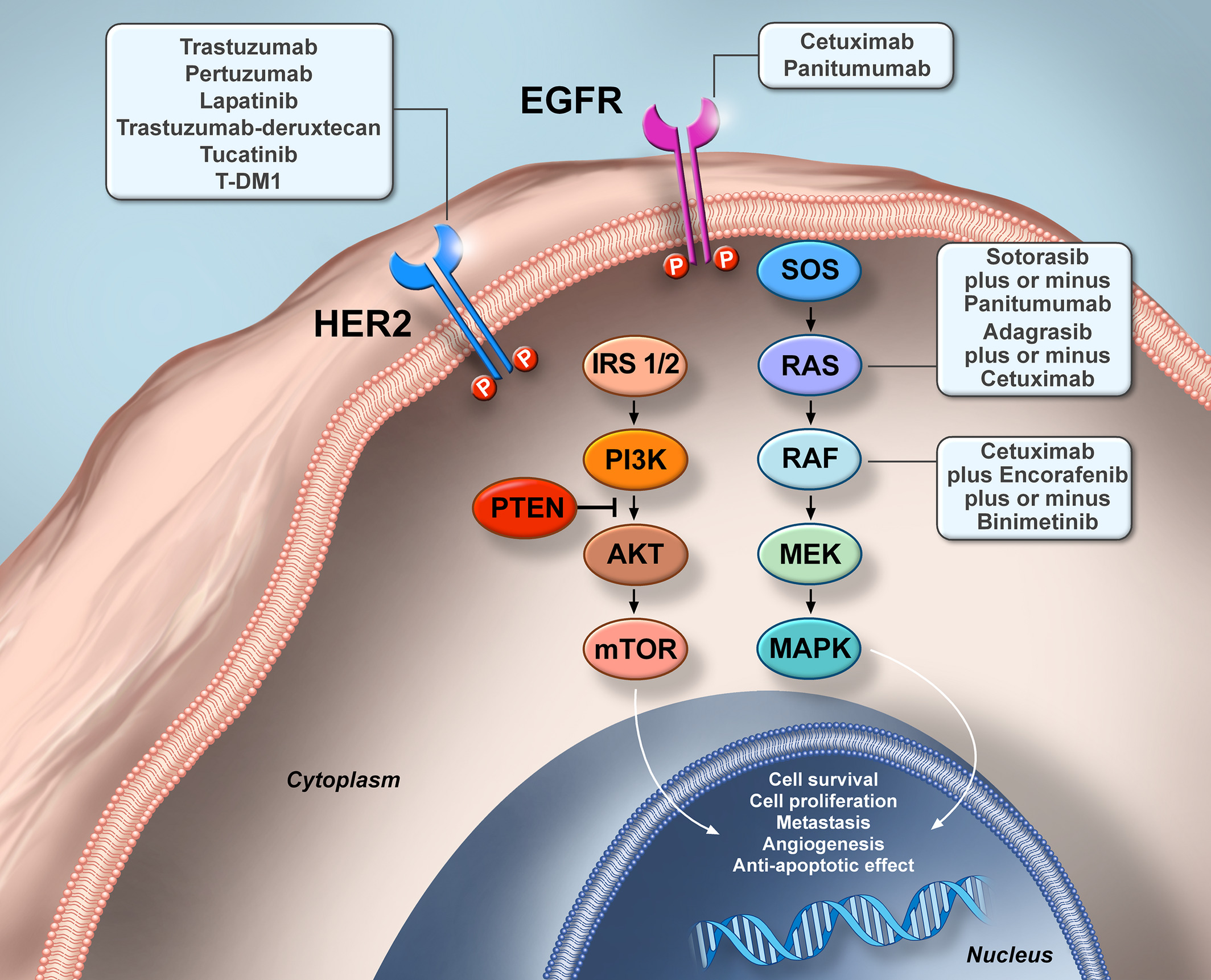
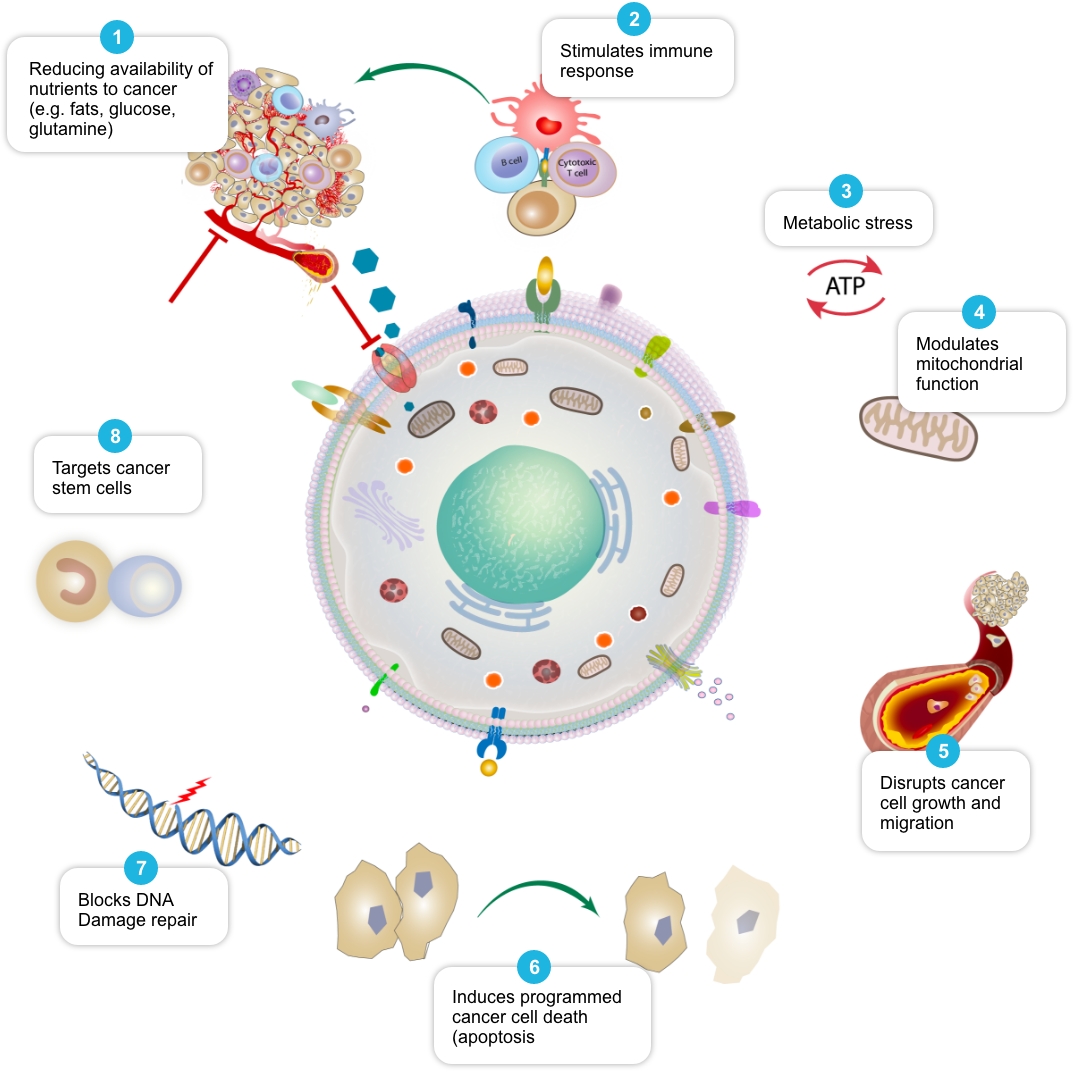
Chemotherapy
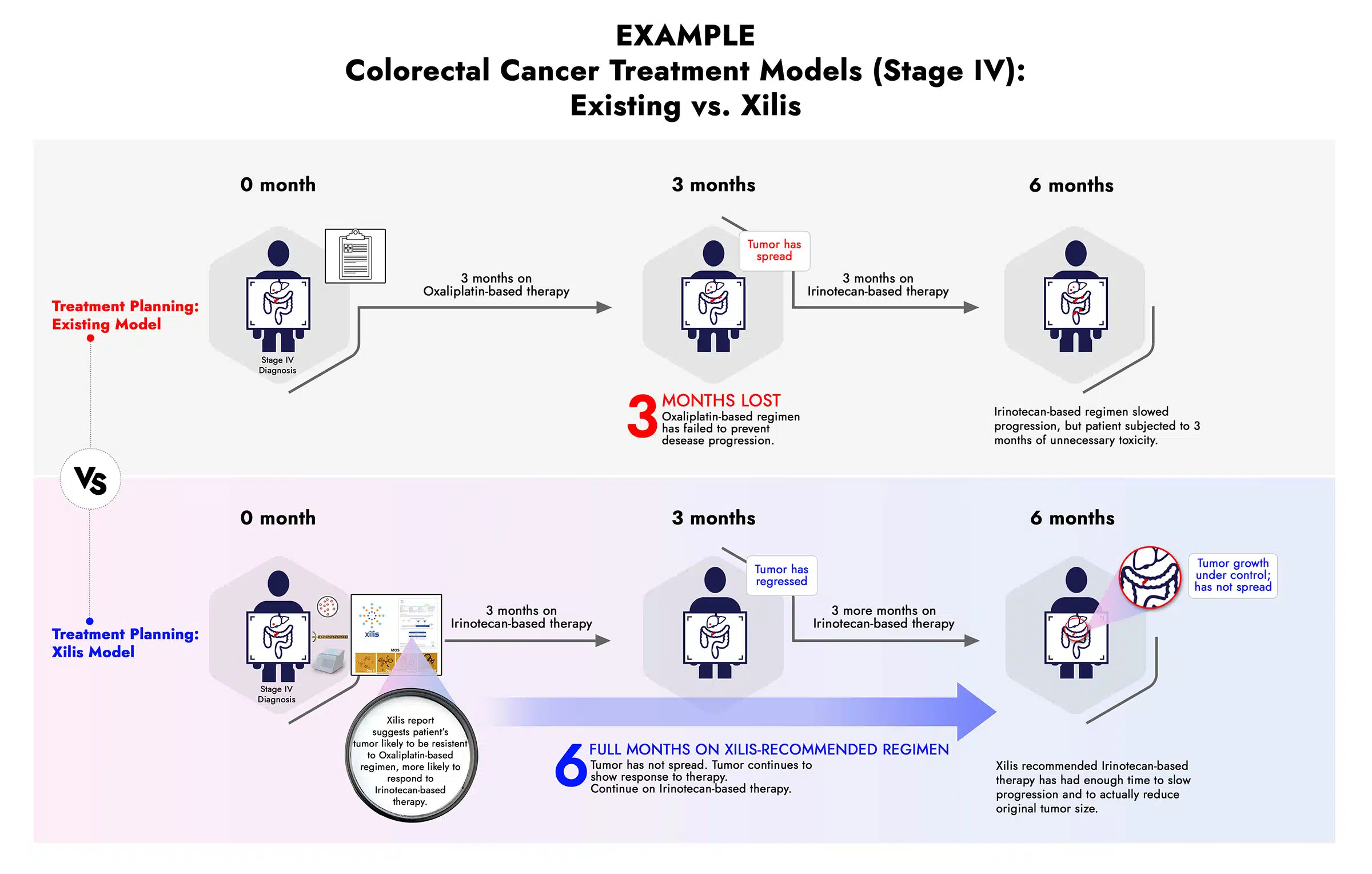
Chemotherapy uses anti-cancer drugs to kill cancer cells in the body. It may be used to remove cancers that have spread elsewhere in the body, before surgery to shrink tumours, after surgery to get rid of cancer that was not removed during the surgery, or if it’s not possible to perform surgery.
Can bowel cancer be prevented?
While there’s no way to prevent bowel cancer completely, several diet and lifestyle choices can lower your bowel cancer risk:
- Keep physically active for at least 30 minutes each day.
- Reduce alcohol intake to no more than 2 standard drinks per day, or avoid it altogether.
- Include dairy products such as low-fat milk, yoghurt and cheese in your daily diet, with at least 2 serves per day.
- Include wholegrains and fibre, such as brown rice, wholemeal bread, vegetables, fruits, beans and nuts.
- Limit red meat consumption to 500 grams cooked per week and avoid processed meat altogether.
- Quit smoking and avoid breathing in tobacco smoke.
Are there complications of bowel cancer?
Possible complications after bowel surgery include:
- an infection following surgery
- difficulty eating or drinking
- constipation, diarrhoea and other bowel problems
- pain, swelling or unexpected leakage from your wound or stoma
- leaking faeces
In addition, living with a stoma can be challenging and if you have one, you may need extra support.
In some cases, bowel cancer may recur in the bowel or elsewhere in the body. Secondary cancer may develop in the liver, lungs or elsewhere.