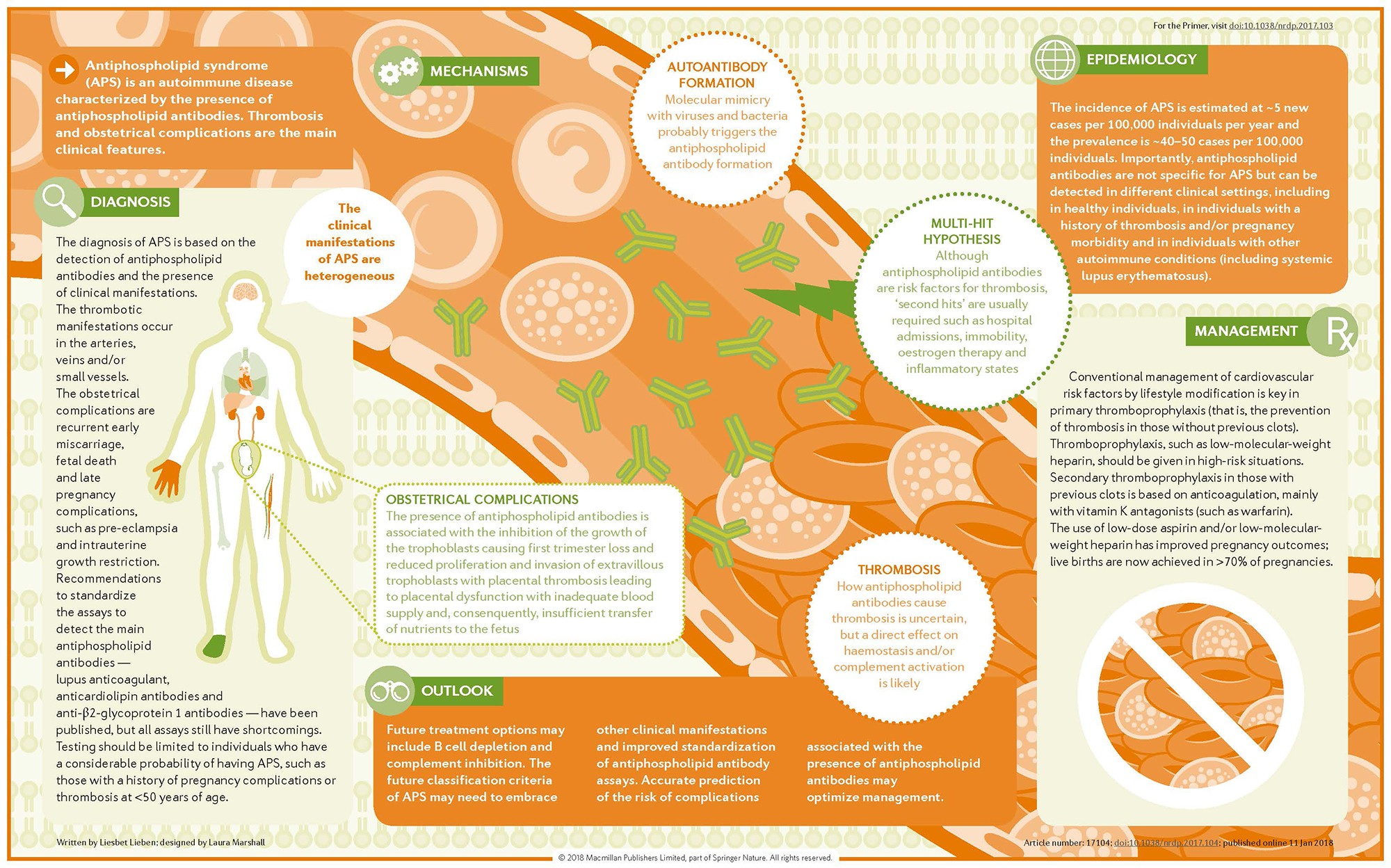
Antiphospholipid syndrome (APS) is a blood disorder that puts a person at greater risk of developing blood clots or having problems with pregnancy. It is sometimes called Hughes syndrome or sticky blood. With treatment, most people with APS can lead normal lives.
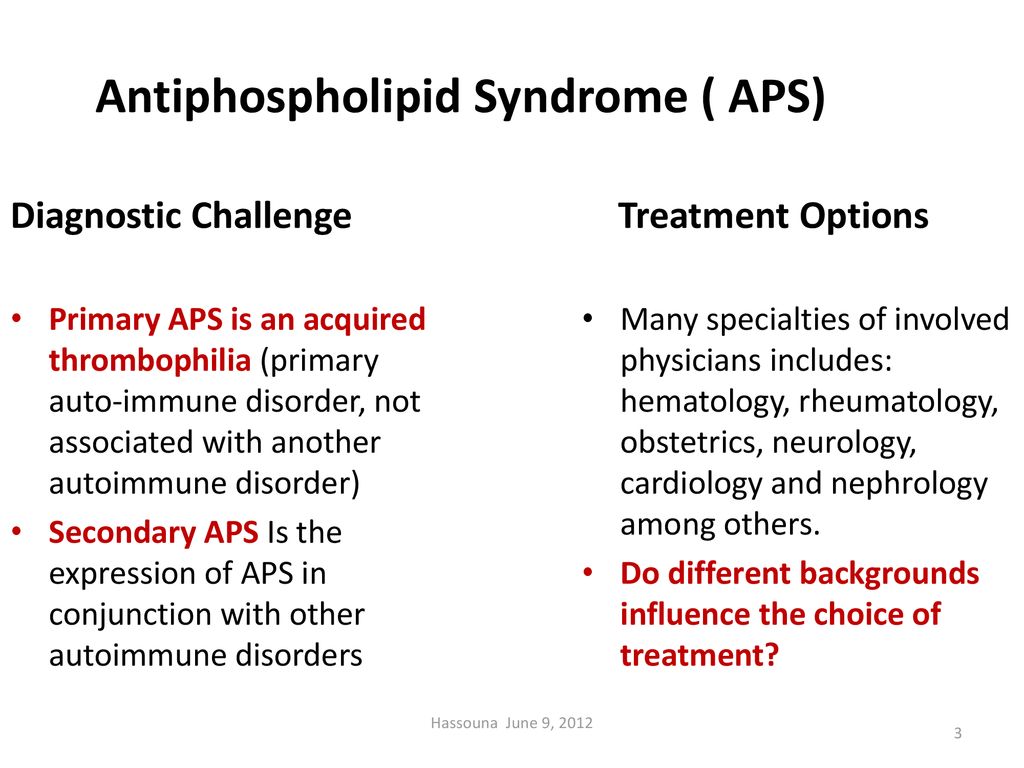
Types of APS
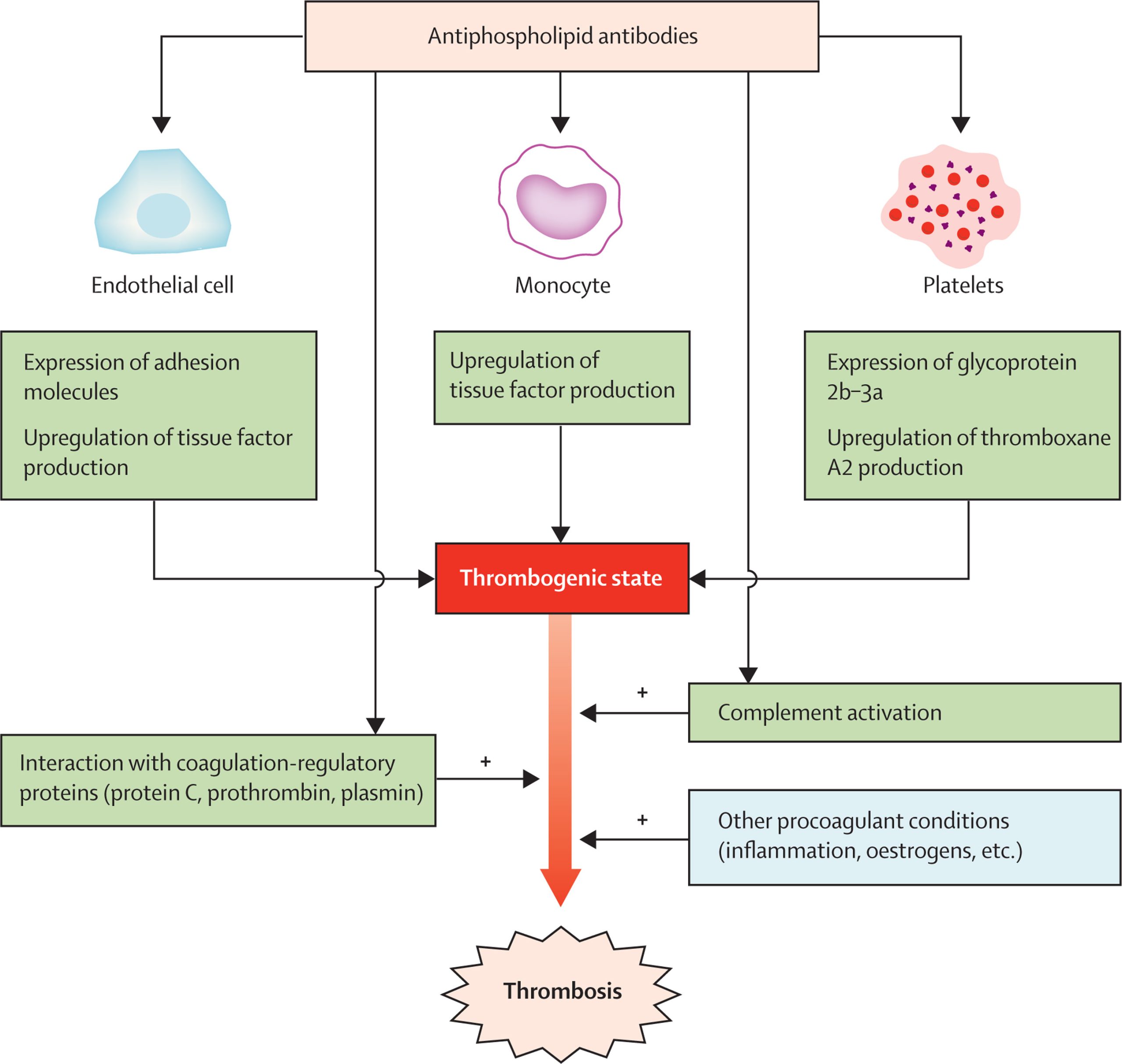
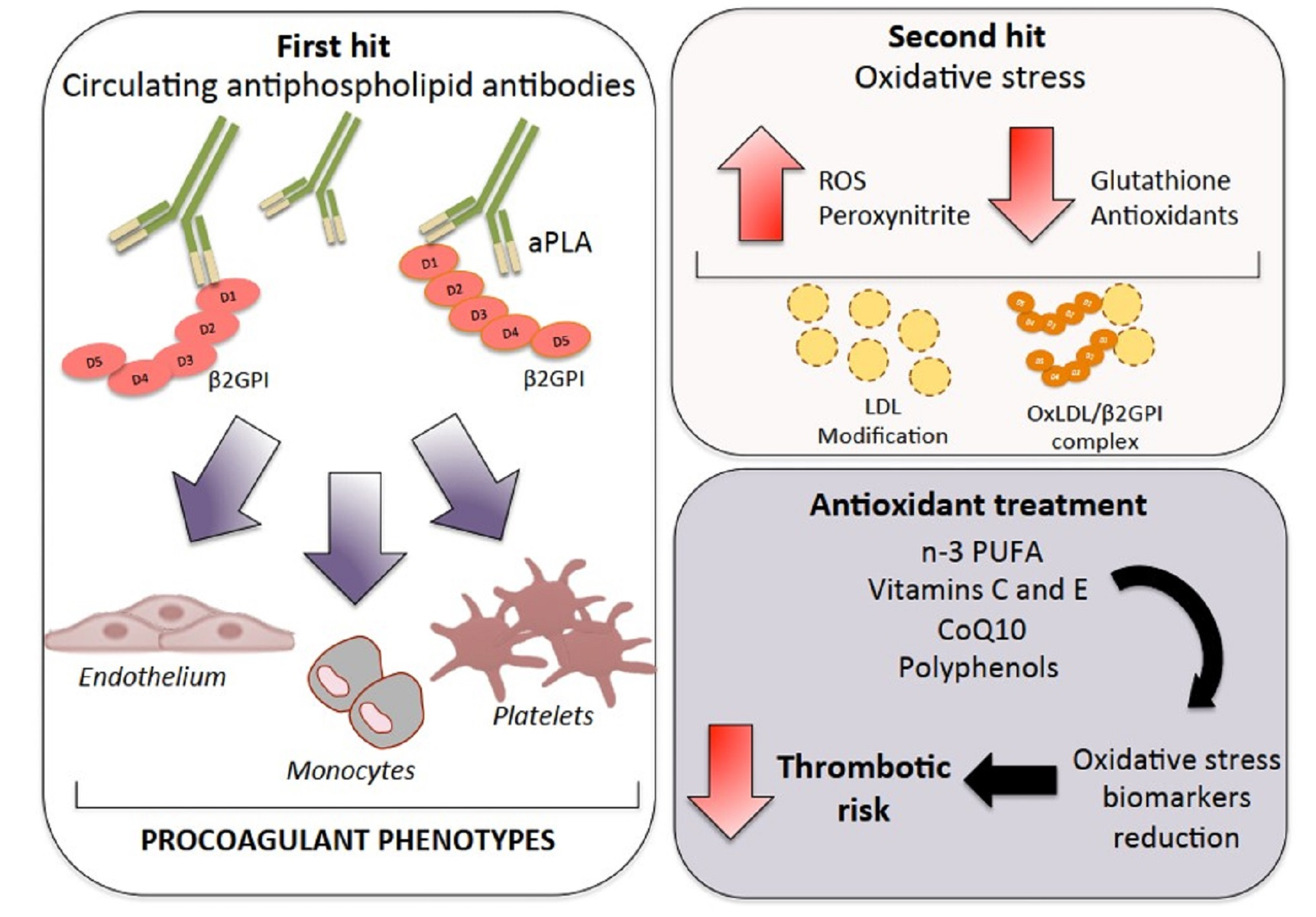
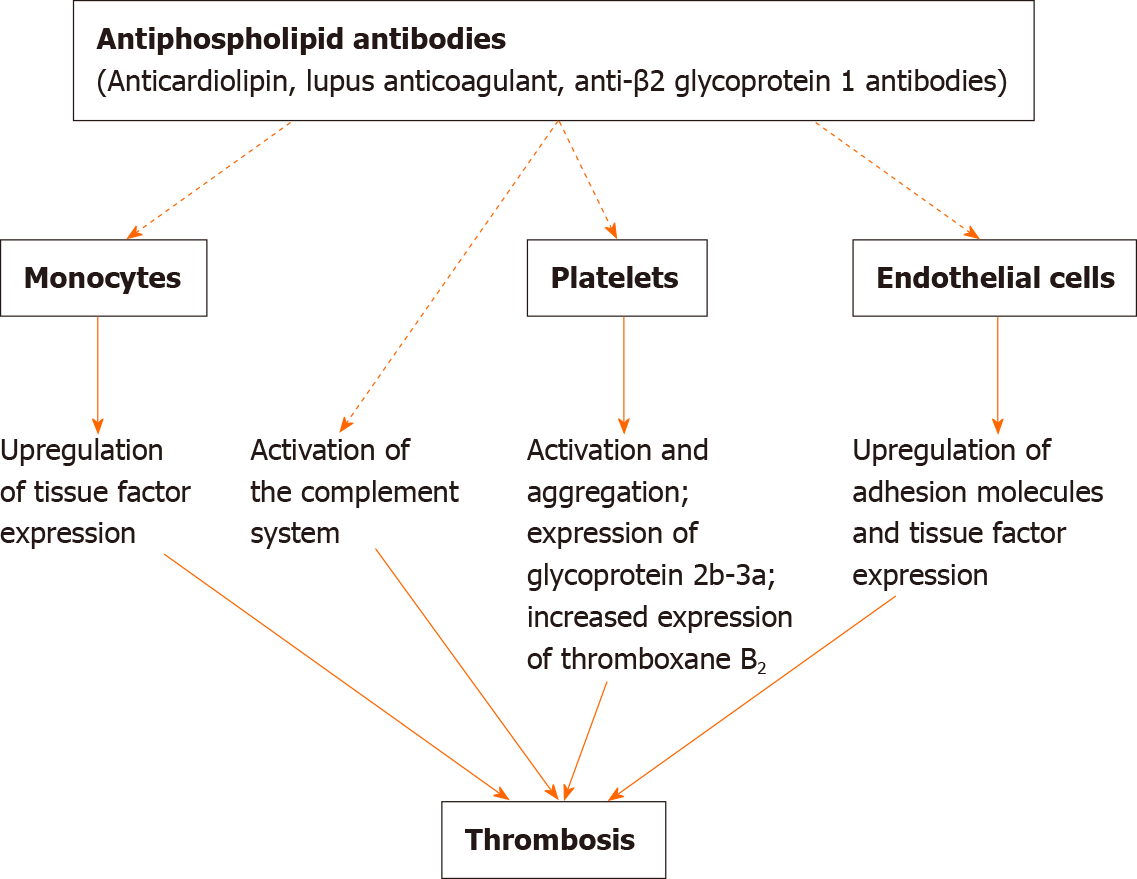
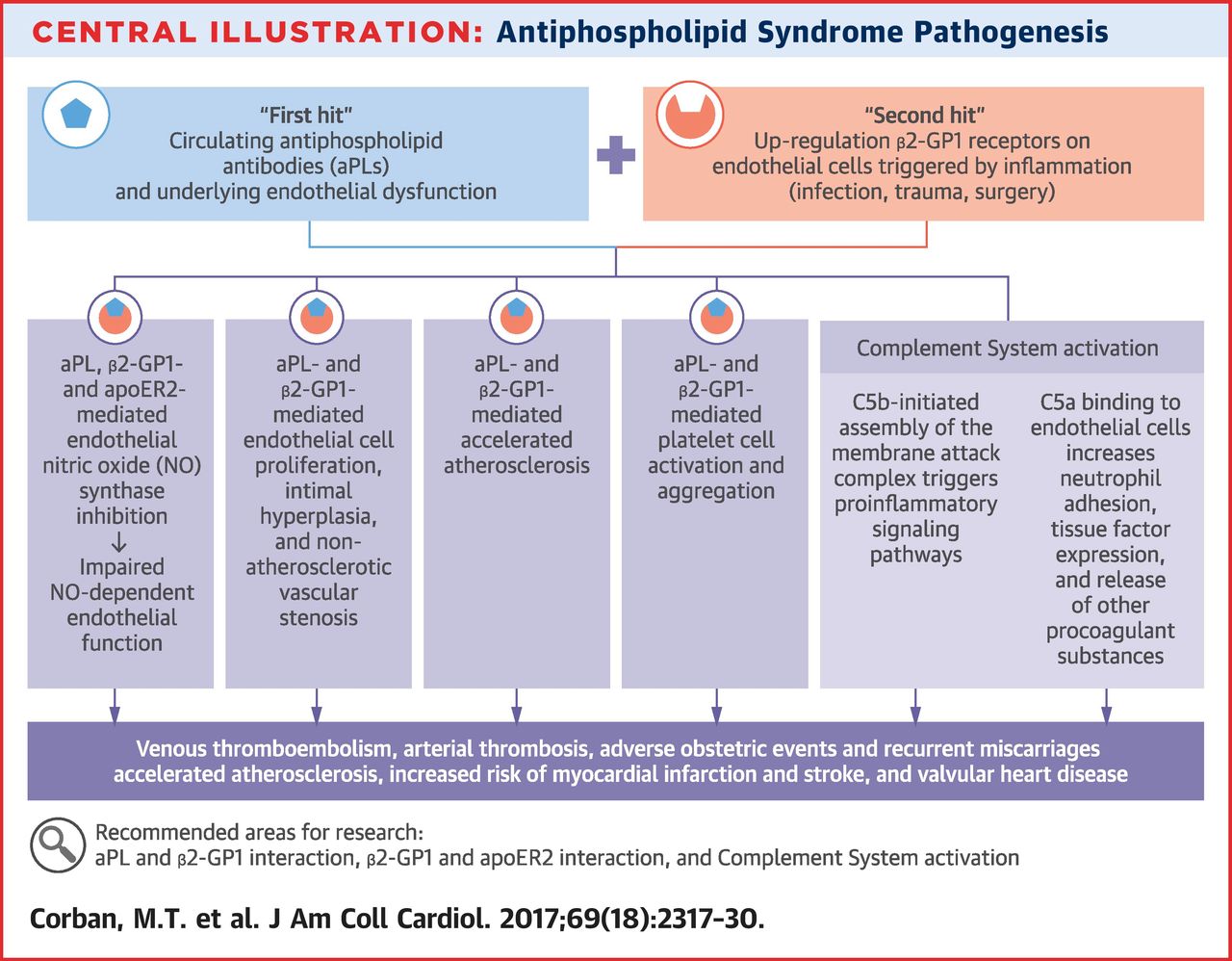
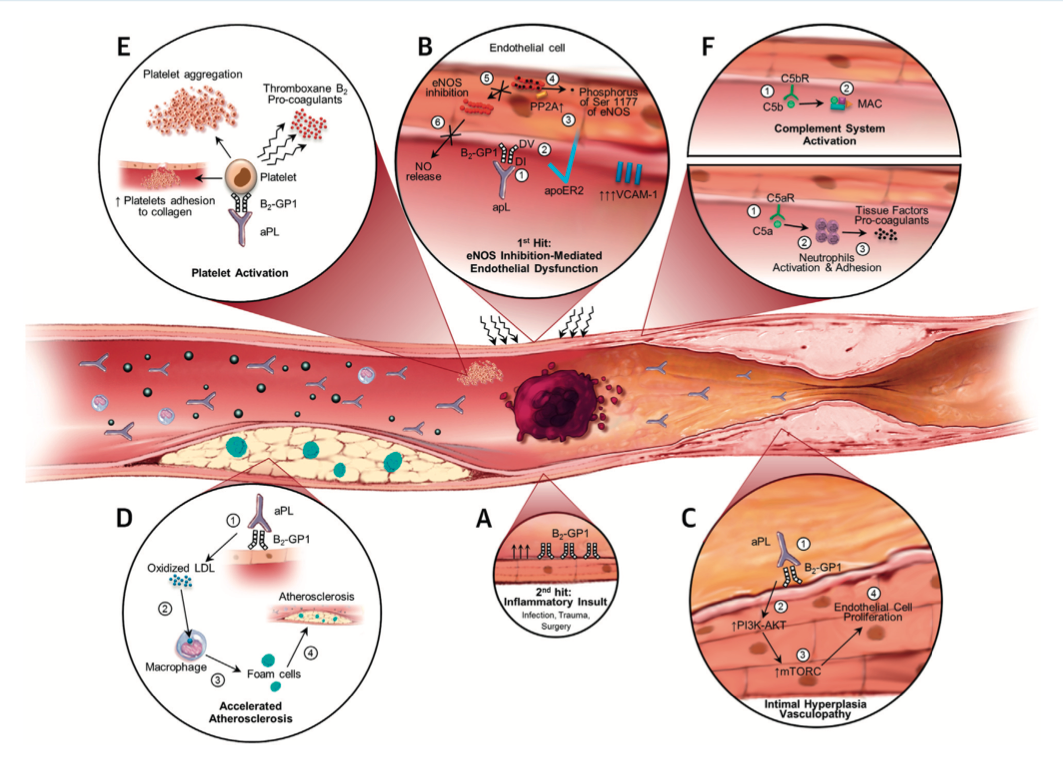
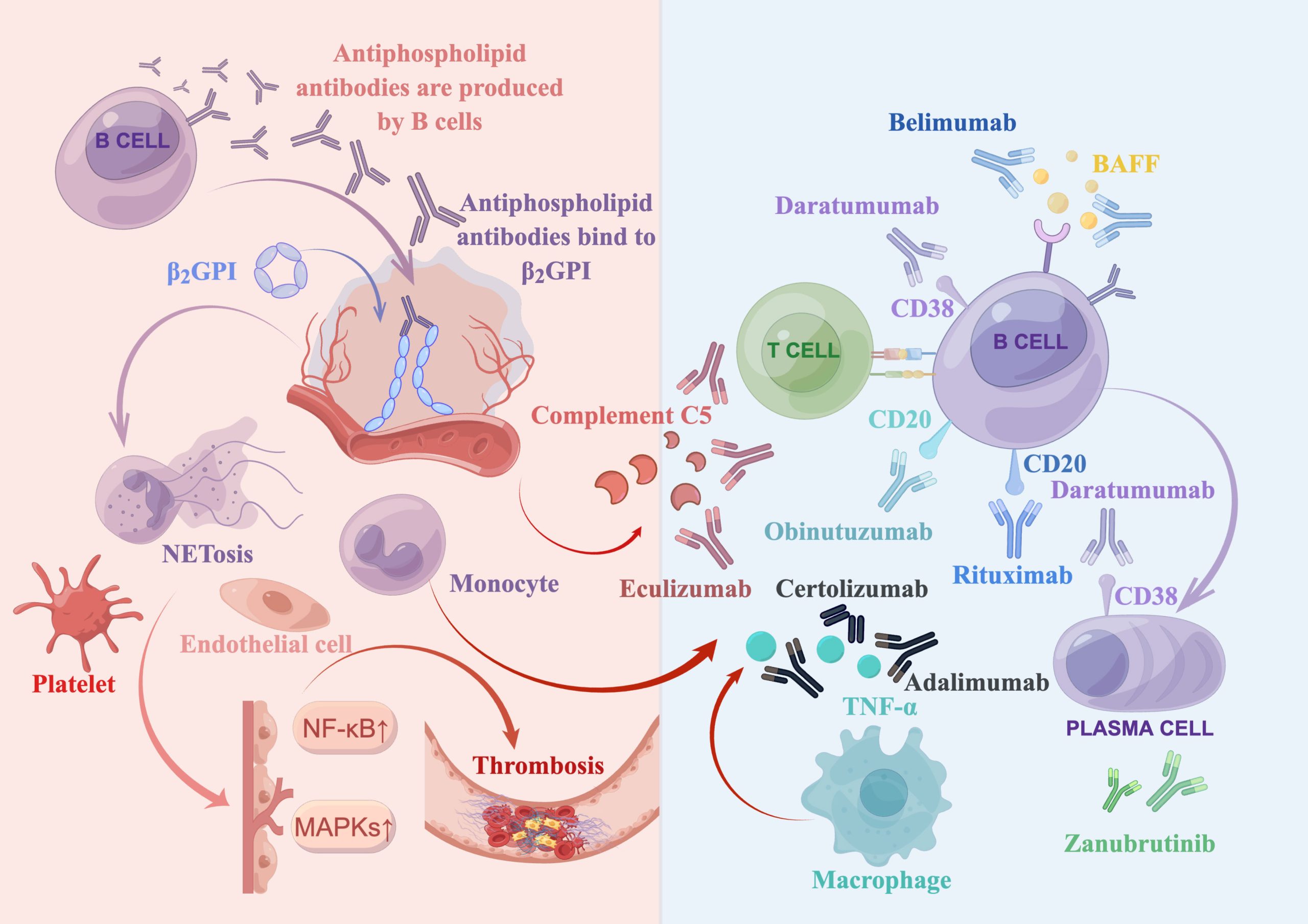
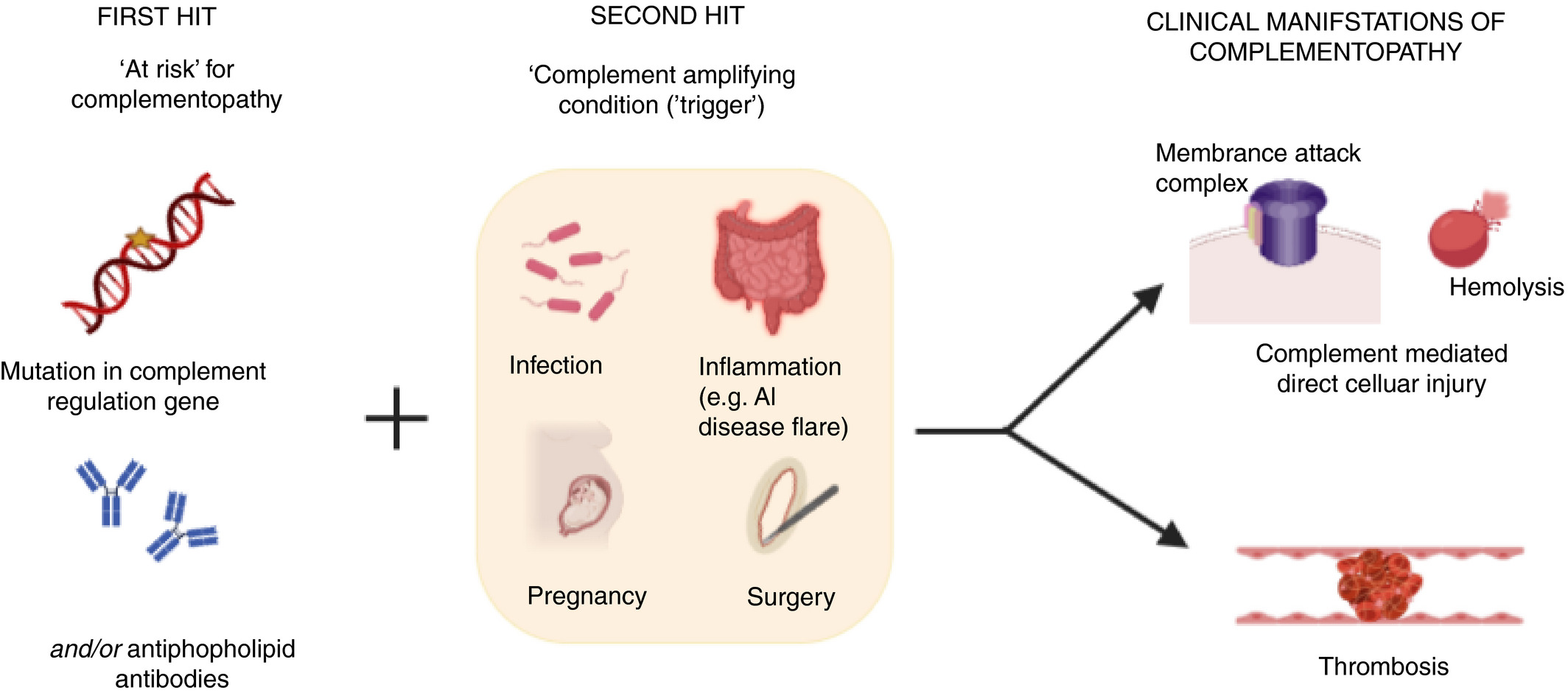
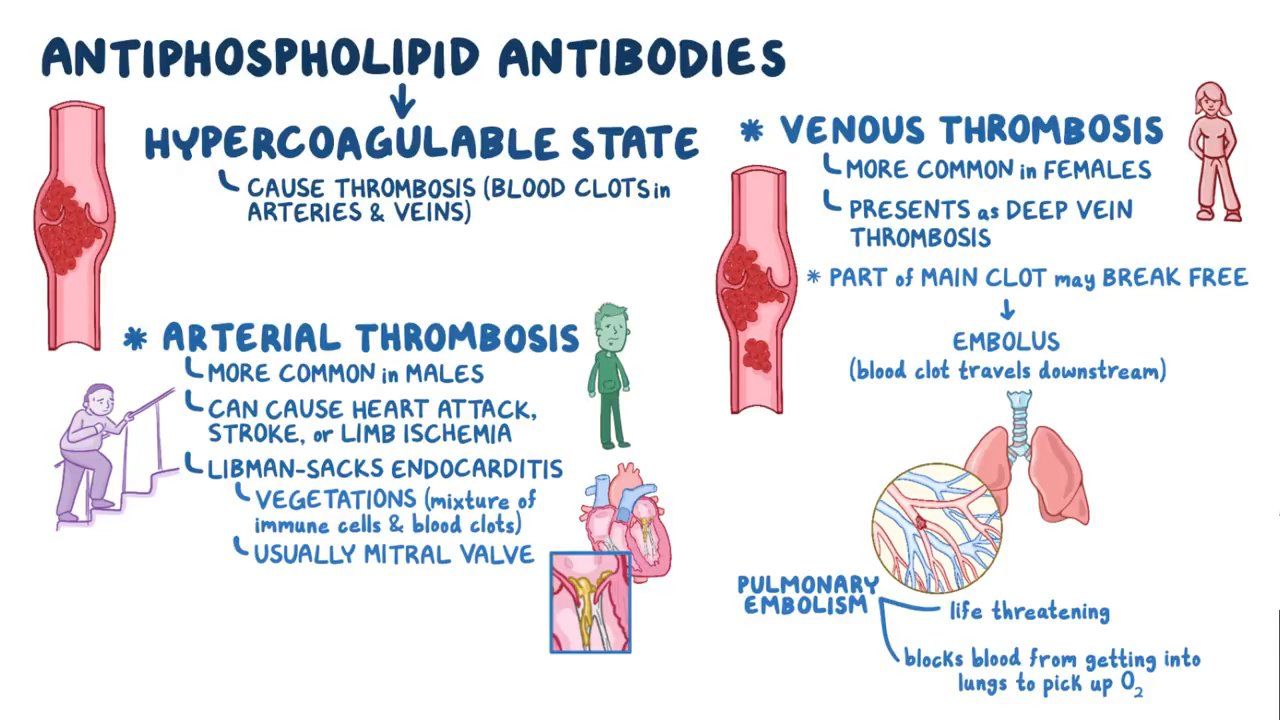
APS develops when someone has abnormal antibodies in their blood. It is an autoimmune disorder, meaning the antibodies the body produces to fight infections start attacking the body instead.
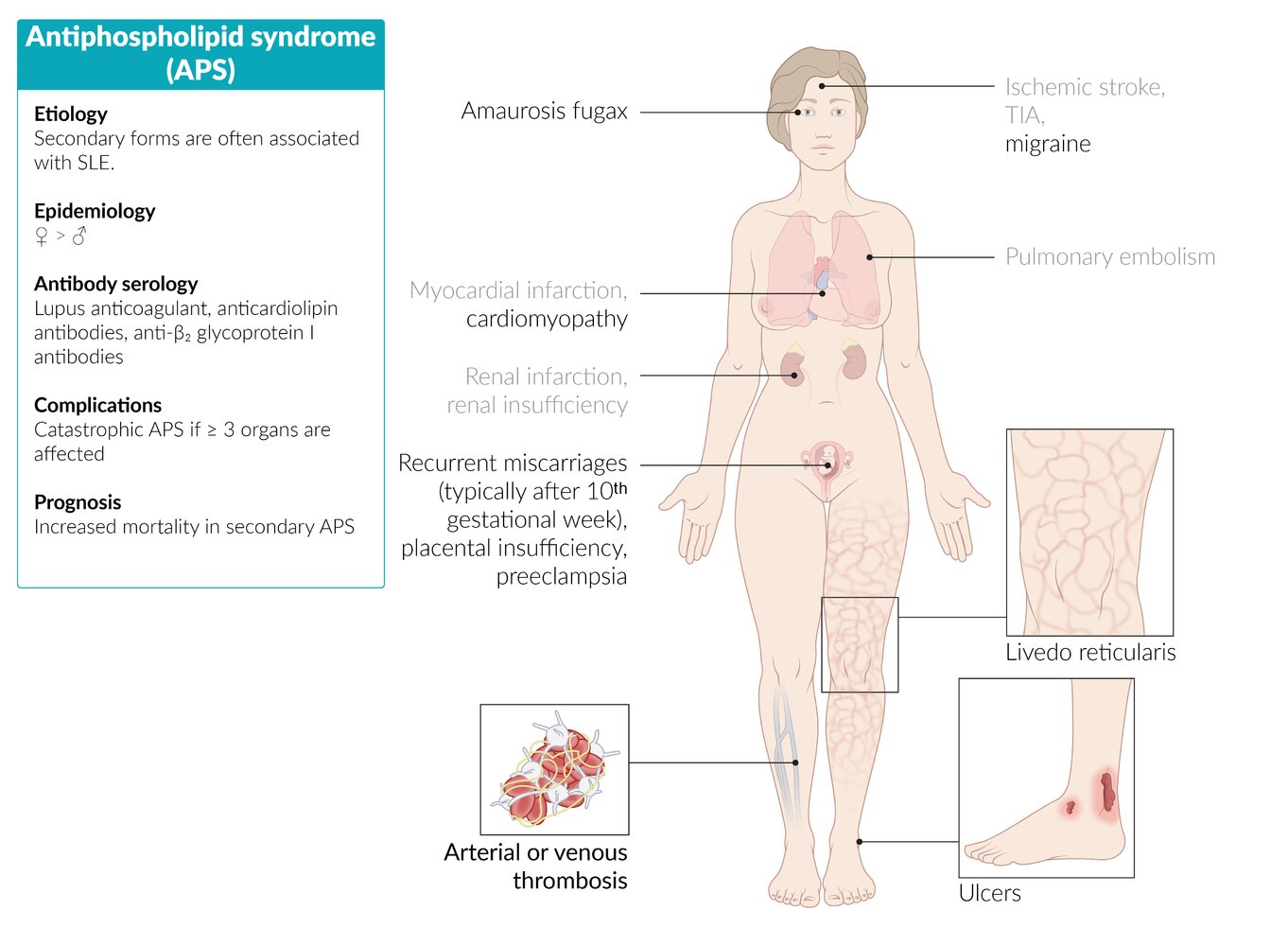
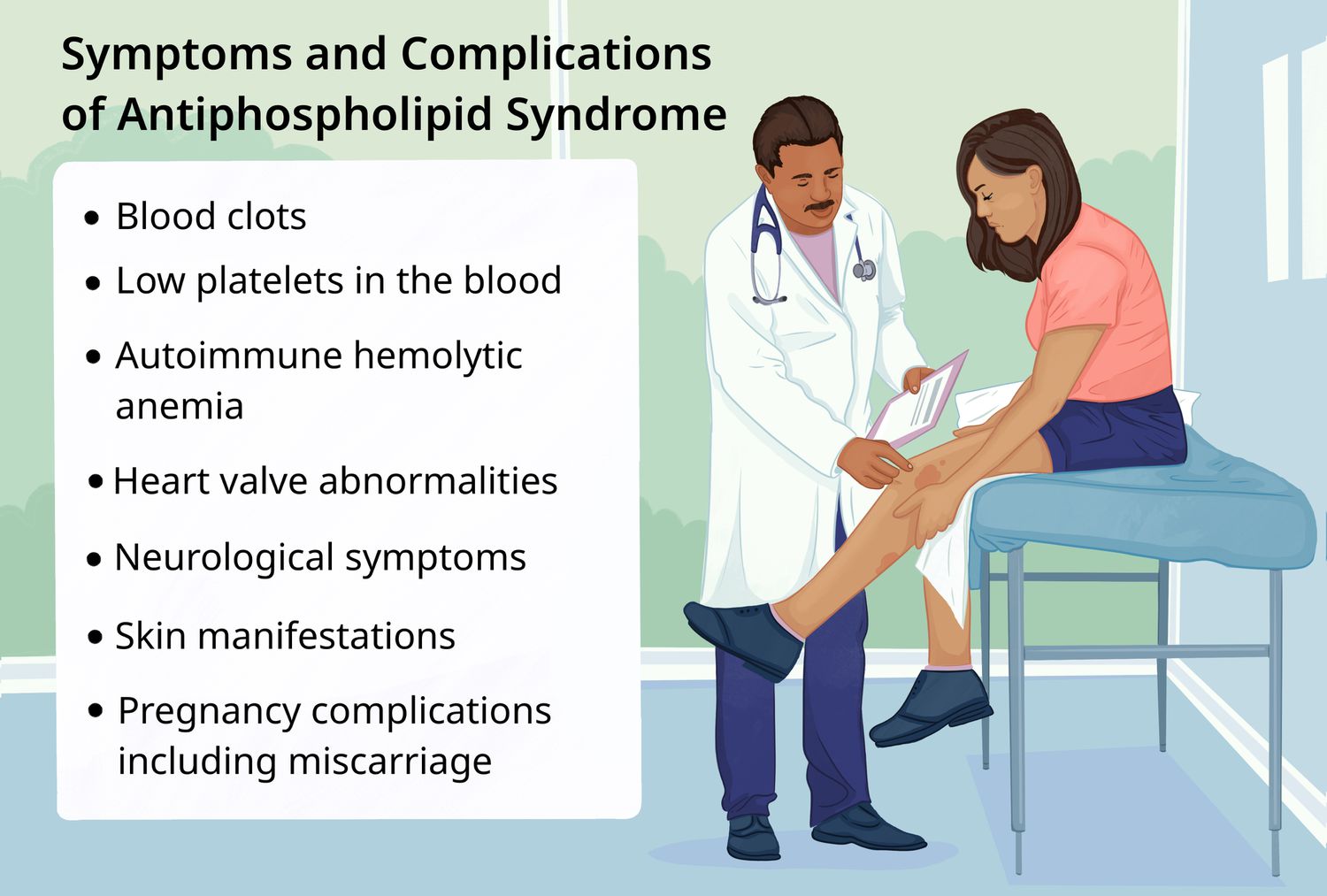
Blood clots can cause serious problems, such as deep vein thrombosis (DVT) in the legs, or damage to organs, such as your kidneys, lungs or brain.
Causes of APS
People with APS may also have lupus or an infection such as HIV/AIDS or Q Fever. It can sometimes be caused by taking some medicines. APS affects more women than men.
APS symptoms
Symptoms depend on where the blood clots form and where they travel through the veins. Blood clots due to APS can cause:
- DVT: Symptoms include pain or swelling in the calf or thigh.
- Pulmonary embolism (PE): A blood clot forms in an artery that feeds the lung — symptoms include chest pain and shortness of breath.
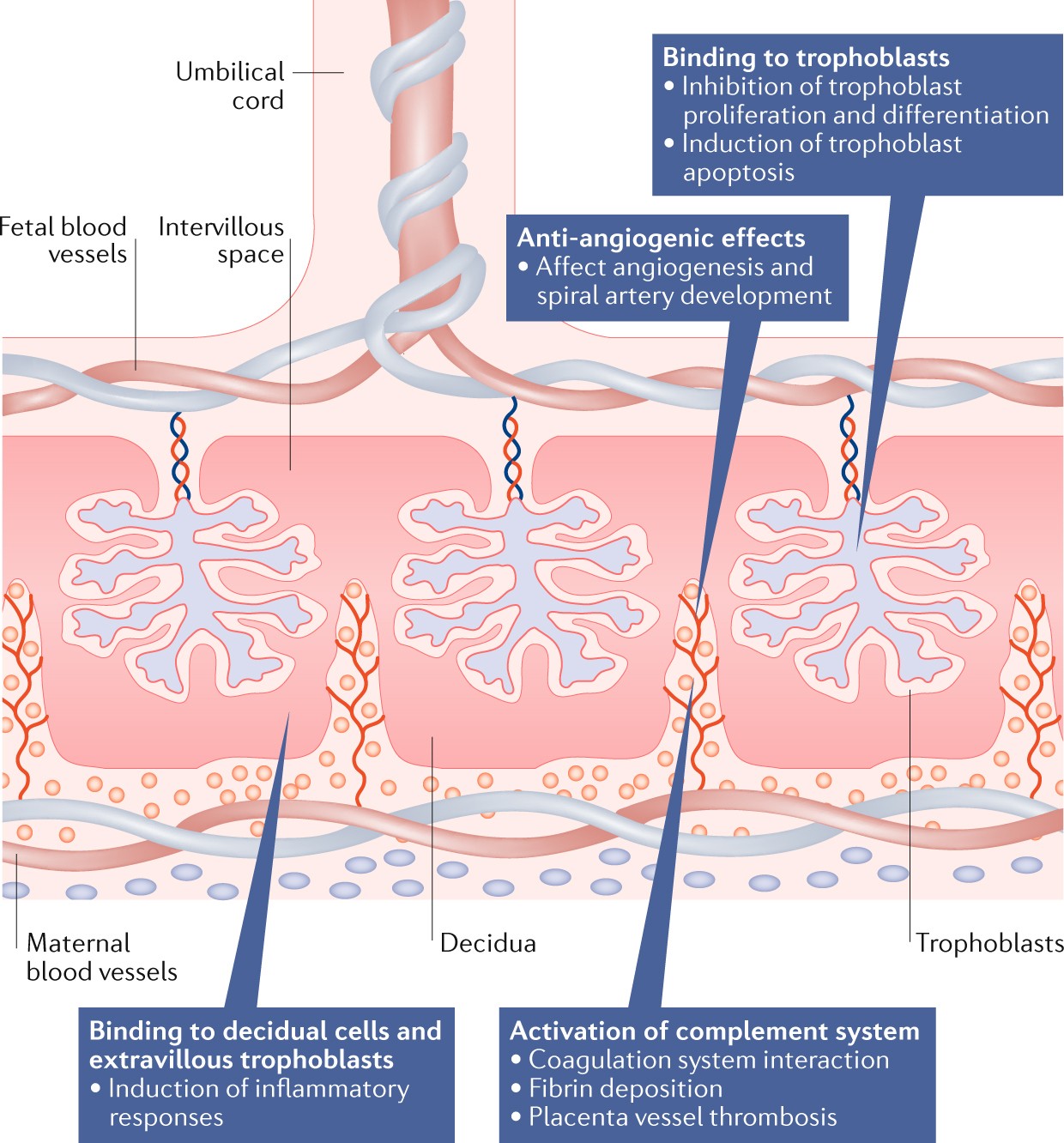
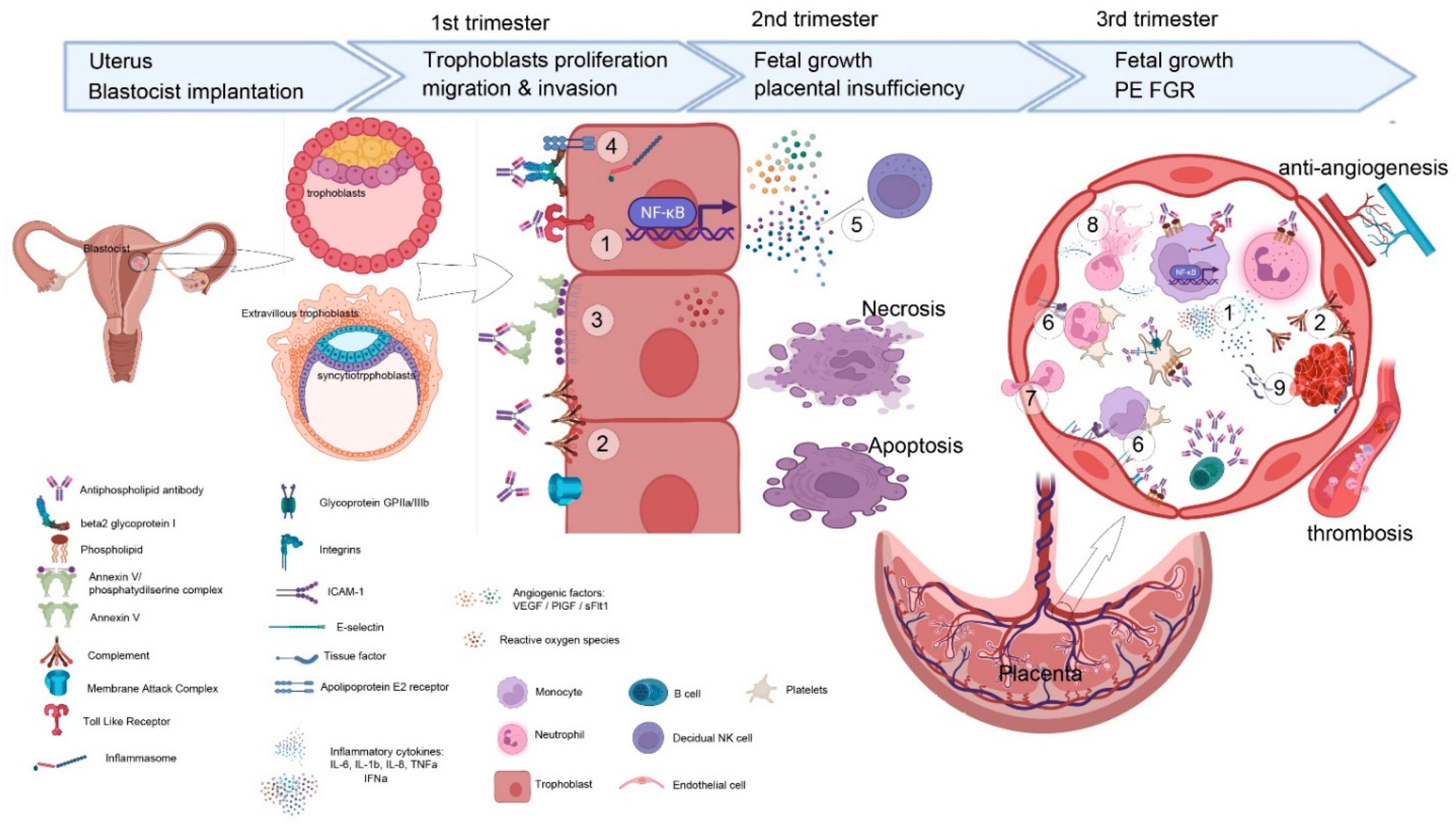
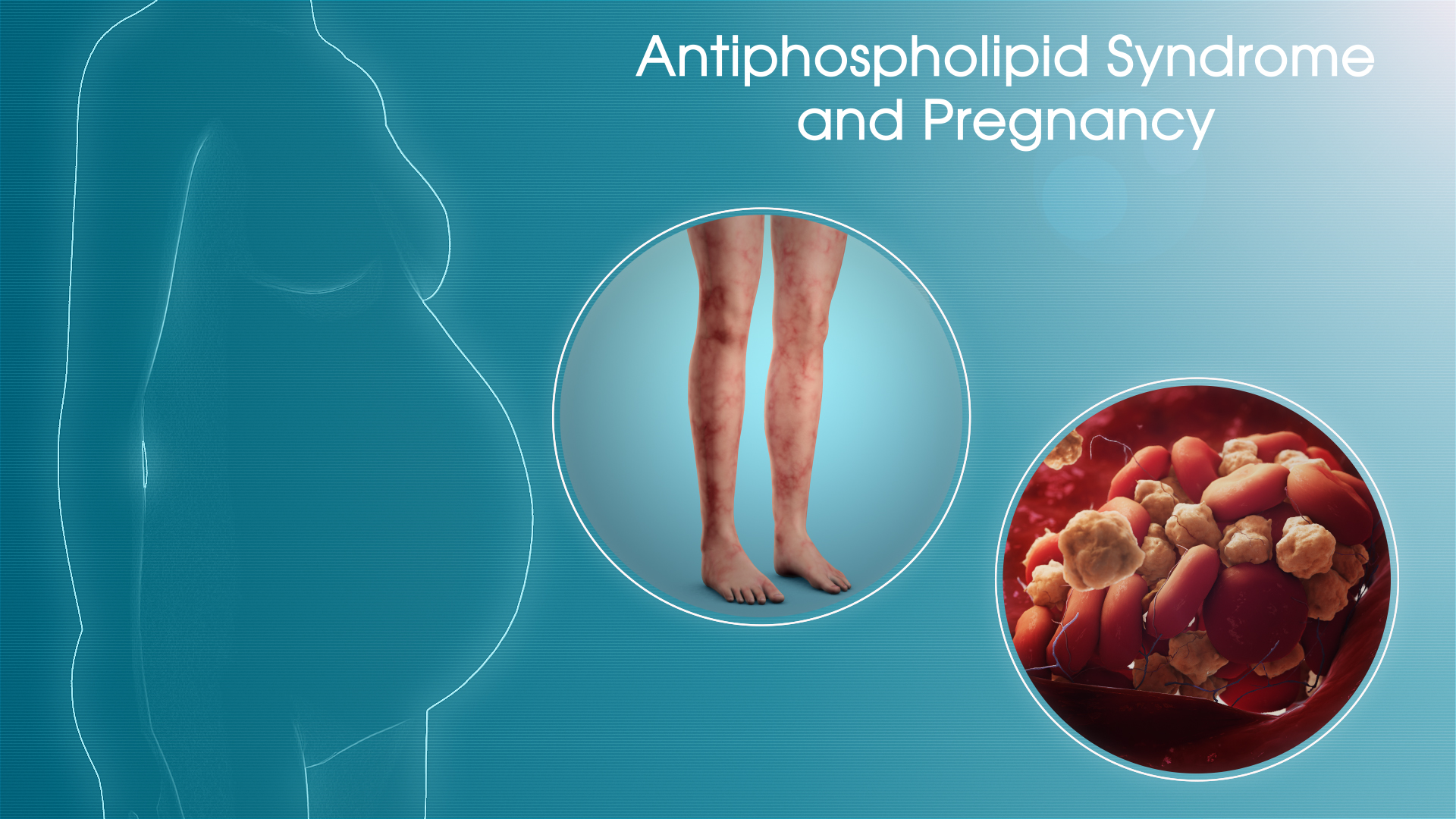
- Problems with pregnancy: APS can cause miscarriages, preterm delivery or pre-eclampsia.
- Ischemic stroke: A blood clot can cut off blood supply to the brain, causing a stroke.
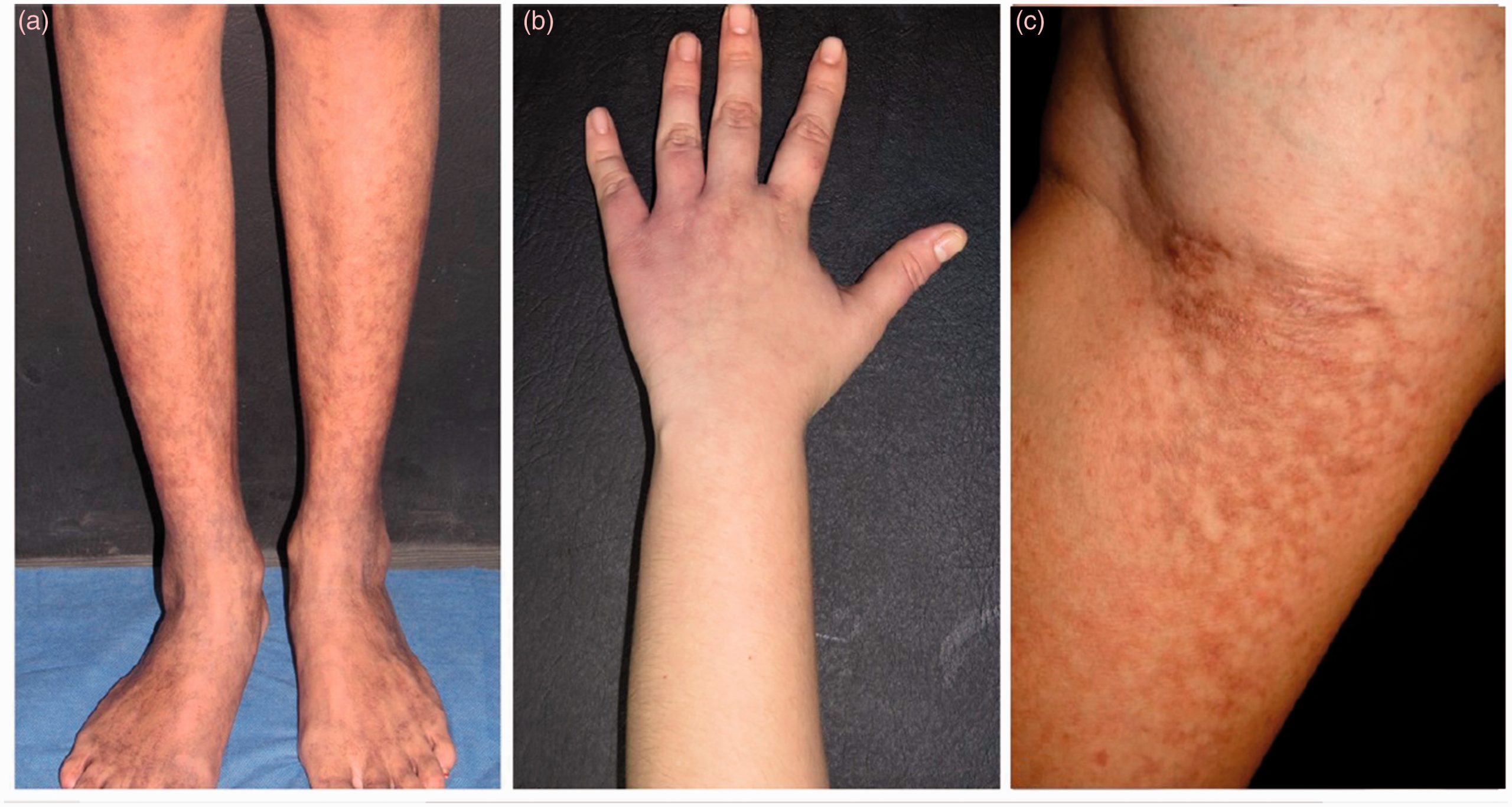
Some people with APS will also have problems such as an abnormal heart valve or too few platelets in their blood, which can cause bleeding. Some also develop headaches, seizures or a lacey red rash on their knees and wrists known as livedo reticularis.
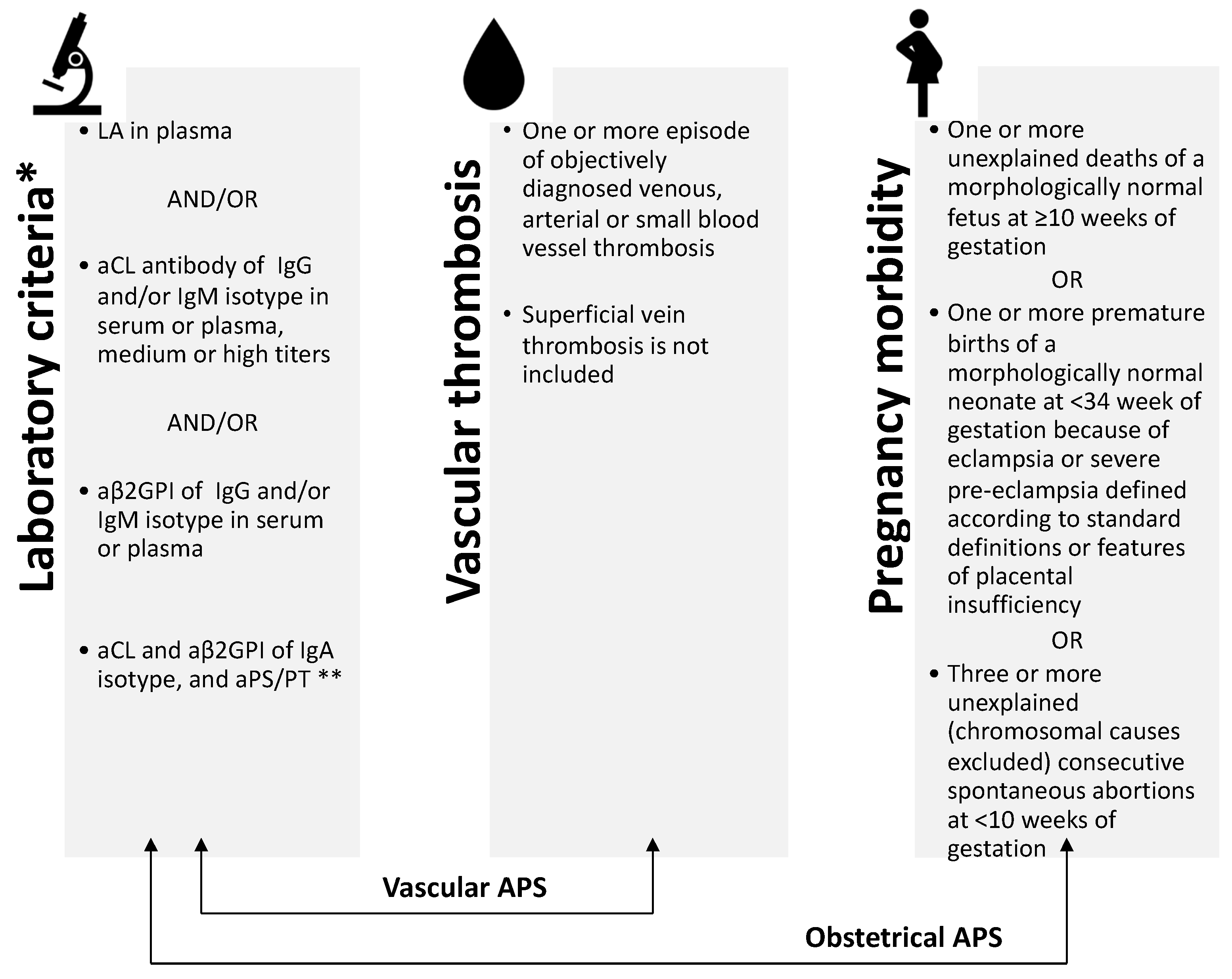
APS diagnosis
APS is usually discovered if someone has repeated blood clots or miscarriages that can’t be explained by something else.
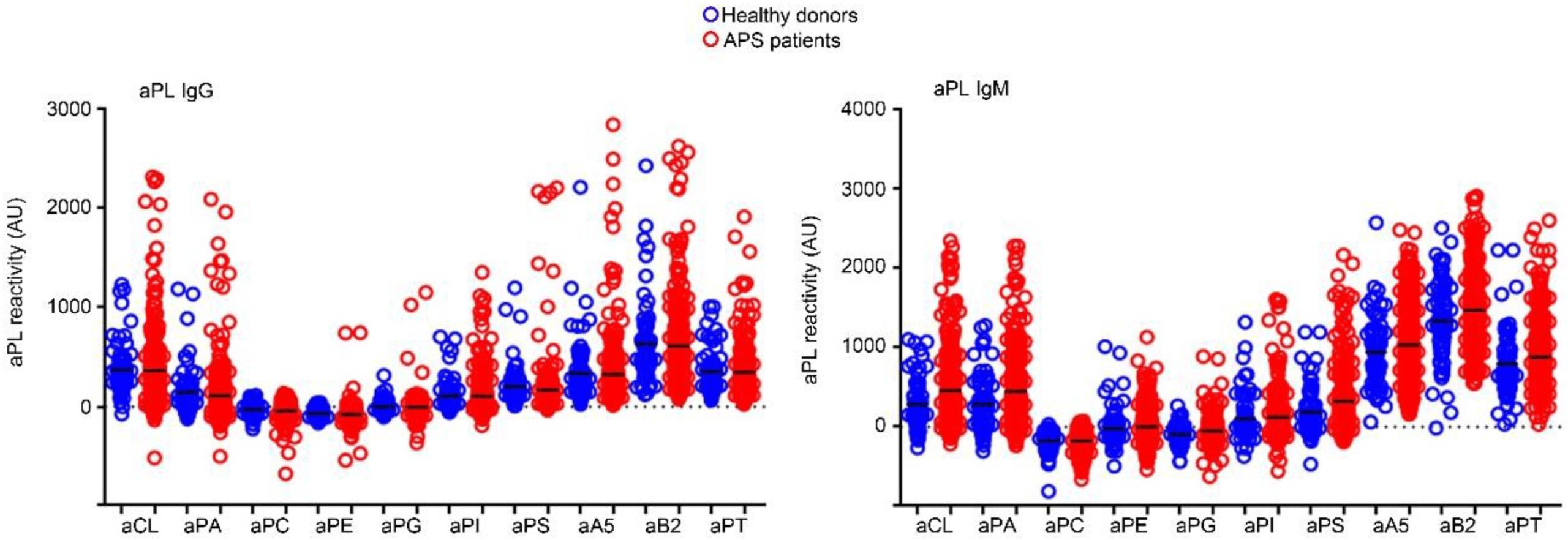
It is diagnosed by using blood tests to check how the blood is clotting and whether there are any of the abnormal antibodies.
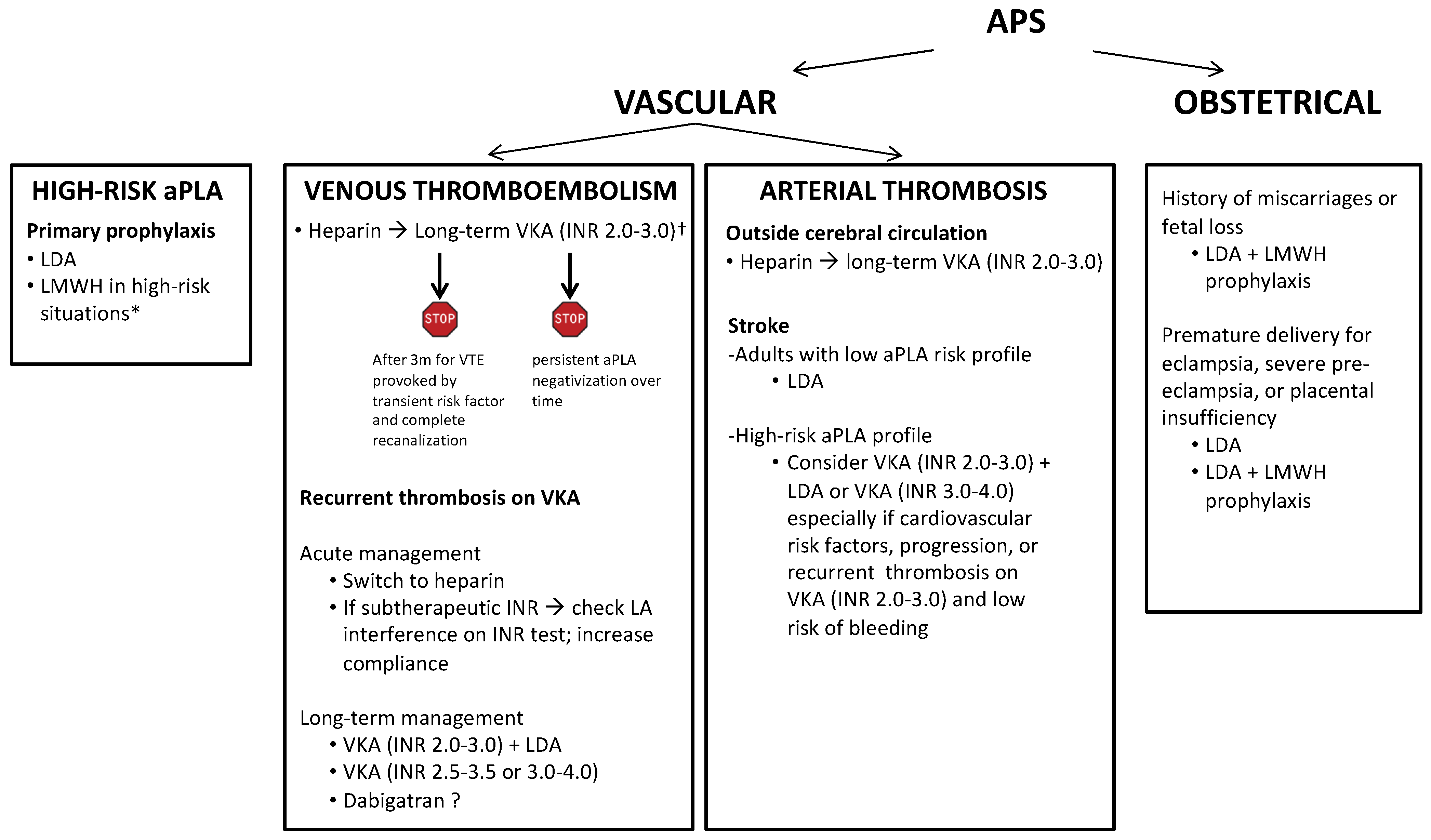
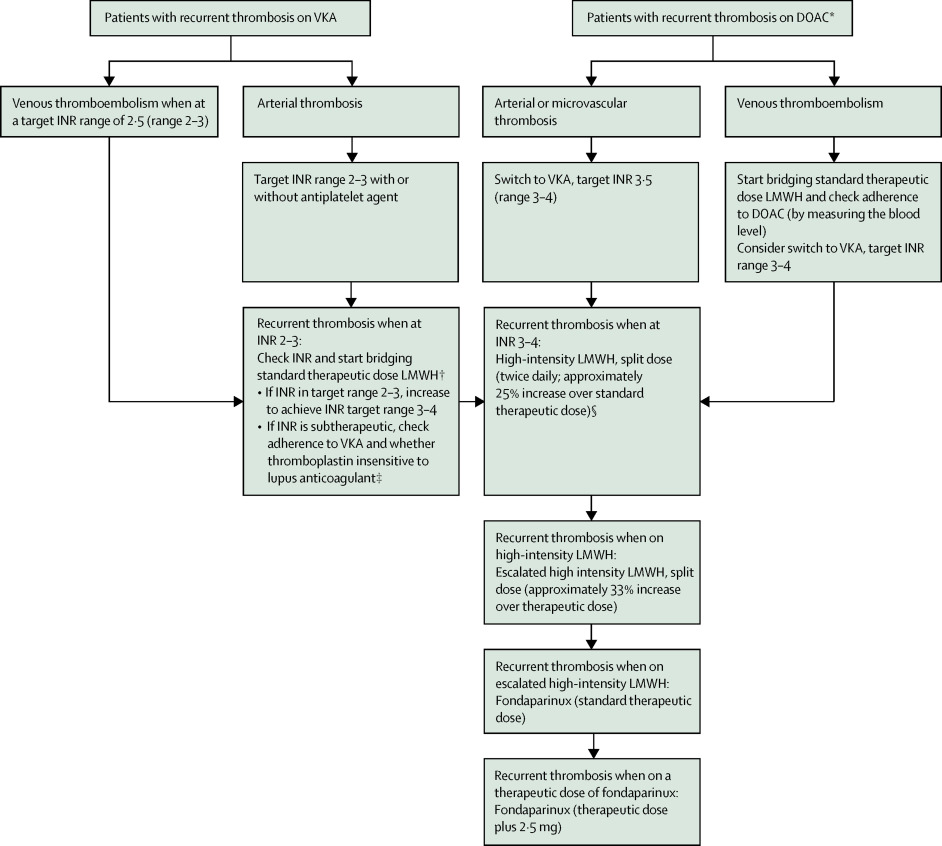
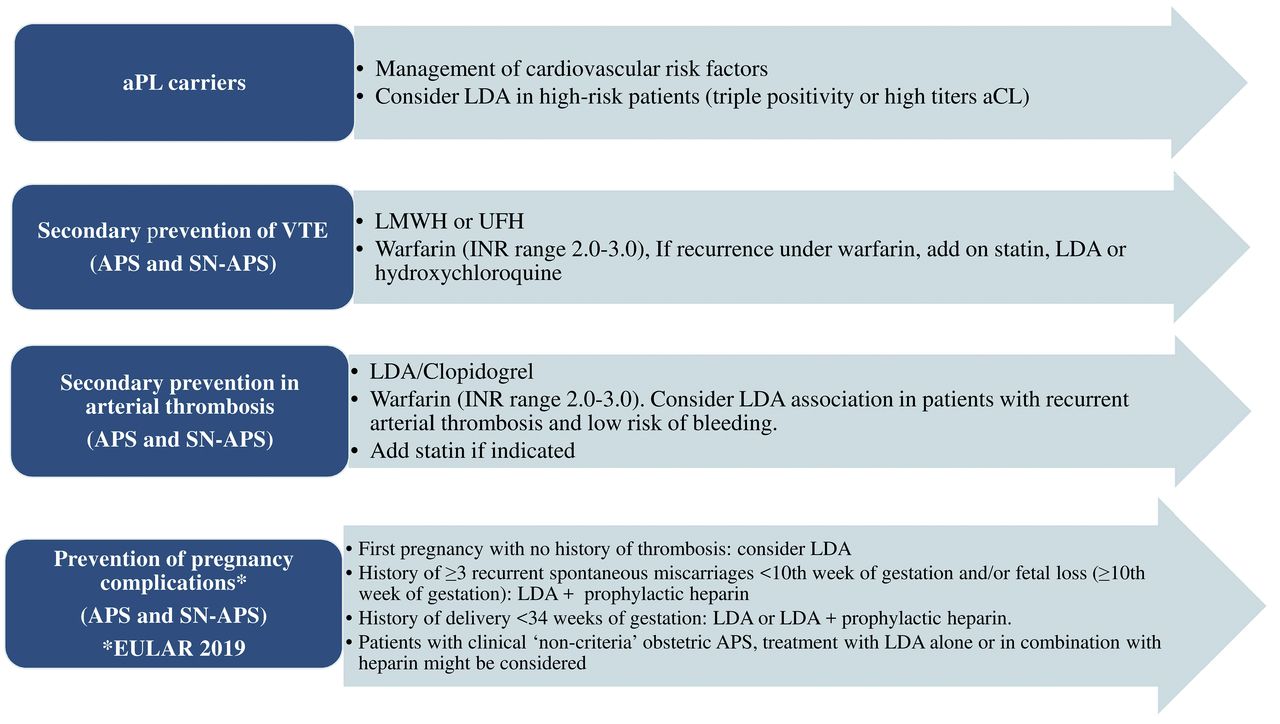
APS treatment
Not everyone who has abnormal antibodies will develop blood clots. But because blood clots can be very serious, if you have APS you will probably need to take medicine to thin your blood and reduce the chance of a clot.
The medicines most commonly used are heparin (an injection) and warfarin (a pill). Your doctor might also ask you to take a low dose of aspirin. Taking these medicines may increase your risk of bleeding, so your doctor will need to monitor you carefully.
You cannot take warfarin if you are pregnant. Your doctor will likely prescribe a certain type of heparin and low dose aspirin if you are pregnant to stop your blood from clotting and to maximise the chance of your carrying your baby to term. If you are planning on becoming pregnant, it is best to talk to your doctor first.
When to seek help
If you have been diagnosed with APS, see your doctor or seek emergency medical help if you have:
- pain, swelling, redness or tenderness in your arm or leg
- spotting or bleeding if you are pregnant
- numbness, weakness or paralysis in your face, arm or leg with speech or vision problems and dizziness (this could be a stroke)
- sudden shortness of breath, chest pain and coughing up mucus with blood in it (this could be a pulmonary embolism)
- unexplained bleeding from your nose or gums, a very heavy period, vomit with blood in it or black, tar-like faeces (poo)
Living with APS
If you have had a blood clot you are at higher risk than others of having another one. Taking your medicine will greatly lower the risk. You may have to stay on the medicine for the rest of your life, or until your doctor thinks the risks are greater than the benefits.
If you take blood-thinning medicine, you need to avoid injuring yourself or bleeding. You should:
- be very careful when using sharp tools or kitchen utensils
- avoid contact sports
- use a soft toothbrush
- use an electric razor
You should avoid developing a blood clot by:
- not smoking
- keeping at a healthy weight
- being physically active
Some foods, medicines and supplements can interfere with blood thinning medication. Ask your doctor what to avoid.